Remote magnetic navigation has proved to be effective in the ablation of most supraventricular and ventricular arrhythmias. Initial studies reported worse results with this system compared to conventional ablation for atrial flutter. The aim of this study was to assess the acute and long-term success of atrial flutter ablation with remote magnetic navigation and to retrospectively compare the results obtained with an 8-mm tip catheter versus an irrigated catheter.
MethodsWe studied 38 consecutive patients, mean age 61±15 years, 28 male, who underwent ablation of typical atrial flutter with the Niobe II remote magnetic navigation system (Stereotaxis). Ablation was performed with an 8-mm tip catheter in 17 patients and with an irrigated-tip catheter in 21 patients. Acute success was defined as the presence of bidirectional isthmus block, and long-term success as absence of symptoms and atrial flutter during Holter monitoring.
ResultsBidirectional isthmus block was achieved in 37 patients (97%), and the success rate was similar in both groups. Total procedure time was not significantly different between the groups but fluoroscopy time was shorter in the irrigated tip group (13.4±3.7 min vs. 6±4.4 min; p<0.01). The number of applications and total radiofrequency time did not differ. There were no complications. During a follow-up of 32±19 months there were two relapses, one in each group.
ConclusionsThe Niobe II remote control system for ablation of typical atrial flutter is safe and effective in both the short and long term. The 8-mm and irrigated-tip catheters showed similar safety and efficacy.
A ablação com sistema de navegação magnética tem demonstrado ser eficaz em vários tipos de procedimentos de ablação. Estudos iniciais apontam para uma menor eficácia deste método na ablação do istmo cavo-tricúspide. O objetivo deste estudo foi avaliar a eficácia imediata e a longo prazo deste método e comparar retrospetivamente os resultados obtidos com o cateter de 8mm com os obtidos com o cateter irrigado.
MétodosEstudaram-se 38 doentes consecutivos, idade média 61±15 anos, 28 homens, referenciados para ablação de flutter típico com sistema de navegação magnética Niobe II (Stereotaxis) com um período de seguimento superior a seis meses. A ablação foi efetuada com cateter de 8mm em 17 doentes e com cateter irrigado em 21 doentes. O sucesso imediato foi definido como presença de bloqueio ístmico bidirecional e o sucesso a longo prazo definido com ausência de sintomas e de flutter auricular no registo de Holter.
ResultadosO bloqueio ístmico bidirecional foi obtido em 37 doentes (97%). A taxa de sucesso foi semelhante nos dois grupos. O tempo de procedimento não diferiu entre os dois grupos, mas o tempo de fluoroscopia foi significativamente inferior no grupo com cateter irrigado (13,4±3,7min versus 6±4,4min; p<0,01). O número de aplicações e o tempo de radiofrequência foram semelhantes nos dois grupos. Não foram registadas complicações. Após um período de seguimento médio de 32±19 meses ocorreram duas recidivas, uma em cada grupo.
ConclusõesO sistema de navegação magnética Niobe II mostrou-se eficaz e seguro na ablação de flutter típico permitindo uma taxa de sucesso elevada com uma eficácia mantida a longo prazo. O cateter de 8mm e o cateter irrigado mostraram-se igualmente eficazes e seguros.
atrial fibrillation
atrial flutter
coronary sinus
cavotricuspid isthmus
inferior vena cava
magnetic navigation system
radiofrequency
Atrial flutter (AFL) is an abnormal cardiac rhythm characterized by rapid regular atrial depolarizations with a rate of approximately 300/min and regular ventricular rate. Typical AFL is the most common macroreentrant atrial tachycardia.1 Catheter ablation of the cavotricuspid isthmus (CTI) is the treatment of choice for this arrhythmia due to its high success rate and low rate of complications compared to drug therapy, which is relatively ineffective.2
The Niobe magnetic navigation system (MNS) (Stereotaxis) was developed for remote control of ablation procedures, aimed at improving steering of the catheters and reducing fluoroscopy time. The system has been shown to be effective and safe in ablation of different types of supraventricular and ventricular arrhythmias, and is superior to conventional ablation for ventricular tachycardia.3,4 In a randomized trial of ablation of supraventricular tachycardias with the Niobe system compared to manual navigation, the MNS was associated with reduced fluoroscopy time and number of radiofrequency (RF) applications.5 However, initial studies of AFL ablation reported lower success rates than with manual steering,6–8 which may be due to the limited contact force possible with flexible catheters.
The aim of this study was to assess the feasibility and safety of the MNS for ablation of AFL and its long-term success and to compare the results obtained with an 8-mm tip catheter versus an irrigated catheter.
MethodsStudy populationBetween January 2008 and October 2012, 38 consecutive patients underwent electrophysiological study and catheter ablation of typical AFL with the Niobe MNS at our institution. AFL was documented by 12-lead ECG and the patients were symptomatic despite medication. No patient was contraindicated for magnetic navigation, and all gave their written informed consent.
Electrophysiological studyPatients were assessed after six hours’ fasting and antiarrhythmic medication was suspended for five half-lives; amiodarone was suspended at least one month before the procedure. Patients with persistent AFL who were not under oral anticoagulation underwent transesophageal echocardiography to exclude the presence of left atrial thrombi.
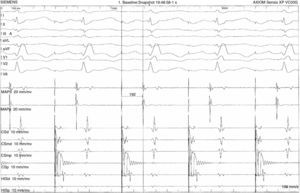
Surface electrocardiograms and intracavitary electrograms were recorded on an AXIOM Sensis system (Siemens Healthcare). Programmed stimulation was performed using a UHS 3000 heart stimulator (Biotronik). The catheters were inserted via the femoral vein and positioned under fluoroscopic guidance, a quadripolar catheter (Navistar, Biosense Webster) in the His bundle and an octapolar catheter (Dynamic XT, Bard) in the coronary sinus (CS).
When ablation was carried out in AFL rhythm, entrainment pacing was used to demonstrate the presence of isthmus-dependent atrial flutter. Patients in sinus rhythm underwent CS pacing to measure conduction time across the CTI before ablation.
Magnetic navigationAll procedures were carried out using the Niobe II system. The MNS has been previously described9; it basically consists of two computer-controlled magnets positioned on either side of the fluoroscopy table, which create a magnetic field (0.1 T). The position of the magnets is controlled from a console, the Navigant workstation, which orientates the magnetic field according to vectors selected by the operator. The ablation catheter has three magnets at its distal end, which orientate it parallel to the magnetic field. Changes in the orientation of the magnetic field deflect the catheter tip, which is advanced or withdrawn remotely by a motor at the proximal end of the catheter (Cardiodrive, Stereotaxis). Magnetic field vectors can be stored, enabling subsequent automatic navigation to previous sites.
Mapping and ablationThe MNS is integrated with a CARTO XP RMT (Biosense Webster) electroanatomical mapping system and provides real-time information on the position and orientation of the mapping catheter tip. This information is overlaid on the fluoroscopic images on the Navigant workstation, providing real-time monitoring of the catheter position without the need for further fluoroscopy (Figure 1). The location of the His bundle is marked on the screen of the CARTO workstation.
Reference fluoroscopic images on the Navigant workstation in right and left anterior oblique views showing the real-time position of the ablation catheter, without further fluoroscopy, in the cavotricuspid isthmus at the 5 o’clock position, the automatic vector of the magnetic navigation system (yellow arrow) and the His bundle (yellow point). OAD: right anterior oblique; OAE: left anterior oblique.
A Navistar RMT (Biosense Webster) catheter with an 8-mm tip was used for the first 17 procedures and a Navistar RMT Thermocool (Biosense Webster) irrigated-tip catheter for the subsequent 21 procedures. The ablation catheter was introduced via the femoral vein and advanced manually to the right atrium without the need for long sheaths, then remotely to the tricuspid annulus at the 6 o’clock position in left anterior oblique view and subsequently to the right ventricle, after which it was gradually withdrawn until an atrial potential was detected on the distal bipole of the ablation catheter. RF energy was then applied at this point and the ablation catheter was progressively withdrawn under remote control to the inferior vena cava (IVC).
The MNS vector was directed downward in the initial portion of the CTI and more anteriorly in the final portion, closer to the IVC (Figure 2). Using an EP Shuttle RF generator (Stockert), RF was applied between the distal electrode of the ablation catheter and a cutaneous patch electrode, with a power limit of 70 W and maximum temperature of 55°C in the case of the 8-mm catheter, and a power limit of 50 W and maximum temperature of 45°C with the irrigated catheter. The duration of RF application depended on the disappearance of the atrial potential on the distal electrogram, but was never less than 30 s. Light sedation with midazolam (bolus) or remifentanil (perfusion) was administered during RF application when necessary. Procedure and fluoroscopy times were recorded, procedure time being defined as the interval between venous puncture and removal of the introducer. Acute success was defined as demonstration of bidirectional block in the CTI and non-inducibility of AFL after 30 min. Bidirectional block was demonstrated by documentation of downward activation in the right atrial lateral wall during CS pacing and downward activation in the septum during low-lateral right atrial pacing, as well as a conduction delay across the isthmus. As previously described,10 the minimum conduction delay across the isthmus during CS pacing that demonstrates conduction block in the CTI was taken to be 110 ms (Figure 3).
If the initial ablation line did not result in CTI block, the line was mapped to detect possible gaps, and if CTI conduction persisted after any gaps were eliminated, additional lines were created in more lateral or septal positions. If bidirectional CTI block could not be achieved, the procedure was considered unsuccessful. All patients remained under surveillance in hospital for 24 hours after the procedure.
The results obtained with an 8-mm tip catheter were compared with those using an irrigated catheter.
Follow-upFollow-up consultations included clinical assessment between the first and third month after the procedure and then every six months. Holter 24-hour monitoring was performed between the third and sixth month and then at least once a year. Clinical success was defined as absence of palpitations and/or absence of AFL on ECG.
Statistical analysisData are presented as means ± standard deviation for continuous variables and as frequencies for categorical variables. Categorical variables were analyzed with the chi-square test and continuous variables with the Student's t test.
ResultsPopulationThirty-eight consecutive patients, mean age 61±15 years, 28 male, underwent ablation of typical AFL. Twenty-six had persistent AFL. Nineteen had hypertension, four had coronary disease and had undergone coronary artery bypass grafting, two had non-ischemic dilated cardiomyopathy, one had Ebstein's anomaly and 12 had no structural heart disease. The baseline characteristics of the two groups (those treated by 8-mm tip catheter and by irrigated catheter) are presented in Table 1. There were no significant differences between the groups.
Characteristics of the study population.
| 8-mm tip catheter | Irrigated catheter | p | |
| n | 17 | 21 | NS |
| Age (years) | 65±9 | 58±18 | NS |
| Male | 71% | 76% | NS |
| Persistent AFL | 82% | 57% | NS |
| RA dilatation | 81% | 73% | NS |
| LVH | 30% | 23% | NS |
| Isolated AFL | 6 | 6 | NS |
| Medication | |||
| Oral anticoagulation | 11 | 13 | NS |
| Amiodarone | 3 | 6 | NS |
| Propafenone | 1 | 1 | NS |
| Flecainide | 1 | 2 | NS |
| Beta-blockers | 6 | 8 | NS |
AFL: atrial flutter; LVH: left ventricular hypertrophy; RA: right atrial.
Ablation was carried out in AFL rhythm in 31 patients and in sinus rhythm in seven. The procedure was successful in 37 patients (97%). FLA was terminated during the procedure in 30 cases.
Procedure time was 167±59 min and fluoroscopy time was 7.8±5.3 min. The mean number of RF applications was 22±15, with a mean application time of 24±13 min.
The ablation procedure characteristics in the study population are presented in Table 2. The success rate was similar in both groups, 94% in the 8-mm tip catheter group and 100% in the irrigated catheter group, as was procedure time, but fluoroscopy time was significantly shorter in the irrigated catheter group (13.4±3.7 vs. 6±4.4 min; p<0.01). The number of RF applications and total RF application time did not differ significantly between the groups.
Ablation procedure characteristics.
| 8-mm tip catheter | Irrigated catheter | p | |
| AFL during ablation | 14 | 17 | NS |
| Procedure time (min) | 189±61 | 151±71 | 0.09 |
| Fluoroscopy time (min) | 13.4±3.7 | 6±4.4 | 0.01 |
| No. of RF applications | 22±15 | 21±14,8 | NS |
| RF application time (min) | 25±15 | 24±13 | NS |
| Success | 16/17 | 21/21 | NS |
AFL: atrial flutter; RF: radiofrequency energy.
There were no procedure-related complications.
During a follow-up of 32±19 months (6–60) two patients had relapse of AFL, one in each group (Table 3). One patient refused reablation and in the other the procedure was repeated with an irrigated catheter, which was successful. Six patients developed atrial fibrillation (AF) during follow-up that was treated by ablation. After pulmonary vein isolation, conduction across the CTI was assessed and continuing bidirectional block was confirmed in all patients.
There were no deaths during follow-up.
DiscussionThe main finding of this study was that the Niobe II MNS is safe and effective for treatment of AFL, with similar success rates to conventional ablation.11 We also found that 8-mm tip and irrigated catheters are equally effective, which is in agreement with previous studies comparing these two types of catheter for AFL ablation.12–14
Linear CTI ablation, first described by Cosio et al.,15 is the first-line strategy for treatment of typical AFL. The first procedures used a 4-mm tip catheter, but success rates were as low as 67% in some series.16 Efforts to improve these figures included the development of 8-mm tip catheters and then irrigated-tip catheters designed to increase the size of lesions, improving success rates, which in some cases have reached 99%.12,14,16,17 The high success rates of AFL ablation, together with the poor results of drug therapy,2 have led to catheter CTI ablation becoming a common procedure.
Previous studies comparing conventional AFL ablation with remote navigation-controlled systems showed that the latter produced worse results (91% vs. 84%).7
In our study, the success rates with the MNS of 94% using an 8-mm tip catheter and 100% with an irrigated catheter are higher than those described with conventional systems.11 Previous studies have also shown that procedure time and RF time tend to be longer with the MNS but fluoroscopy time is significantly shorter.7,8 Mean fluoroscopy time in our series (7.8±5.3 min) was also significantly shorter than reported for conventional ablation.12,14,16,17 The longer fluoroscopy time seen in the 8-mm tip catheter group may be due to the greater difficulty in adjusting the larger tip to the anatomy of the CTI, but may also be the result of the learning curve associated with the MNS, since the first cases using the remote system were treated with an 8-mm tip catheter. Randomized trials comparing the two catheter types have shown similar success and complication rates as well as procedure and fluoroscopy times.12,15
Our long-term success rate (5% relapse at 32±19 months) was better than that described for conventional ablation, well below the 10.9% at 13.8±0.3 months of Perez et al.11 and the 20% at 21±11 months reported by Blomstrom-Lundqvist et al.2 Although we did not assess coagulum formation on the catheter tip in our study, most studies show a tendency for higher prevalence of this complication with 8-mm tip catheters than with irrigated catheters (between 6% and 15%).8,12 For this reason, notwithstanding the good results obtained with the 8-mm tip catheter, the irrigated catheter has been our choice for AFL ablation since it became available for the MNS.
The occurrence of AF following ablation of AFL, although not strictly speaking a relapse of the initial arrhythmia, is a cause of morbidity and hospitalization. The incidence of AF after AFL ablation depends on whether it had occurred before the procedure and on the duration of follow-up, and ranges between 8 and 52%.10 In our patient population the incidence of AF was 16% in a mean follow-up of 32±19 months; the figure was higher in the 8-mm tip catheter group, but without statistical significance, and may be due to the longer follow-up in this group.
LimitationsThe present study was not randomized and included a small number of patients, and no comparison was made with conventional ablation in terms of procedure or fluoroscopy times or efficacy. The comparison between the two different catheter types was performed retrospectively.
ConclusionsOur study demonstrates that the remote control Niobe II system is safe and effective for AFL ablation, with a high rate of acute success and a low rate of relapse. Irrigated catheters and 8-mm tip catheters were equally effective and safe for the ablation of typical AFL using the MNS.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Parreira L, Cavaco D, Carmo P, et al. Ablação do istmo cavo-tricúspide com sistema de navegação magnética por controlo remoto no tratamento do flutter auricular típico – resultados a longo prazo. Rev Port Cardiol. 2014;33:773–779.