Renal oncocytoma accounts for 5–7% of primary renal neoplasms. It is usually diagnosed in asymptomatic patients and is characterized by a benign behavior without invasion of adjacent tissues or metastasis. Diagnosis during pregnancy is uncommon and to date there have been only a few cases reported in the literature.
Case reportThe authors present the case of a 32-year-old nulliparous woman with uncontrolled hypertension diagnosed at seven weeks gestation. She was referred to our institution at 24 weeks with superimposed pre-eclampsia complicated by acute pulmonary edema and hemodynamic instability requiring mechanical ventilatory support, fetal growth restriction and stillbirth. Etiological study of the hypertensive disorder performed in the postpartum period was consistent with renal oncocytoma.
ConclusionThe clinical behavior of renal oncocytoma remains poorly characterized during pregnancy and may lead to an adverse maternal and fetal outcome despite its theoretically benign behavior. It is essential to exclude a possible secondary cause of hypertension in cases that are difficult to control.
O oncocitoma renal representa 5–7% das neoplasias primárias do rim, é diagnosticado em doentes assintomáticos e caracteriza-se por um comportamento benigno, sem invasão dos tecidos adjacentes ou metastização. O seu diagnóstico no decurso da gravidez é raro, havendo poucos casos descritos na literatura.
Caso clínicoOs autores apresentam o caso de uma nulípara de 32 anos com hipertensão arterial de difícil controlo diagnosticada às sete semanas gestacionais com internamento às 24 semanas por quadro de hipertensão crónica agravada com pré-eclâmpsia sobreposta, edema agudo do pulmão e instabilidade hemodinâmica com necessidade de suporte ventilatório mecânico, restrição do crescimento fetal e morte fetal. O estudo etiológico do quadro hipertensivo efectuado no período pós-parto permitiu demonstrar a existencia de um tumor renal-oncocitoma.
ConclusãoO comportamento clínico do oncocitoma renal permanece mal caracterizado durante a gravidez, podendo associar-se, apesar do seu comportamento teoricamente benigno, a um desfecho materno e fetal adverso. É fundamental excluir uma possível causa secundária nos quadros hipertensivos de difícil controlo.
The authors report the case of a 32-year-old woman, white, with no relevant medical, surgical or obstetric history. The current pregnancy arose through medically assisted techniques due to primary infertility.
During the first half of the pregnancy, the patient developed hypertension that was difficult to control despite combined medical therapy with alpha-methyldopa 500mg every hours, propranolol 20mg every 8hours and nifedipine CR 30mg once a day.
At 24 weeks gestation, following further elevation of blood pressure (BP) (194/131mmHg), visual disturbances, proteinuria and worsening renal function, the patient was transferred to a hospital with specialist perinatal support services and admitted to a maternal–fetal intensive care unit. The clinical setting and laboratory tests confirmed chronic hypertension with superimposed pre-eclampsia; intravenous perfusion of labetalol and magnesium sulfate was therefore begun and betamethasone was administered for fetal pulmonary maturation according to the department's protocol. On the third day of hospital stay, the patient's clinical condition worsened despite therapy, and she developed ascites, limb edema, periorbital edema and other signs of volume overload. Laboratory tests revealed hypoalbuminemia and worsening renal function (Table 1). Fetal ultrasound showed a good biophysical profile (8/8), despite fetal growth restriction and absent end-diastolic flow; ductus venosus Doppler was normal, and regular fetal monitoring was instituted.
Maternal and fetal evolution in the maternal–fetal intensive care unit.
| Gestational age | Maternal syndrome | Fetal syndrome | Treatment |
| Day 124 weeks 5 days | BP 174/115mmHg, proteinuria and lower limb edemaLaboratory results: Hb 11.9mg/dl, leukocytes 13000/μl, platelets 287000/μl, urate 5.6mg/dl, creatinine 0.8mg/dl, AST 13, ALT 15, proteinuria 0.8g/dl | Betamethasone, magnesium sulfate, labetalol, nifedipine, methyldopa | |
| Day 325 weeks | Periorbital edema and ascitesLaboratory results: Hb 10mg/dl, leukocytes 17100/μl, platelets 246000/μl, urate 7.2mg/dl, creatinine 0.9mg/dl, AST 14, ALT 16, Mg2+ 5.6, proteinuria 0.4g/dl | Ultrasound:Pelvic presentation, estimated weight 587gFlowmetry:Absence of diastolic flow in UA, normal DV | Furosemide, labetalol, nifedipine, methyldopa, magnesium sulfate |
| Day 425 weeks 1 day | Dyspnea, bibasal crackling ralesLaboratory results: Hb 9.0g/dl, leukocytes 14900/μl, platelets 228000/μl, urate 8.1mg/dl, albumin 2.6g/dl, AST 20, ALT 19, proteinuria 1g/dl | Furosemide, labetalol, nifedipine, methyldopa, IDN, desalted human albumin | |
| Day 525 weeks 2 days | Dyspnea, bibasal crackling ralesLaboratory results: Hb 10.2 g/dl, leukocytes 16000/μl, platelets 246000/μl, urate 9.0mg/dl, creatinine 0.9mg/dl, albumin 2.9g/dl, proteinuria 1.5g/dl | Flowmetry:Reverse diastolic flow in UA, normal MCA | Furosemide, labetalol, nifedipine, methyldopa, IDN, desalted human albumin |
| Day 625 weeks 3 days | Acute pulmonary edema with hemodynamic instability (BP 160/110mmHg) | Fetal death | Invasive ventilation |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; BP: blood pressure; DV: ductus venosus; Hb: hemoglobin; IDN: isosorbide dinitrate; MCA: middle cerebral artery; Mg2+: magnesium; UA: umbilical artery.
On the fourth day of hospital stay, a diagnosis of acute pulmonary edema in the context of hypertensive crisis was made and appropriate therapeutic measures were taken. On the sixth day, there was further worsening of the mother's pulmonary status requiring invasive mechanical ventilation, followed by fetal death; the patient was transferred to a general intensive care unit. The fetus was stillborn two days later, and the patient's condition slowly improved.
A thorough etiological study was performed in the postpartum period, including renal and endocrine studies and investigation of hereditary and acquired thrombophilia.
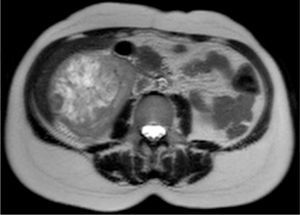
Renal ultrasound showed a well-defined mass in the lower pole of the right kidney. Renal magnetic resonance imaging was performed to clarify its nature and relations, which showed a well-defined, macronodular mass measuring 85mm at its widest point, with radial expression and a central necrotic scar with high contrast uptake, suggestive of renal oncocytoma (Figs. 1 and 2).
Total right nephrectomy was subsequently performed and the surgical specimen was sent for pathoanatomical and immunohistochemical study. This confirmed a solid tumor measuring 85×70×65mm, consisting of granular and eosinophilic cytoplasm, positive for Cam 5.2 and negative for CD10, and focally positive for CK7 and vimentin, compatible with a diagnosis of renal oncocytoma.
The patient's BP normalized in the postoperative period.
After two years of clinical surveillance, the patient became pregnant again. The second pregnancy was monitored from the first trimester at our institution and was uneventful, with normal BP. At 36 weeks, it was decided to perform a cesarean section due to abnormal fetal presentation and oligamnios, resulting in the birth of a healthy boy weighing 2165g, with an Apgar score of 7/10.
DiscussionRenal oncocytoma accounts for 5–7% of primary renal neoplasms. It is usually diagnosed in asymptomatic patients following diagnostic exams for non-urological reasons.1
On histopathological study, renal oncocytoma presents as a well-defined, solid mass in the renal parenchyma with a central sclerosed area, although it should be remembered that this classical finding is present in only a third of cases.1–3 Diagnosis therefore requires thorough histopathological study to document the presence of tumor cells arranged in nests, cords, or tubules, with eosinophilic cytoplasm and no mitosis, and exclude the coexistence of a clear-cell tumor, found in 10–32% of cases in the literature.2,4,5
This type of tumor usually has a benign behavior and excellent prognosis. Even large masses are encapsulated and as such are rarely invasive or associated with metastasis.5–8
Diagnosis of renal oncocytoma during pregnancy is uncommon. In 1989, Fraser et al.3 published the first case report of a renal tumor diagnosed at 23 weeks gestation following investigation of right lower back pain in a healthy 31-year-old woman. This case had a good perinatal outcome despite pre-eclampsia.
In the case presented here, the renal oncocytoma was diagnosed following investigation of the cause of hypertension detected in the first half of the pregnancy that was refractory to combined therapy, culminating in early onset of severe pre-eclampsia associated with acute pulmonary edema requiring invasive ventilation, followed by fetal death.
Pre-eclampsia is defined as hypertension (BP of over 140/90mmHg in two measurements at least 6h apart) and proteinuria of over 300mg/24h. It is a complex maternal–fetal syndrome of early onset that results from inadequate trophoblast invasion. The complications associated with this syndrome include acute renal failure, eclampsia, acute pulmonary edema, placental abruption fetal growth restriction and fetal death. Such manifestations or the development of pre-eclampsia at early gestational ages are taken by some authors as a criterion of severe disease that justifies thorough investigation of the underlying causes.
This case presented with hypertension before the 20th week of gestation that could not be controlled despite combined antihypertensive therapy, and was associated with significant maternal morbidity and fetal death. Thorough investigation to exclude a secondary cause led to a diagnosis of renal oncocytoma and resolution of the patient's hypertension.
ConclusionThe clinical behavior of renal oncocytoma remains poorly characterized during pregnancy and may lead to an adverse maternal and fetal outcome despite its theoretically benign behavior.
The authors highlight the importance of excluding a secondary cause of hypertension in cases that are difficult to control.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Torres, R. Oncocitoma renal na gravidez – uma forma invulgar de hipertensão secundária. Rev Port Cardiol 2012. doi:10.1016/j.repc.2011.08.002