The aim of this study was to assess the effectiveness of atrial antitachycardia pacing (ATP) in the conversion of atrial tachyarrhythmia episodes, and its impact in reducing arrhythmic burden.
MethodsWe performed a retrospective study in the pacing laboratory of a district hospital of 57 consecutive patients implanted with a dual chamber pacemaker, capable of performing atrial antitachycardia pacing, between 2005 and 2010. The patients were divided into two groups: ATP_ON (n=24) and ATP_OFF (n=33). The follow-up period was 15 months, with data being collected at three follow-up consultations: the first at three months after implantation, the second at nine months and the last at 15 months. In this period, there were 12 428 ATP therapies of atrial tachyarrhythmias.
ResultsAlthough there were no statistically significant differences, there was a trend in favor of the ATP_ON group, the increase in arrhythmic burden being less marked in this group. The mean percentage of ventricular apical pacing was also significantly lower in this group, which was associated with a marginally significant reduction in arrhythmic burden (p=0.06). There was a significant positive correlation between changes in the percentage of ventricular pacing and changes in arrhythmic burden (r=0.417, p=0.02).
ConclusionsAtrial antitachycardia pacing converted 59.7% of episodes of atrial arrhythmia, but did not significantly reduce arrhythmic burden. There was a significant positive correlation between changes in the percentage of ventricular pacing and changes in arrhythmic burden.
O objetivo do estudo foi avaliar a eficácia do pacing auricular antitaquicardia (ATP) na conversão de episódios de taquiarritmia auricular e seu impacto na redução da carga arrítmica.
MétodosEstudo retrospetivo que decorreu no laboratório de pacing num hospital distrital, incluindo consecutivamente 57 doentes que implantaram pacemaker dupla câmara, com capacidade de realizar pacing auricular antitaquicardia, entre 2005-2010. Formaram-se dois grupos, grupo ATP_ON constituído por 24 doentes e grupo ATP_OFF constituído por 33 doentes. O período de seguimento foi de 15 meses, tendo-se recolhido os dados das consultas de seguimento de pacing realizadas em três momentos distintos, o primeiro ao 3.° mês após o implante (M1), o segundo ao 9.° mês (M2) e o último ao 15.° mês (M3), incluindo este período, tentativa de tratamento por ATP de 12.428 episódios de taquiarritmias auriculares.
ResultadosApesar de não ocorrerem diferenças estatisticamente significativas, verificou-se uma tendência favorável ao grupo ATP_ON, visto que, o aumento de carga arrítmica foi menos acentuado neste grupo. Também neste grupo se verificou percentagem média de pacing ventricular apical significativamente inferior, associando-se este parâmetro a redução marginalmente significativa da carga arrítmica (p=0,06). Verificou-se uma relação significativamente positiva entre a evolução da percentagem de pacing ventricular e a evolução da carga arrítmica (R=0,417, p=0,02).
ConclusõesO pacing auricular antitaquicardia converteu 59,7% dos episódios de arritmia auricular, mas não reduziu significativamente a carga arrítmica. Verificou-se correlação significativamente positiva entre a evolução da percentagem de pacing ventricular e a evolução da carga arrítmica.
Atrial fibrillation (AF) is one of the most common cardiac arrhythmias, affecting 1% of the general population and almost 10% of those aged over 80.1,2 Clinical management focuses on prevention of stroke and is based on anticoagulation therapy and ventricular rhythm and/or rate control.
Atrial antitachycardia pacing (ATP) is a therapeutic option for rhythm control in patients with permanent pacemakers that have this feature. The usual form, in which pacing is faster than the atrial rate, consists of the administration of a number of pulses of fixed duration (Burst pacing), or sequences at progressively shorter intervals (Ramp pacing), that are designed to abort episodes of AF or atrial flutter (AFL). The aim is to reduce atrial remodeling and the development of tachycardiomyopathy as well as to shorten the duration of the episode and reduce arrhythmic burden, which is a risk factor for stroke.3–5
The efficacy of ATP is influenced by tachycardia cycle length and regularity, but some more rapid and irregular rhythms can be converted by ATP, including AF, which can be initially regular.6 Multiple transitions in cycle length and regularity may occur over the course of a long arrhythmic episode, and ATP is more effective for the treatment of AFL and slow organized atrial tachycardia (AT).7,8 In a study by Gillis et al. of 71 patients over a three-year follow-up, neither ATP therapy alone nor combined atrial ATP and atrial pace prevention significantly reduced time in AT/AF.9
In a study by Vollmann et al. of 22 patients in whom ATP was delivered for 10 026 AT episodes, success rates were higher during immediate than during delayed ATP (59±7% vs. 22±5%, p<0.01), but this greater efficacy did not translate into a significant reduction in arrhythmic burden.10 In the PITAGORA trial comparing Ramp and Burst+ pacing in 176 patients, Ramp was more effective in terminating AT episodes (53.1 vs. 44.3%, p<0.001) for a cycle length of >240 ms, this advantage being explained by the theory of pacing for the termination of AT with a presumed reentry mechanism, and also because Ramp pacing delivers a larger number of differently coupled pulses within each sequence and thus has a greater chance of capturing the atrium.11 Improved quality of life has also been shown in patients with ATP efficacy >60%.12
Optimization of atrial ATP therapy may reduce the duration of AT episodes and contribute to the prevention of cardioembolic events. Nevertheless, anticoagulation should be maintained in patients with thromboembolic risk factors.11
The potential benefit of ATP therapy, which is now available in various models of conventional pacemakers, needs to be demonstrated in clinical practice. The aim of this study was to assess the effectiveness of atrial ATP in reducing arrhythmic burden and to identify predictors of success for ATP algorithms, in order to optimize their use.
MethodsWe performed a retrospective study in the pacing laboratory of a district hospital of consecutive patients implanted with a dual chamber pacemaker (EnRhythm P1501DR, Medtronic Inc., Minneapolis, MN, USA), between January 2005 and December 2010. The study population consisted of 57 patients, 28 male and 29 female, with a mean follow-up of 15 months. The ATP algorithm was activated at one month after implantation in nine patients and at three months in a further 15 patients, while in the others (n=33) ATP pacing remained switched off until the end of follow-up. The patients were thus divided into two groups: those with ATP pacing switched on (ATP_ON) and those with the algorithm switched off (ATP_OFF). The decision whether to activate ATP pacing was taken on the basis of the occurrence of atrial arrhythmias during follow-up, the algorithm being switched on in patients with arrhythmic burden >0.1%. The managed ventricular pacing (MVP) function, designed to minimize ventricular pacing, was switched off in one patient in the ATP_ON group and in seven patients in the ATP_OFF group (p=0.183). Table 1 summarizes the baseline clinical characteristics of the study population; no significant differences were seen between the two groups in terms of age, gender, cardiovascular risk factors, previous events, or current medication. The indication for pacemaker implantation was sinus node disease in 80.7% (n=46) and atrioventricular block (second-degree in 5.3%, n=3; third-degree in 14.0%, n=8) in the remainder, with no significant difference between the groups. Previous AF or AFL was documented in 45 patients (78.9%), with no significant difference between ATP_ON and ATP_OFF (p=0.97).
Baseline clinical characteristics of the study population.
| Total (n=57) | ATP_OFF (n=33) | ATP_ON (n=24) | p (between groups) | |
| Age, years (mean ± SD) | 73.05±9.11 | 73.61±8.99 | 72.29±9.44 | 0.60 |
| Gender | ||||
| Male, % (n) | 49.1 (28) | 42.4 (14) | 58.3 (14) | 0.29 |
| Female, % (n) | 50.9 (29) | 57.6 (19) | 41.7 (10) | |
| Hypertension | ||||
| No, % (n) | 10.5 (6) | 9.1 (3) | 12.5 (3) | 0.68 |
| Yes, % (n) | 89.5 (51) | 90.9 (30) | 87.5 (21) | |
| Dyslipidemia | ||||
| No, % (n) | 47.4 (27) | 51.5 (17) | 41.7 (10) | 0.59 |
| Yes, % (n) | 52.6 (30) | 48.5 (16) | 58.3 (14) | |
| Diabetes | ||||
| No, % (n) | 78.9 (45) | 81.8 (27) | 75.0 (18) | 0.74 |
| Yes, % (n) | 21.1 (12) | 18.2 (6) | 25.0 (6) | |
| CHF | ||||
| No, % (n) | 77.2 (44) | 72.7 (24) | 83.3 (20) | 0.52 |
| Yes, % (n) | 13 (22.8) | 27.3 (9) | 16.7 (4) | |
| CRF | ||||
| No, % (n) | 86.0 (49) | 84.8 (28) | 87.5 (21) | 0.78 |
| Yes, % (n) | 14.0 (8) | 15.2 (5) | 12.5 (3) | |
| Stroke | ||||
| No, % (n) | 93.0 (53) | 93.9 (31) | 91.7 (22) | 0.74 |
| Yes, % (n) | 7.0 (4) | 6.1 (2) | 8.3 (2) | |
| AF/paroxysmal AFL | ||||
| No, % (n) | 21.1 (12) | 21.2 (7) | 20.8 (3) | 0.97 |
| Yes, % (n) | 78.9 (45) | 78.8 (26) | 79.2 (19) | |
AF: atrial fibrillation; AFL: atrial flutter; ATP: antitachycardia pacing; CHF: congestive heart failure; CRF: chronic renal failure; SD: standard deviation.
Patients were selected on the basis of the model of pacemaker implanted. All information in their medical records and from follow-up consultations in the pacing laboratory was collected, as were pacemaker data from the pacing consultations via the Medtronic CareLink 2090 programmer with the model 2067 programming head. Percentages of successful ATP therapies, arrhythmic burden and atrial and ventricular pacing, number of episodes with attempted therapies, and number of successfully treated episodes were recorded. Data were collected retrospectively at three months (time point 1 – T1), nine months (T2) and 15 months (T3) after implantation.
Statistical analysisSPSS for Windows version 19.0 was used for the statistical analysis. The normality of the distribution of variables was assessed with the Kolmogorov-Smirnov test and the homogeneity of variance by Levene's test. Simple descriptive statistics was used to characterize the sample and the distribution of variables.
Groups were compared using the chi-square test for categorical variables and the Student's t test for two groups for quantitative variables. Repeated measures ANOVA was also used for the parameters assessed at different time points. When violations of sphericity were detected the Greenhouse–Geisser correction for degrees of freedom was applied. Bonferroni's correction for levels of significance was applied to all comparisons intended to identify the effects of a given factor. Frequent simple linear regression analyses were performed, complemented by multiple linear regression analysis. A value of p≤0.05 was used to determine statistical significance for a 95% confidence interval.
ResultsThe atrial lead was positioned in the right atrial appendage and the ventricular lead in the right ventricular (RV) apex in all patients. There were a total of 12 428 ATP therapies for episodes of AF/AFL, the arrhythmia being terminated in 7420 cases (estimated efficacy of 57.9% at 15 months). Data at the three different follow-up consultations were as follows: twenty-nine patients (50.9%) had received ATP therapies at T1, 32 (56.1%) at T2 and 36 (63.2%) at T3. There were no statistically significant differences between the groups. At T1, with nine patients having the ATP algorithm activated, there were 1019 attempted therapies, which were successful in 604 cases (59.3% efficacy); at T2, of 5458 episodes recorded, 3019 were treated successfully (55.3% efficacy); and at T3 there had been 5951 episodes, 3797 being treated successfully (63.8% efficacy). The variation in efficacy between the three follow-up consultations was not statistically significant (p=0.638), indicating that atrial ATP efficacy is relatively stable over time.
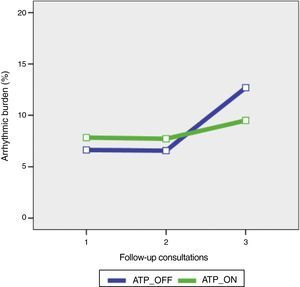
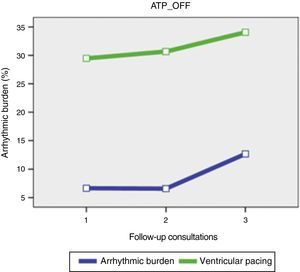
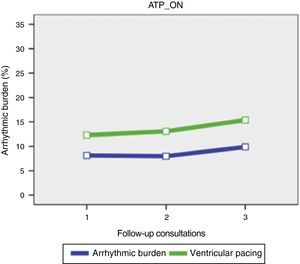
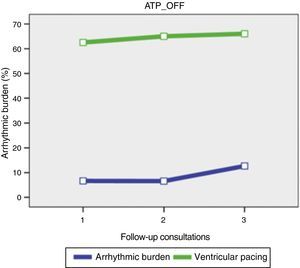
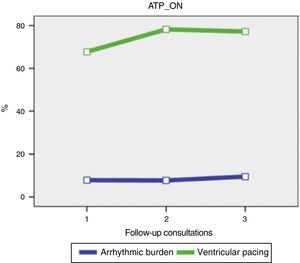
Mean arrhythmic burden was 6.64% in the ATP_OFF group and 7.51% in the ATP_ON group (p=0.845) at T1, 6.57% in the ATP_OFF group and 7.39% in the ATP_ON group at T2 (p=0.867), and 12.68% in the ATP_OFF group and 9.5% in the ATP_ON group at T3 (p=0.653). Although there were no statistically significant differences, there was a trend in favor of the ATP_ON group, the increase in arrhythmic burden being less marked in this group (Figure 1).
To determine whether the use of additional algorithms for prevention of atrial tachyarrhythmias increased the benefit of atrial ATP, the groups were divided into subgroups according to the presence or absence of preventive algorithms for AF. Analysis of the results (Figure 2) shows that the group with the ATP algorithm alone presented the lowest arrhythmic burden at the end of follow-up (15 months) and was also the group in which the increase in arrhythmic burden was smallest, although without statistical significance (p=0.967).
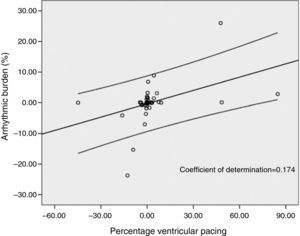
There was a positive and statistically significant correlation between changes in the percentage of ventricular pacing and changes in atrial arrhythmic burden (r=0.417, p=0.02), indicating that an increase in ventricular pacing is reflected in a significant increase in arrhythmic burden (coefficient of determination 0.174) (Figure 3).
The mean percentage of ventricular pacing was 29.47% in ATP_OFF and 11.34% in ATP_ON at T1 (p=0.024), 30.67% in ATP_OFF and 12.5% in ATP_ON at T2 (p=0.038), and 34.07% in ATP_OFF and 14.73% in ATP_ON at T3 (p=0.037) (Figures 4 and 5). The ATP_OFF group thus presented a significantly higher percentage of apical ventricular pacing than the ATP_ON group at all three follow-up time points.
Comparison of the two groups in terms of the relation between percentage of ventricular pacing and variation in arrhythmic burden revealed a marginally significant association (p=0.06), indicating that ventricular pacing is an independent determining factor in atrial arrhythmic burden.
The mean percentage of atrial pacing was 62.53% in ATP_OFF and 68.63% in ATP_ON at T1 (p=0.46), 65.02% in ATP_OFF and 78.22% in ATP_ON at T2 (p=0.09), and 66.05% in ATP_OFF and 77.2% in ATP_ON at T3 (p=0.22). There were thus no statistically significant differences between the groups (Figures 6 and 7) and no significant association between atrial pacing, arrhythmic burden and ATP (p=0.372), unlike the results for ventricular pacing.
Regarding major clinical events during follow-up, two cases of stroke and one of acute renal failure were observed in the ATP_OFF group and one death from cancer in the ATP_ON group.
DiscussionSome previous studies have demonstrated that atrial ATP therapy is a valid and safe option for rhythm control in patients with symptomatic bradycardia requiring pacing and can terminate 40–60% of atrial arrhythmias.7,11,13,14 In our study mean success rates with atrial ATP were slightly over 50% and no complications were recorded. However, other studies have shown that atrial ATP, either alone or combined with prevention algorithms, does not prevent or even significantly reduce arrhythmic burden.9,15 This was also observed in our study, even when different programming combinations were compared, notwithstanding a trend for a less marked increase in arrhythmic burden in the ATP_ON group without preventive pacing.
Analysis of the literature makes it clear that the evidence for the benefit of ATP therapy is inconsistent, largely due to the considerable heterogeneity in individual response, which means that the therapy will not be beneficial in a wide range of patients. Studies have shown that ATP is at best moderately effective in converting slow regular atrial tachycardias, less effective with rapid atrial tachycardias, and ineffective at treating established AF, and therefore cannot be considered the first-line treatment for paroxysmal AF.12,14–16
In the Atrial Therapy Efficacy and Safety Trial (ATTEST)16 of 324 patients, it was suggested that the high proportion of ventricular pacing (median=99%) may have exerted a deleterious effect and limited any benefit from the atrial therapies. This is partly supported by our results, although the effect was not so marked, which may be explained by the use of the MVP function, resulting in lower percentages of ventricular pacing in both groups (ATP_ON and ATP_OFF) than in ATTEST.
However, we found that changes in arrhythmic burden were significantly different in the ATP_ON group, in which the increase in arrhythmic burden was less marked. It is noteworthy that this group also presented a significantly lower mean percentage of ventricular pacing. Previous studies have shown that in patients with sinus node disease and intact atrioventricular conduction, high percentages (>40%) of ventricular pacing significantly increase the risk of AF and hospitalization for heart failure; in our study there was a significant positive correlation between changes in the percentage of ventricular pacing and changes in arrhythmic burden.17,18
Nevertheless, even with the lower frequency of apical RV pacing in the ATP_ON group, arrhythmic burden increased over the course of follow-up, which supports the idea that the ventricular dyssynchrony caused by ventricular pacing is deleterious. However, it does not significantly affect the performance of the algorithm, and is probably not the only risk factor for the development of atrial arrhythmias in these patients.
In addition, there is evidence that success rates are higher with immediate than with delayed ATP (59±7% vs. 22±5%, p<0.01), although this does not translate into a reduction of arrhythmic burden or related symptoms.10 In our series, the parameter “Episode duration before RX delivery” was nominally programmed for the therapy to be administered after 1 min than immediately after the beginning of the episode. The extent to which this may have negatively affected the efficacy of atrial ATP remains to be seen, which constitutes a limitation of the study.
There is also evidence that the position of the atrial lead is crucial to optimal ATP performance, with interatrial septal position being clearly superior to the conventional position.19–21 The fact that in all our patients the lead was positioned in the right atrial appendage means that the overall performance of the algorithm may have been sub-optimal.
LimitationsThe study included an insufficient number of patients with atrial ATP switched on to assess differences in comorbidities, hospitalization and mortality. Its retrospective nature is also a limitation, particularly with regard to the impact of percentage of atrial pacing on arrhythmic burden, since no statistically significant differences were found between the groups and so no association could be established.
The duration of follow-up is another limitation, since although it was longer than in most studies on this subject, a significantly longer follow-up would probably strengthen the tendency seen in the ATP_ON group for lower arrhythmic burden.
ConclusionsAtrial ATP was safe and effective in converting episodes of atrial tachyarrhythmias in this population and with the devices used in this study. However, it did not significantly reduce clinical events or arrhythmic burden. There was a significant positive correlation between changes in the percentage of ventricular pacing and changes in arrhythmic burden, and apical RV pacing had a deleterious effect, significantly increasing arrhythmic load.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Silva R, Pereira T, Martins V. Eficácia das terapias de pacing auricular antitaquicardia no tratamento da fibrilhação auricular paroxística em doentes portadores de pacemaker. Rev Port Cardiol. 2014;33:781–788.