Cardiovascular (CV) disease is the leading cause of death in Portugal. The prevalence of hypertension, the second most important risk factor accounting for overall disability-adjusted life years (DALYs), is significant. Hypertension rarely occurs in isolation, but is usually associated with other determining risk factors that contribute to greater overall CV risk. The main objective of the PRECISE study, a cross-sectional epidemiological study, was to determine the prevalence of other concomitant modulating CV risk factors in hypertensive patients.
MethodsThe prevalence of other CV risk factors and target organ damage was assessed in 2848 hypertensive patients of both sexes followed in primary health care centers. Demographic, anthropometric and clinical data and antihypertensive and lipid-lowering therapies prescribed were collected.
ResultsOf the study population (mean age 65.8±11.0 years, 60.8% women), 98.0% were treated for hypertension, but only 56.7% had controlled blood pressure. Hypercholesterolemia was the most frequent concomitant CV risk factor (82.1%), followed by sedentary behavior (71.4%). Prevalences of concomitant modulating risk factors were significantly different between the sexes and age groups. Overall, 81.7% of hypertensive patients had three or more concomitant CV risk factors.
ConclusionsThe study showed that, in Portugal, hypertensive patients have a high prevalence of other CV risk factors, confirming the need to identify these factors, calculate overall CV risk and continuously monitor the care provided and the results obtained.
A doença cardiovascular (CV) continua a ser a primeira causa de morte em Portugal. Com uma prevalência significativa, a hipertensão arterial (HTA) é o segundo fator de risco a concorrer para o total de anos de vida saudável perdidos (DALY). Raramente isolada, está, habitualmente, associada a outros elementos determinantes de risco, que contribuem para um maior risco CV global. O Precise, um estudo epidemiológico e transversal, teve como objetivo principal a avaliação da prevalência em doentes hipertensos de outros fatores concomitantes modeladores do risco CV.
MétodosNuma população de 2848 hipertensos, de ambos os géneros, acompanhados nos Cuidados de Saúde Primários avaliou-se a prevalência de outros fatores de risco CV e outras lesões de órgão alvo e caracterizaram-se aspetos demográficos, antropométricos e clínicos, assim como a terapêutica anti-hipertensora e antidislipidémica prescrita.
ResultadosCom uma média de idade de 65,8 ± 11,0 anos (60,8% mulheres), 98,0% estavam medicados para a HTA, mas só 56,7% tinham a pressão arterial controlada. A hipercolesterolemia foi o fator de risco CV mais frequente (82,1%), seguido pelo sedentarismo (71,4%). A prevalência dos diversos modeladores de risco foi significativamente diferente entre os géneros e grupos etários. Globalmente, 81,7% dos hipertensos apresentavam três ou mais fatores de risco CV concomitantes.
ConclusõesO estudo atestou que, em Portugal, os doentes com HTA têm uma prevalência elevada de outros fatores de risco CV, confirmado a necessidade de identificar os diversos fatores de risco, calcular o risco CV global e a monitorar continuamente dos cuidados prestados e dos resultados obtidos.
According to the INTERHEART and INTERSTROKE studies, hypertension is the cause of 37% of all strokes and of 18% of cases of myocardial infarction (MI) worldwide.1 Hypertensive heart disease, aortic stenosis, arterial stiffness, and to some extent aortic syndromes and obstructive peripheral arterial disease (PAD) also result from hypertension and its clinical manifestations, which include cardiac dysfunction and heart failure, angina, arrhythmias (particularly atrial fibrillation), intermittent claudication and acute lower limb ischemia. Furthermore, hypertension is a risk factor for cognitive decline and dementia, chronic kidney disease, erectile dysfunction, and possibly age-related macular degeneration.2
Hypertension increases the risk of target organ damage (TOD), maternal and fetal morbidity and overall mortality. Increased blood pressure (BP) is strongly and directly related to cardiovascular (CV) morbidity and mortality, without any evidence of a threshold down to at least 115/75 mmHg; each difference of 10 mmHg in diastolic blood pressure (DBP) or 20 mmHg in systolic blood pressure (SBP) doubles CV risk.3 Baseline CV risk, in conjunction with elevated BP, increases with every decade of life, and is thus higher in hypertensives, whose initial absolute risk is greater.
The NCD Risk Factor Collaboration estimates that the number of adults with elevated BP (≥140/90 mmHg) increased from 594 million to 1.13 billion in 2015, with higher prevalences in low-income and middle-income countries, largely due to aging populations.4 The prevalence of hypertension in Portugal was 42.2% in 2014,5 a similar figure to 2003.6 According to the Global Burden of Disease Study,7 high SBP was the condition responsible for the most disability-adjusted life years (DALYs) in 2015 (in third place in 1990). DALYs are a measure of the impact of a disease over time, which combines years lived with disability and years of life lost.8 The most recent data on the Portuguese population show that hypertension is the second leading factor after poor diet accounting for overall DALYs (13% and 16%, respectively).9
Part of the burden of hypertensive disease is due to the coexistence of other risk factors (such as dyslipidemia, which is more frequent in hypertensives than in those with normal BP) that increase overall CV risk and lead to atherosclerotic CV events. This association means that coexisting risk factors require a combined and complementary approach, which will determine the type and intensity of treatment.10,11 Hypertension in fact rarely occurs in isolation; 40% of coronary events in men and 68% of those in women are estimated to result from two or more CV risk factors.12 In the Framingham Heart Study, isolated hypertension was observed in less than 10% of subjects, while it was accompanied by other CV risk factors such as dyslipidemia, abdominal obesity and diabetes in over 50%. This epidemiological study also demonstrated the relationship of DBP (more often studied than SBP at that time) with coronary artery disease (CAD), stratified by total cholesterol (TC) levels, showing a more significant increase in risk in individuals with higher TC.12–14
There are few if any epidemiological data on the situation in Portugal concerning this issue. It is often stated that hypertensive patients seen in hospital outpatient consultations are not representative of the general population with hypertension, since most hypertensive individuals are followed in primary health care centers (PHCCs). In this context, the present study was designed to assess the prevalence of other CV risk factors and the main types of TOD in patients diagnosed with hypertension followed in PHCCs. This retrospective study aimed to illustrate real-world practice concerning hypertensive patients in Portugal, stratified by gender, age and region.
MethodsObjectivesThe PRECISE study (PREvalence of Cardiovascular RIsk FactorS in patiEnts with high BP in Portuguese primary health care centers), a cross-sectional epidemiological study, included individuals of both genders resident in Portugal, diagnosed with hypertension and followed in PHCCs. The main objective was to determine the percentage of patients with hypertension who presented other concomitant modulating CV risk factors and certain types of TOD associated with hypertension, particularly left ventricular hypertrophy (LVH) and proteinuria. The secondary objectives were to establish the prevalence of CV risk factors (smoking, hypercholesterolemia, obesity, type 2 diabetes, sedentary behavior, family history of CAD, personal history of PAD, stroke or CAD, LVH by electrocardiogram [ECG-LVH], and microalbuminuria/proteinuria), stratified by gender and age; to determine the percentage of patients with treated and controlled hypertension and thus to estimate this percentage for the overall Portuguese population; and to stratify patients according to CV risk using the Systematic COronary Risk Evaluation (SCORE) system15 and the Framingham Risk Score (FRS).16
Procedures, variables and study sample characteristicsSample size was calculated on the basis of the prevalence of hypertension5,6 and of CV risk factors in the Portuguese population. The sample was stratified by region (North, Central, Lisbon and Tagus Valley, Alentejo, Algarve, Azores and Madeira), maintaining equal representation of both sexes, in accordance with the specific characteristics of each municipality (urban or rural, population density and socioeconomic level), in order to obtain a sample that was representative of the country as a whole.
The required sample size was 3600 individuals. Each physician (n=240) took part in the study for two days or until 15 patients were enrolled. As PRECISE was a strictly observational study, no intervention outside normal clinical practice was involved, and all procedures followed standard good epidemiological and clinical practice. The study was authorized by the competent health authorities (the respective Regional Health Administration and the Director of the PHCC) and all patients gave their written informed consent for inclusion in the study.
A questionnaire was applied to each participant by their attending physician on a single occasion. This provided information on age at the time of assessment, age-group (in 10-year intervals from <30 to ≥80 years), body mass index (BMI) calculated as weight in kg divided by height in m2 and defining obesity as BMI ≥30 kg/m2, number of CV risk factors, and 10-year CV risk according to SCORE and the FRS.15,16
The following variables were collected: demographic (age, gender, civil status, education level and employment status), anthropometric (weight, height and BMI), smoking status (in the previous six months), physical activity (at least 30 min exercise at least twice a week), and clinical variables: SBP and DBP, time since diagnosis of hypertension (defined as BP ≥140/90 mmHg), antihypertensive medication and dosages, presence of hypercholesterolemia (defined as TC >190 mg/dl or under lipid-lowering therapy) (time since diagnosis and most recent lipid profile showing TC, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and triglyceride levels), presence of type 2 diabetes (fasting blood glucose ≥126 mg/dl [7.0 mmol/l] in two or more measurements, or ≥200 mg/dl [11.1 mmol/l two hours after a 75-g oral glucose load, or glycated hemoglobin ≥6.5% [48 mmol/mol], or under oral antidiabetic or insulin therapy),17 personal history of PAD, stroke or CAD, family history of premature CV disease15 (particularly CAD), presence of ECG-LVH, and presence of albuminuria (microalbuminuria 30-150 mg/24 hours or proteinuria >150 mg/24 hours).
Statistical analysisA descriptive analysis was performed of all the above variables, with continuous variables expressed as mean, standard deviation, median, maximum and minimum, and categorical variables expressed as absolute and relative frequencies. Bivariate analysis comparing pairs of categorical variables used contingency tables and the chi-square test and Fisher's exact test, while continuous and categorical variables were compared using the t test for independent samples or the non-parametric Kruskal-Wallis test. Missing values were not included in the statistical analysis. All analyses were carried out using SPSS version 15.0 (SPSS Inc., Chicago, IL), and the level of significance was taken to be p<0.05.
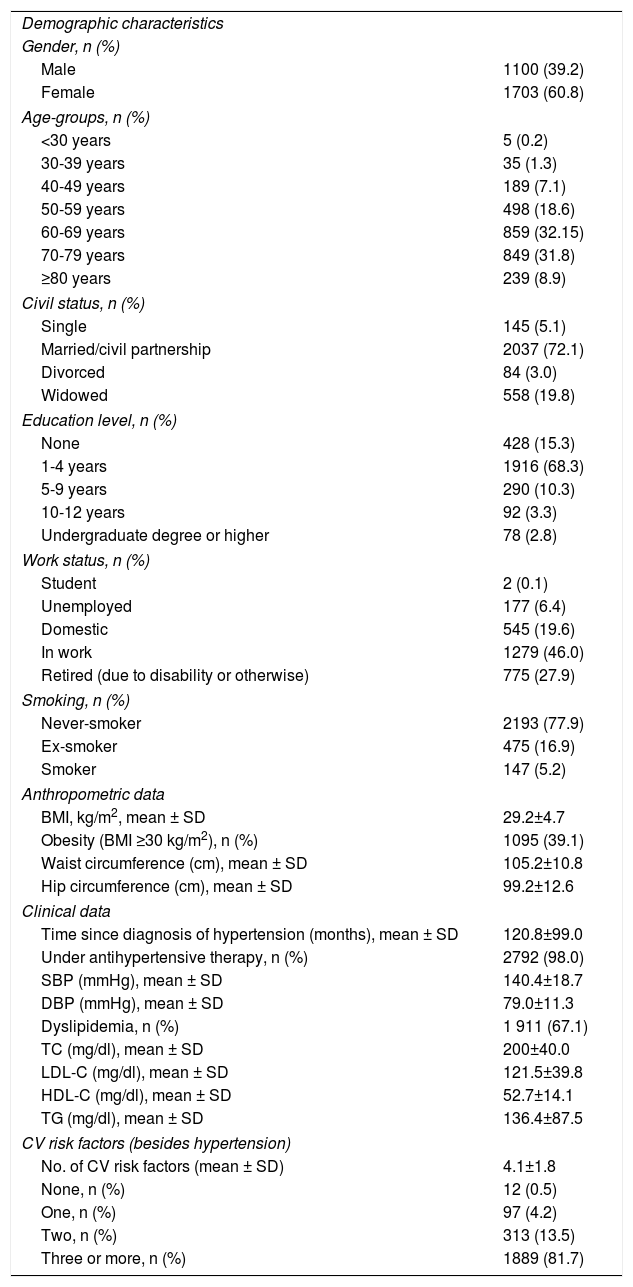
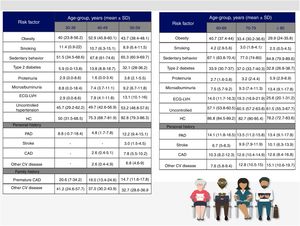
ResultsA total of 2848 individuals were included, 39.2% male and 60.8% female (Table 1). Their mean age was 65.8±11.0 years, most (63.9%) in the 60-79 age-group. In terms of civil status, 72.1% were married or in a civil partnership, while 20% were widowed. Education level was generally low, only 16% of the sample having more than four years of schooling and only 6.1% having 12th-year or higher education. Only 5.2% were active smokers and 16.6% were former smokers; mean consumption was 22 cigarettes/day, significantly more in men than in women (22.8±14.6 vs. 12.8±10.5, respectively; p<0.001).
General characteristics of the study population.
| Demographic characteristics | |
| Gender, n (%) | |
| Male | 1100 (39.2) |
| Female | 1703 (60.8) |
| Age-groups, n (%) | |
| <30 years | 5 (0.2) |
| 30-39 years | 35 (1.3) |
| 40-49 years | 189 (7.1) |
| 50-59 years | 498 (18.6) |
| 60-69 years | 859 (32.15) |
| 70-79 years | 849 (31.8) |
| ≥80 years | 239 (8.9) |
| Civil status, n (%) | |
| Single | 145 (5.1) |
| Married/civil partnership | 2037 (72.1) |
| Divorced | 84 (3.0) |
| Widowed | 558 (19.8) |
| Education level, n (%) | |
| None | 428 (15.3) |
| 1-4 years | 1916 (68.3) |
| 5-9 years | 290 (10.3) |
| 10-12 years | 92 (3.3) |
| Undergraduate degree or higher | 78 (2.8) |
| Work status, n (%) | |
| Student | 2 (0.1) |
| Unemployed | 177 (6.4) |
| Domestic | 545 (19.6) |
| In work | 1279 (46.0) |
| Retired (due to disability or otherwise) | 775 (27.9) |
| Smoking, n (%) | |
| Never-smoker | 2193 (77.9) |
| Ex-smoker | 475 (16.9) |
| Smoker | 147 (5.2) |
| Anthropometric data | |
| BMI, kg/m2, mean ± SD | 29.2±4.7 |
| Obesity (BMI ≥30 kg/m2), n (%) | 1095 (39.1) |
| Waist circumference (cm), mean ± SD | 105.2±10.8 |
| Hip circumference (cm), mean ± SD | 99.2±12.6 |
| Clinical data | |
| Time since diagnosis of hypertension (months), mean ± SD | 120.8±99.0 |
| Under antihypertensive therapy, n (%) | 2792 (98.0) |
| SBP (mmHg), mean ± SD | 140.4±18.7 |
| DBP (mmHg), mean ± SD | 79.0±11.3 |
| Dyslipidemia, n (%) | 1 911 (67.1) |
| TC (mg/dl), mean ± SD | 200±40.0 |
| LDL-C (mg/dl), mean ± SD | 121.5±39.8 |
| HDL-C (mg/dl), mean ± SD | 52.7±14.1 |
| TG (mg/dl), mean ± SD | 136.4±87.5 |
| CV risk factors (besides hypertension) | |
| No. of CV risk factors (mean ± SD) | 4.1±1.8 |
| None, n (%) | 12 (0.5) |
| One, n (%) | 97 (4.2) |
| Two, n (%) | 313 (13.5) |
| Three or more, n (%) | 1889 (81.7) |
BMI: body mass index; CV: cardiovascular; DBP: diastolic blood pressure; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; SBP: systolic blood pressure; SD: standard deviation; TC: total cholesterol; TG: triglycerides.
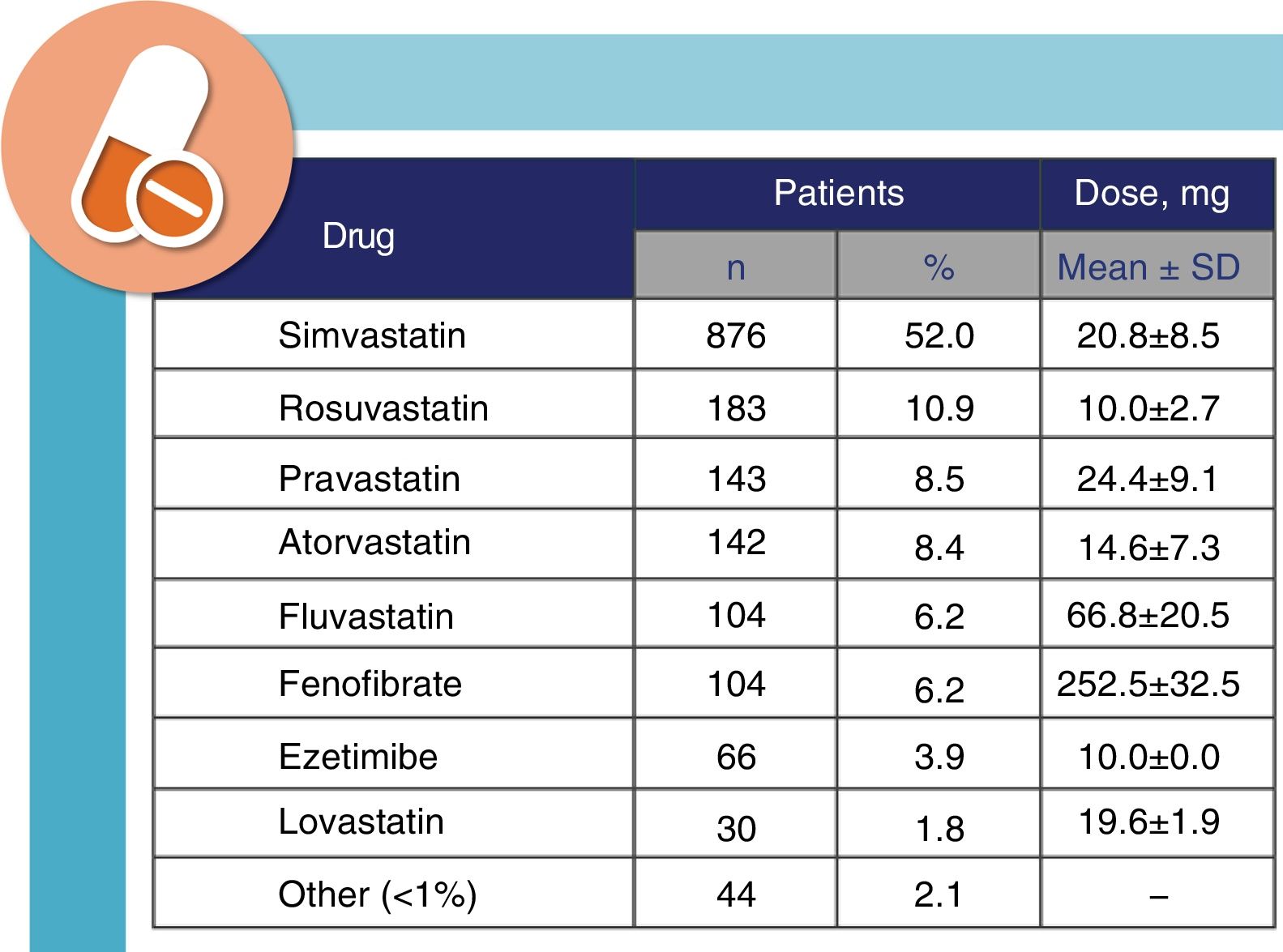
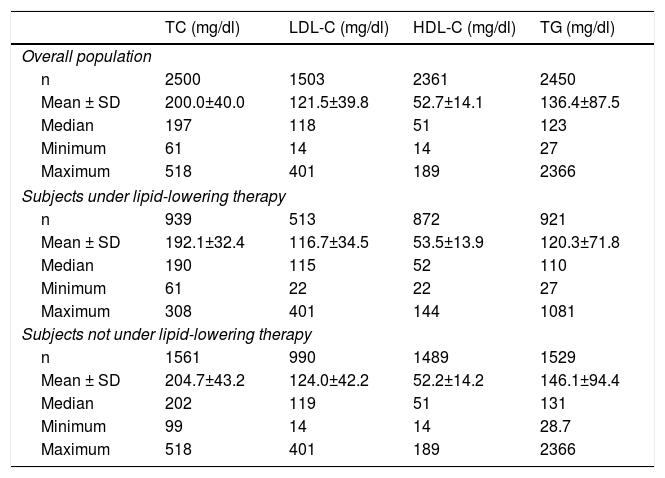
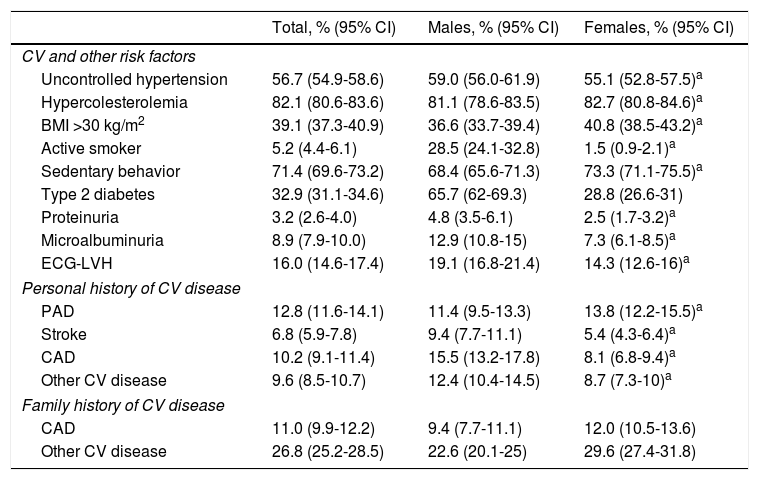
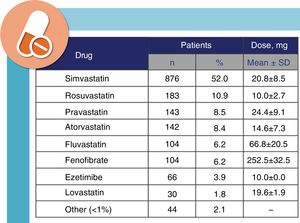
The diagnosis of hypertension was made on average around 10 years previously (albeit with considerable variation), and 98% of the patients were under antihypertensive medication. Mean SBP and DBP at the last assessment were 140.4±18.7 and 79.0±11.3 mmHg, respectively. Dyslipidemia had also been diagnosed in 1405 subjects (67.1%), a mean of around six years (79.0±63.7 months) previously, and 84% of these (56.6% of the overall population) were under lipid-lowering therapy, most with simvastatin (52.0%; mean daily dose: 20.8±8.5 mg) (Figure 1), but only 37.7% of these patients had TC <190 mg/dl. Lipid values were slightly higher in individuals who were not under lipid-lowering therapy (Table 2).
Lipid profiles in the study population (most recent laboratory assessment).
| TC (mg/dl) | LDL-C (mg/dl) | HDL-C (mg/dl) | TG (mg/dl) | |
|---|---|---|---|---|
| Overall population | ||||
| n | 2500 | 1503 | 2361 | 2450 |
| Mean ± SD | 200.0±40.0 | 121.5±39.8 | 52.7±14.1 | 136.4±87.5 |
| Median | 197 | 118 | 51 | 123 |
| Minimum | 61 | 14 | 14 | 27 |
| Maximum | 518 | 401 | 189 | 2366 |
| Subjects under lipid-lowering therapy | ||||
| n | 939 | 513 | 872 | 921 |
| Mean ± SD | 192.1±32.4 | 116.7±34.5 | 53.5±13.9 | 120.3±71.8 |
| Median | 190 | 115 | 52 | 110 |
| Minimum | 61 | 22 | 22 | 27 |
| Maximum | 308 | 401 | 144 | 1081 |
| Subjects not under lipid-lowering therapy | ||||
| n | 1561 | 990 | 1489 | 1529 |
| Mean ± SD | 204.7±43.2 | 124.0±42.2 | 52.2±14.2 | 146.1±94.4 |
| Median | 202 | 119 | 51 | 131 |
| Minimum | 99 | 14 | 14 | 28.7 |
| Maximum | 518 | 401 | 189 | 2366 |
HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; SD: standard deviation; TC: total cholesterol; TG: triglycerides.
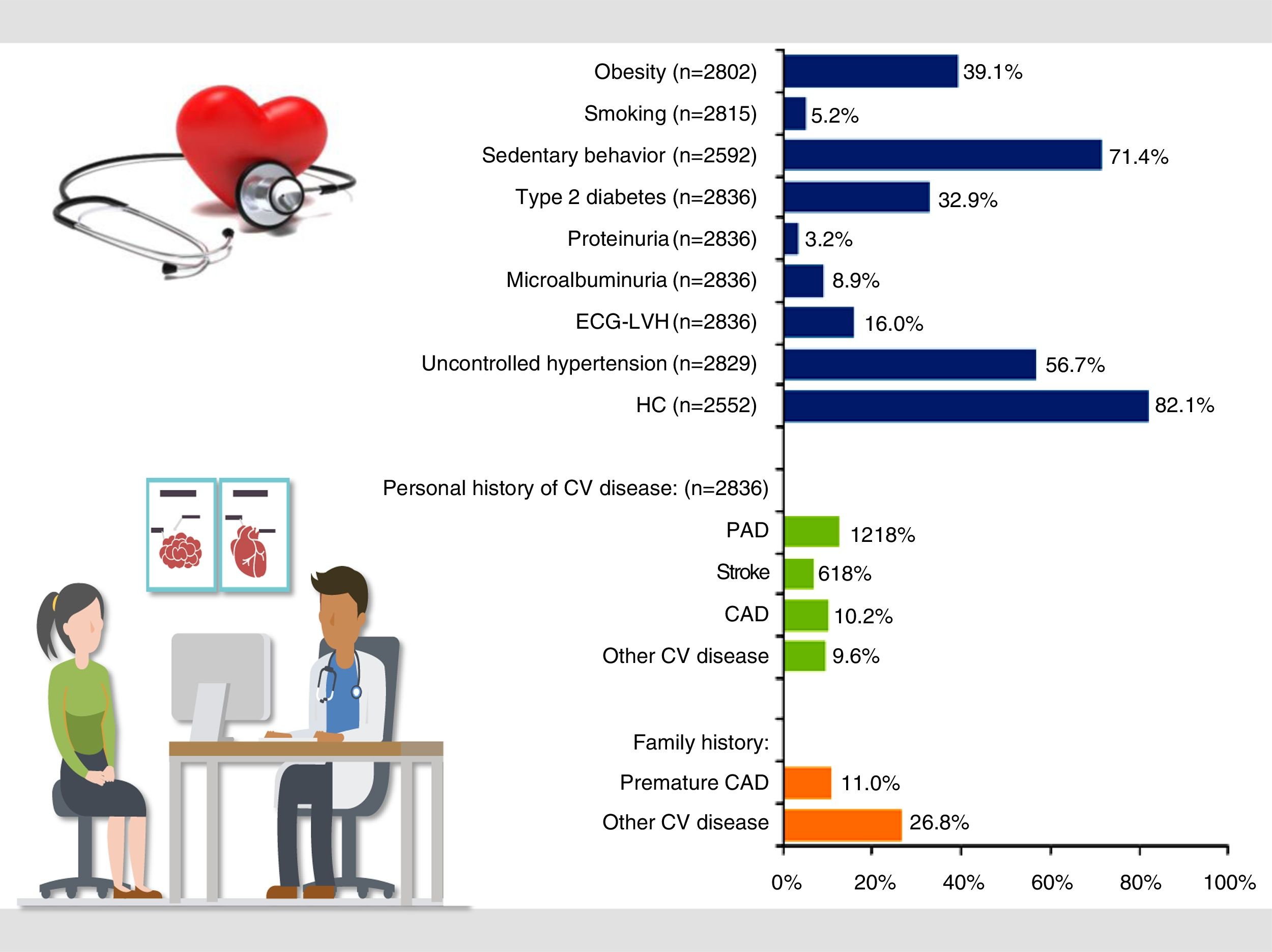
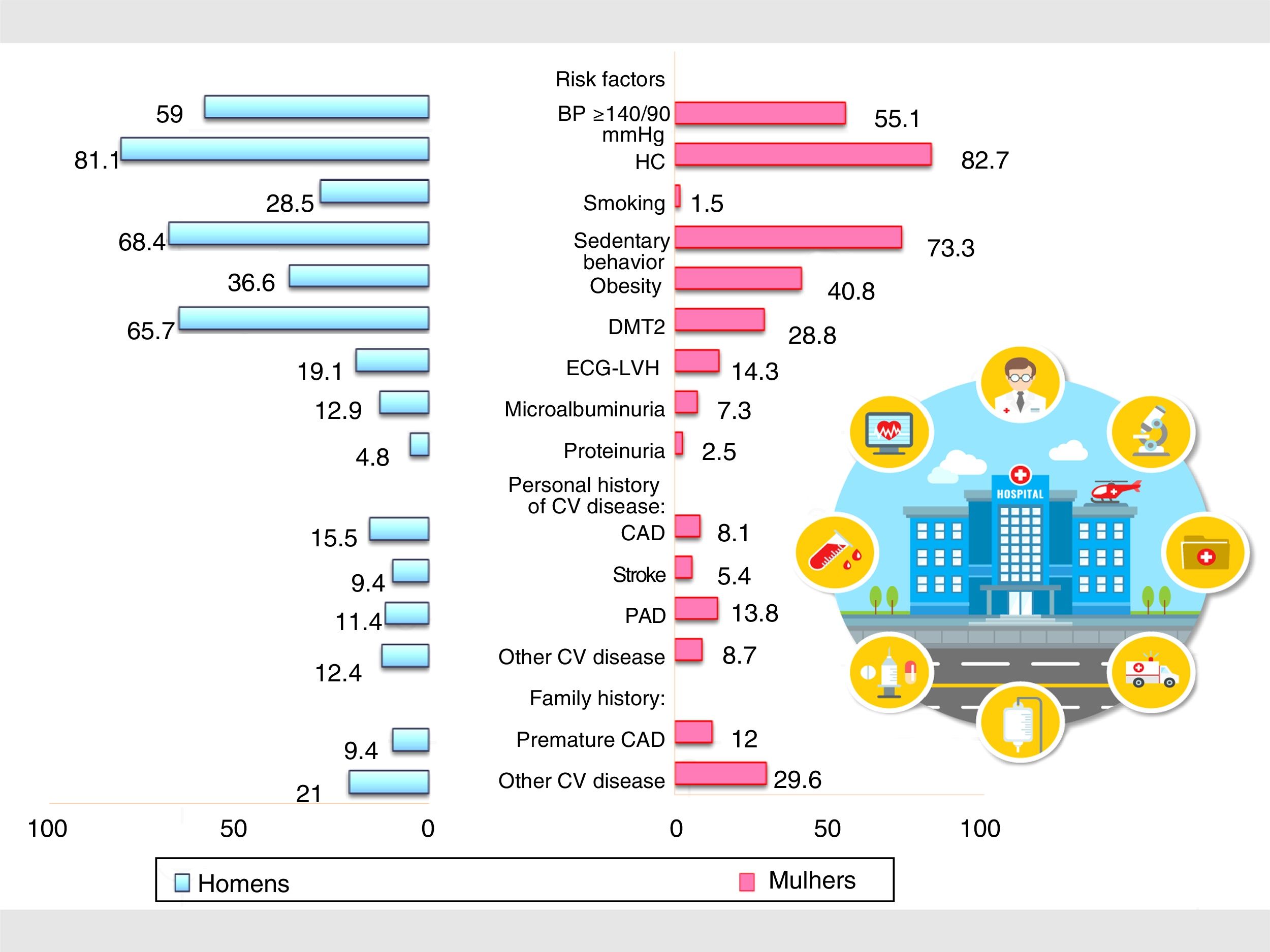
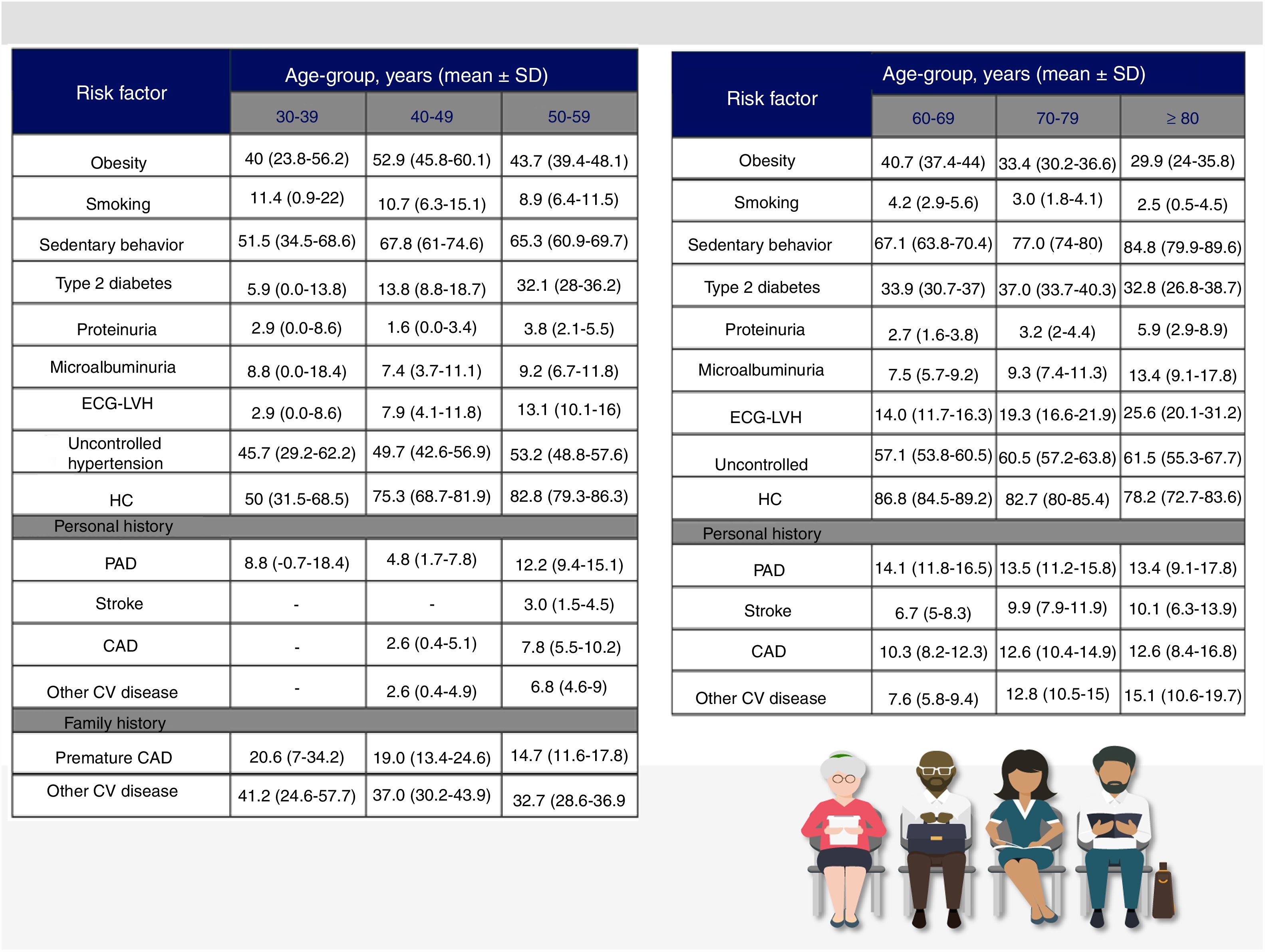
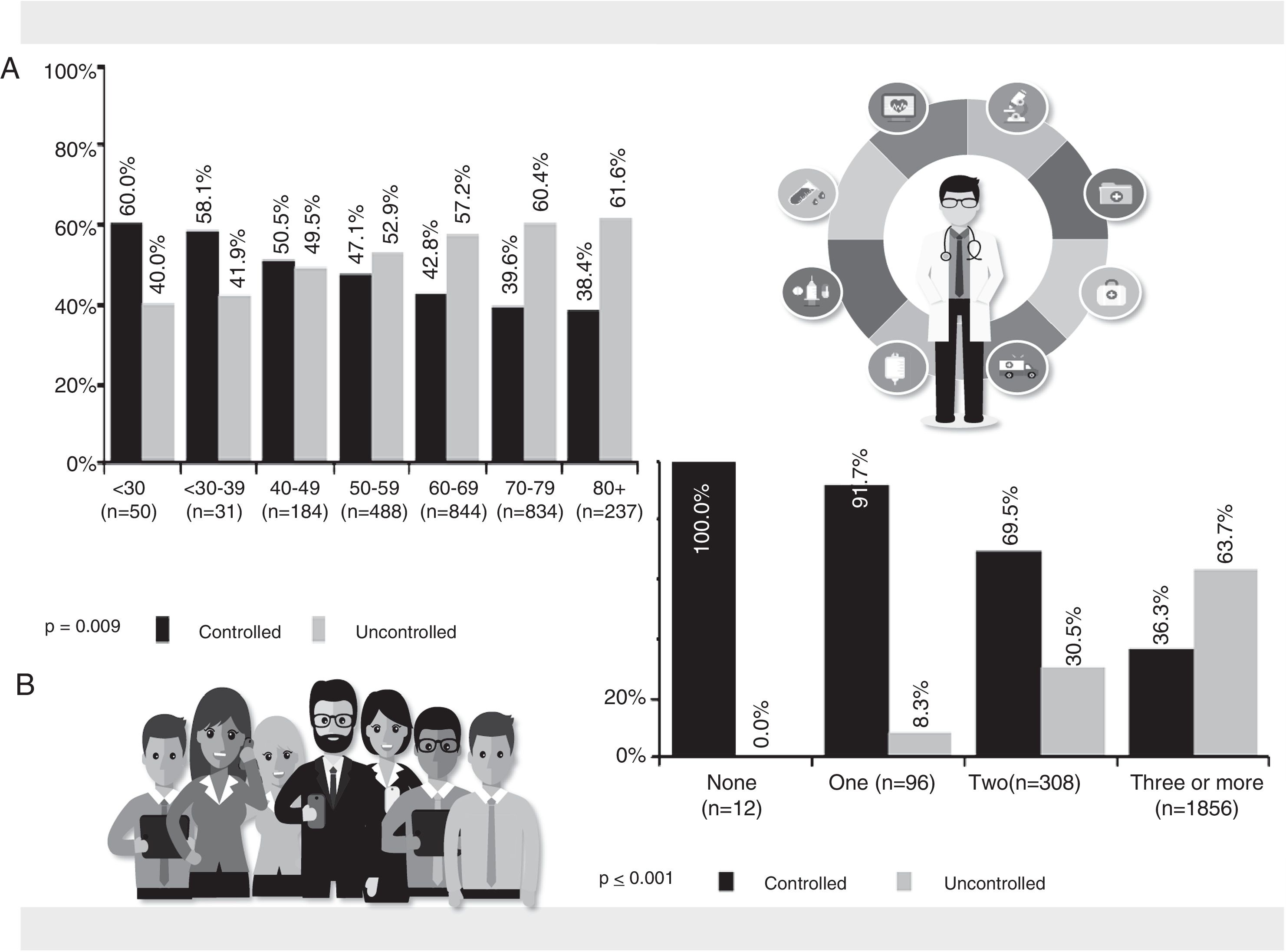
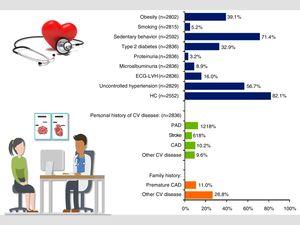
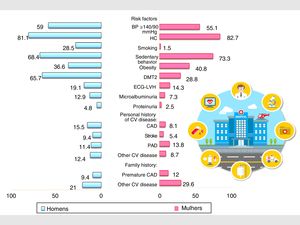
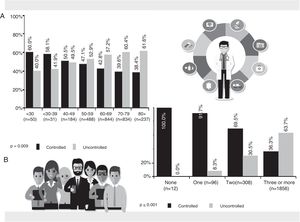
Assessment of CV risk factors and specific types of TOD showed that 81.7% of hypertensive patients had three or more concomitant risk factors (mean: 4.1±1.8), and 13.5% had two (Figure 2). The prevalence of risk factors and specific types of TOD was calculated for the overall population and by gender (Table 3) and by age-group (Figure 3). Hypercholesterolemia was the most prevalent risk factor, and most risk factors (with the exception of hypercholesterolemia, obesity, sedentary behavior, personal history of PAD and family history of CV disease) were statistically more prevalent in males, although with overlapping confidence intervals (Table 3). Figures 3 and 4 present the prevalence of CV risk factors by gender and by age-group. As expected, the prevalence of sedentary behavior, type 2 diabetes, albuminuria and history of PAD was higher in obese hypertensives (p<0.05).
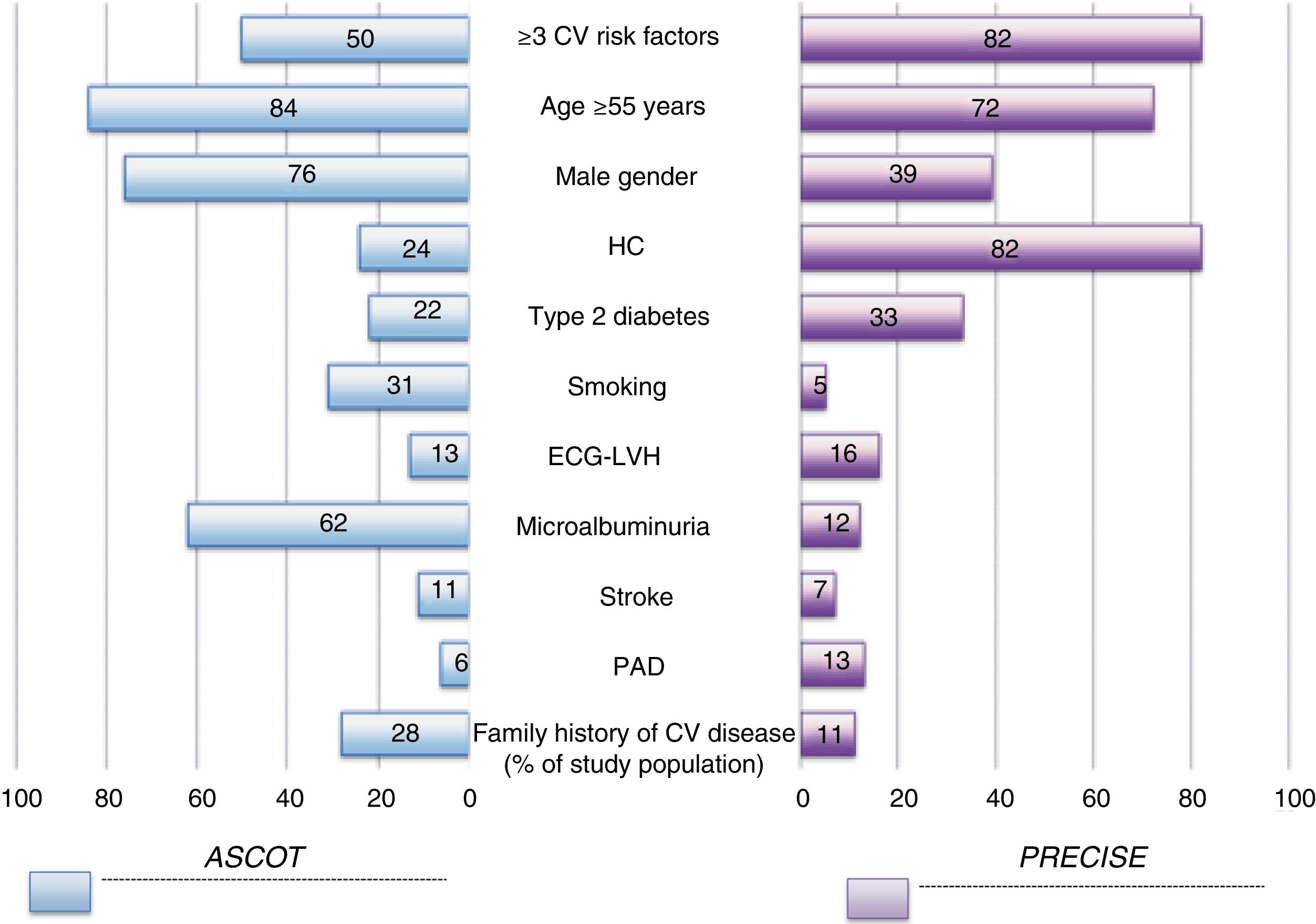
Prevalence of cardiovascular risk factors in the overall study population. CAD: coronary artery disease; CV: cardiovascular; ECG-LVH: left ventricular hypertrophy by electrocardiogram; HC: hypercholesterolemia; PAD: peripheral arterial disease. Obesity defined as body mass index ≥30 kg/m2.
Prevalence of cardiovascular risk factors and specific types of target organ damage in the overall population and by gender.
| Total, % (95% CI) | Males, % (95% CI) | Females, % (95% CI) | |
|---|---|---|---|
| CV and other risk factors | |||
| Uncontrolled hypertension | 56.7 (54.9-58.6) | 59.0 (56.0-61.9) | 55.1 (52.8-57.5)a |
| Hypercolesterolemia | 82.1 (80.6-83.6) | 81.1 (78.6-83.5) | 82.7 (80.8-84.6)a |
| BMI >30 kg/m2 | 39.1 (37.3-40.9) | 36.6 (33.7-39.4) | 40.8 (38.5-43.2)a |
| Active smoker | 5.2 (4.4-6.1) | 28.5 (24.1-32.8) | 1.5 (0.9-2.1)a |
| Sedentary behavior | 71.4 (69.6-73.2) | 68.4 (65.6-71.3) | 73.3 (71.1-75.5)a |
| Type 2 diabetes | 32.9 (31.1-34.6) | 65.7 (62-69.3) | 28.8 (26.6-31) |
| Proteinuria | 3.2 (2.6-4.0) | 4.8 (3.5-6.1) | 2.5 (1.7-3.2)a |
| Microalbuminuria | 8.9 (7.9-10.0) | 12.9 (10.8-15) | 7.3 (6.1-8.5)a |
| ECG-LVH | 16.0 (14.6-17.4) | 19.1 (16.8-21.4) | 14.3 (12.6-16)a |
| Personal history of CV disease | |||
| PAD | 12.8 (11.6-14.1) | 11.4 (9.5-13.3) | 13.8 (12.2-15.5)a |
| Stroke | 6.8 (5.9-7.8) | 9.4 (7.7-11.1) | 5.4 (4.3-6.4)a |
| CAD | 10.2 (9.1-11.4) | 15.5 (13.2-17.8) | 8.1 (6.8-9.4)a |
| Other CV disease | 9.6 (8.5-10.7) | 12.4 (10.4-14.5) | 8.7 (7.3-10)a |
| Family history of CV disease | |||
| CAD | 11.0 (9.9-12.2) | 9.4 (7.7-11.1) | 12.0 (10.5-13.6) |
| Other CV disease | 26.8 (25.2-28.5) | 22.6 (20.1-25) | 29.6 (27.4-31.8) |
Although 98% of subjects were under antihypertensive therapy, only 56.6% had BP <140/90 mmHg. There was no significant difference between the sexes in terms of BP control (p=0.079), but BP was less often controlled in older subjects (p=0.009) and in those with more concomitant CV risk factors (p<0.001). After excluding patients at high or very high baseline risk,15 25% of subjects had a 10-year CV mortality risk of 5-9% according to SCORE, and 16% had ≥10% (mean 5.7±6.2%; median 3.9%). The results from the FRS were different, with a median 10-year CV risk of 10% (mean 10.9±7.8%).
DiscussionThe main objective of the PRECISE study was to determine the prevalence of other concomitant modulating CV risk factors and certain types of TOD in hypertensive patients. There have been several other studies with similar aims, but results have been inconsistent and debate continues.10,11,18–24 Estimates of the prevalence of various CV risk factors and comorbidities differ markedly, appearing to depend largely on study design and population and the definitions of the risk factors and comorbidities under analysis. Despite this, the present study is, to the best of our knowledge, the most recent assessment of this question in Portugal (the previous one having been published in 201025), analyzing 2848 patients stratified by region, gender and age. Although time and budget constraints meant we were unable to include the initially calculated sample population, and for logistical reasons the subjects were not randomized, the study is generally representative of real-world patients in PHCCs, as demonstrated by the mean age of the population and the fact that most participants were female and in the 60-79 age-group.
The question of the prevalence of hypertension is an example of how methodological issues can give rise to disagreements. The prevalence of hypertension in Europe26 ranges from 15.2% in the UK to 31.7% in Estonia. There also appear to be differences between countries in mean BP levels, with a mean SBP in women of 115 mmHg in France and of 130 mmHg in Moldova, while in men it is 138 mmHg in Slovakia compared to 121 mmHg in Turkey. As stated above, two studies5,6 have indicated a prevalence of over 40% in Portugal. However, other studies27–29 have given lower figures. The first, in 2013, was based on computer records from health centers and general practitioners and analyzed 2 639 570 hypertensive individuals (58.04% of them female). The prevalence of hypertension was 29.1% (26.9% in men and 29.5% in women).27 It should be noted that this study presented limitations in data collection (use of computer records only, inclusion only of individuals for whom at least two BP readings were available, a lower proportion of patients aged under 35 years, exclusion of those who did not attend a PHCC), and in maintaining consistency in the definition of hypertension and in operating procedures, such as BP measurement. The other two studies found prevalences of 25.3% in 201428 and of 36.0% in 2015,29 higher in the elderly (71.3%) and in women (39.6%) in the latter. These two studies also had methodological issues, including differences in BP measurement and in study populations, and in one28 subjective perception was involved in the estimation of hypertension prevalence, a common failing of population-based epidemiological surveys.
In the present study, 99.4% of hypertensive patients had at least one additional risk factor or comorbidity, and most (around 82%) had at least three CV risk factors, and were therefore at high or very high risk. These figures support and in fact exceed those in a previous study of 2299 hypertensive patients followed in PHCCs, of whom 27% were at high CV risk and 16% were at very high risk.25 CV risk factors are rarely found in isolation (only 0.5% of subjects in our study had isolated hypertension), and when combined, in some cases a given risk factor may be associated with another, which in turn is associated with another, such as sedentary behavior and obesity, obesity and diabetes, and diabetes and albuminuria.
Furthermore, the concomitant presence of other CV risk factors in hypertensive patients greatly increases clinical and therapeutic complexity (as recognized by the European and North American guidelines on hypertension,32–34 which stress the urgency of treating concomitant risk factors), and makes BP control more difficult35, as is clear from our study (Figure 5). Although 98% of our subjects were under antihypertensive medication, 57% still had uncontrolled BP, this figure reaching 64% in those with three or more risk factors. Although there was no significant difference between the sexes, uncontrolled hypertension was more prevalent in older patients. This may be due to lower adherence to treatment, in turn because of polymedication or greater likelihood of adverse reactions,36 although this was not analyzed in the study.
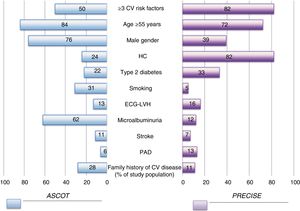
The similarity between the parameters analyzed in our study and the inclusion criteria in the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT)18 led us to compare their results (Figure 6). There are clear differences between these two high-risk populations. Mean 10-year CV risk appears less when estimated by SCORE than by the FRS (as has often been pointed out15,30,31), due to overestimation of risk in a population that differs from the one on which the score was based and because SCORE only estimates the risk of fatal events.
Graph comparing the percentages of the study populations with specific cardiovascular risk factors in the ASCOT study18 and PRECISE (the current study). CV: cardiovascular; ECG-LVH: left ventricular hypertrophy by electrocardiogram; HC: hypercholesterolemia; PAD: peripheral arterial disease. Obesity defined as body mass index ≥30 kg/m2.
In our study, a large proportion of hypertensive patients also had hypercholesterolemia (82%), only diagnosed in 67% of cases, which was often untreated and less often controlled (Table 2) or under lipid-lowering therapy at doses that were inadequate for the therapeutic goal. Hypertension approximately doubles the risk of CAD and treating high blood pressure can reduce this risk by 10-25%, while treating hypercholesterolemia in hypertensive patients reduces residual risk of CAD by 35-40%. This means that effective antihypertensive and lipid-lowering therapy can reduce CV risk by ≥50%, while also reducing the residual risk arising from treating hypertension in isolation37 and improving BP control.38 These advantages are pointed out in the most recent guidelines on treating hypertension32–34 and CV disease in general.15
Our study has certain limitations that should be acknowledged. Firstly, its cross-sectional and observational nature, and the fact that the study population is not necessarily representative of the Portuguese hypertensive population, with estimates of CV risk based on current or retrospective data, limits the generalizability of the results. Furthermore, the definitions of CV risk factors used may be different from those used in other studies and contexts. Secondly, the lipid profiles of the study population were derived from clinical records rather than from a central laboratory, which could have led to significant variations in readings, while self-reported exercise levels and smoking status are not necessarily reliable. Thirdly, there are factors other than conventional CV risk factors that affect CV risk and could therefore be relevant, such as diet and socioeconomic and psychosocial status, which were not analyzed. Finally, it should be noted that simultaneously comparing treated and untreated, and controlled and uncontrolled hypertensive individuals is complex and could lead to bias.
ConclusionThe high prevalence of CV risk factors and the persistence of concomitant uncontrolled hypertension and dyslipidemia, even under medication, suggest that current management of hypertension in particular and CV prevention generally – an increasingly complex diagnostic, therapeutic and organizational task – is inadequate. Hypertensives today, with their multiple health needs, are a challenge. A full understanding is needed of the variety of relevant risk factors, while structured interdisciplinary teams are required to prioritize and oversee the appropriate therapeutic measures. Identification of and screening for CV risk factors is thus essential. A comprehensive patient assessment, individualized diagnosis and therapy, open and regular communication between physician and patient, close coordination of health care services, persistence in overcoming obstacles, and continuous monitoring of the care provided and the results obtained, will bring benefits in reducing hypertension-related CV morbidity and mortality.39 To quote Poulter10: “It therefore seems that the focus of debate should not be whether these modifications should be made, but how best to achieve them.”
Funding sourcesThe PRECISE study was sponsored by the Portuguese Society of Atherosclerosis with the support of Grupo Keypoint. There were no external funding sources for the production of this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful to all the study investigators, Dr. Ana Macedo of Grupo Keypoint for assistance with the statistical analysis, and W4Research for editorial assistance.
Please cite this article as: Marques da Silva P, Lima MJ, Neves PM, Espiga de Macedo M. Prevalência de fatores de risco cardiovascular e outras comorbilidades em doentes com hipertensão arterial assistidos nos Cuidados de Saúde Primários: estudo Precise. Rev Port Cardiol. 2019;38:427–437.