The effectiveness of cardiac rehabilitation programs (CRP) strongly influences the recovery of functional capacity (FC), resulting in improved prognosis and survival.
ObjectiveTo determine the cardiovascular risk factors that predict changes in FC in patients on CRP.
MethodsWe performed a cross-sectional descriptive retrospective study of patients who began a CRP between January 2008 and December 2013. The dependent variable was changes in FC estimated in metabolic equivalents (METs) achieved in stress testing at the beginning and end of the phase II program. The independent variables were age, gender, dyslipidemia, diabetes, smoking, body mass index, physical activity level and reason for referral to the CRP.
ResultsThe sample included 1399 patients, of whom 1125 (80.4%) completed the program. FC improved in most patients (93%), with a mean gain of 1.45±1.19 METs. Patients aged 45–65 and over 65 years achieved a greater increase in FC compared with other age groups. Patients admitted to the CRP after coronary artery bypass graft surgery obtained a greater improvement in FC compared to patients with acute coronary syndrome. Non-diabetic patients benefited more than diabetic patients. No significant differences were seen between the groups in the other variables.
ConclusionThis study highlights the need for new and individualized approaches in certain subgroups of patients on CRP.
A eficácia dos programas de reabilitação cardíaca (PRC) associa-se fortemente à recuperação da capacidade funcional (CF) dos doentes, traduzindo-se na melhoria do prognóstico e na sobrevida.
ObjetivoDeterminar os fatores de risco cardiovascular que podem atuar como preditores da evolução da CF em doentes em PRC.
MétodosEstudo descritivo transversal retrospetivo de doentes que iniciaram um PRC, entre janeiro de 2008 e dezembro de 2013. A variável dependente é a evolução da CF estimada em equivalentes metabólicos (MET) obtidos na prova de esforço, realizada no início e no final da fase II do programa. As variáveis independentes foram a idade, género, dislipidemia, diabetes mellitus, hábitos tabágicos, índice de massa corporal, nível de atividade física e diagnóstico de admissão a PRC.
ResultadosA amostra incluiu 1399 doentes dos quais 1125 (80,4%) finalizaram a fase II do programa. Verificou-se melhoria da CF na maioria dos doentes (93%) com um ganho médio de 1,45±1,19MET. Os doentes na faixa etária (45-65] e superior a 65 anos obtiveram um incremento na CF superior quando comparados com a restante faixa etária. Os doentes admitidos para PRC após Coronary Artery Bypass Graft obtiveram um benefício superior da CF quando comparados com doentes com síndrome coronária aguda. Os doentes não diabéticos obtiveram um incremento da sua CF superior comparativamente com doentes diabéticos. Nas restantes variáveis estudadas não se obteve uma diferença significativa entre os grupos.
ConclusãoEste estudo salienta a necessidade de novas e individualizadas estratégias de atuação em determinados subgrupos de doentes em PRC.
Cardiovascular disease is the leading cause of mortality and morbidity in Portugal, making atherosclerotic disease an important public health issue that requires measures for primary and secondary prevention.1,2
The 2008 Framingham general cardiovascular risk profile identified the main risk factors for cardiovascular disease (CVD) as age, gender, total cholesterol, high-density lipoprotein (HDL) cholesterol, systolic blood pressure, diabetes and smoking.3 Of these, most are modifiable, offering a window of opportunity to significantly reduce the global burden of CVD.
Exercise-based cardiac rehabilitation programs (CRP) are an important element in the prevention and treatment of CVD and in the control of cardiovascular risk factors.4
A significant factor in the effectiveness of CRP is their positive effect on patients’ functional capacity, which results in improved prognosis and survival after diagnosis of CVD. Functional capacity following a cardiovascular event is known to be a strong independent predictor of mortality.5
Participation in a CRP has been shown to improve exercise tolerance, raise ischemic threshold, help control cardiovascular risk factors and improve general health.6,7
The objective of the present study is to determine the cardiovascular risk factors that predict changes in functional capacity in patients who have completed a CRP.
MethodsWe performed a cross-sectional descriptive retrospective study of consecutive patients diagnosed with ischemic heart disease referred for a multidisciplinary exercise-based CRP between January 2008 and December 2013.
Cardiac rehabilitation programThe CRP included individual counseling on strategies for control of cardiovascular risk factors, group health education sessions, and supervised exercise sessions.
Supervised exerciseAll patients participated in a twice-weekly exercise program supervised by physicians (physiatrist and cardiologist) with support from a physiotherapist, lasting 8–12 weeks. Each session lasted 60–90 min and included an exercise protocol consisting of a warm-up period, aerobic training (treadmill and arm and leg cycle ergometers), resistance training (using resistance bands, dumbbells, exercise balls and other strength training equipment), a cool-down period and flexibility exercises. The intensity of aerobic exercise was determined for each individual patient, based on their exercise heart rate calculated by the Karvonen formula using the data obtained from exercise testing, and complemented by the patient's rating of perceived exertion on the Borg scale.8
In addition, patients were encouraged to exercise on the other days of the week in accordance with the guidelines on secondary prevention, in order to maintain an appropriate weekly caloric expenditure.
Statistical analysisSPSS version 21.0 was used for the statistical analysis. Categorical variables were expressed as frequencies and percentages, and continuous variables as means and standard deviation according to univariate and multivariate linear regression for selected variables. The dependent variable was changes in functional capacity estimated in metabolic equivalents (METs) achieved in stress testing at the beginning and end of the program. The independent variables were age, gender, dyslipidemia, diabetes, smoking, body mass index, physical activity level (assessed using the International Physical Activity Questionnaire [IPAQ]) and reason for referral to the CRP. The IPAQ, which has been validated for the Portuguese population, is designed to quantify (in METs/min/week) the amount of exercise taken in a week performing various daily activities. The following categories were used in the analysis: sedentary (<600 METs/min/week); moderate activity (600–3000 METs/min/week); and vigorous activity (>3000 METs/min/week).9
ResultsThe sample included 1399 patients, mean age 61±11 years (Table 1), 1068 (76%) male. Analysis of cardiovascular risk factors showed 71% had dyslipidemia, 38% diabetes and 61% hypertension. Body mass index (BMI) was <25 kg/m2 (low or normal weight) in 33%, 25–30 kg/m2 (overweight) in 49% and ≥30 kg/m2 (obese) in 18%; 31% of the sample were smokers (Table 2).
Distribution of study participants’ age, overall and by year.
| Total (n=1399) | 2008 (n=141; 10%) | 2009 (n=205; 15%) | 2010 (n=240; 17%) | 2011 (n=228; 16%) | 2012 (n=282; 20%) | 2013 (n=303; 22%) | pa | |
|---|---|---|---|---|---|---|---|---|
| Age, years (mean±SD) | 61 (11) | 62 (10) | 61 (11) | 60 (11) | 60 (10) | 60 (11) | 62 (10) | 0.427 |
SD: standard deviation.
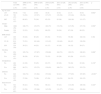
Cardiovascular risk factors in the initial study population, overall and by year.
| Total (n=1399) | 2008 (n=141; 10%) | 2009 (n=205; 15%) | 2010 (n=240; 17%) | 2011 (n=228; 16%) | 2012 (n=282; 20%) | 2013 (n=303; 22%) | p | |
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Age in years | ||||||||
| <45 | 90 (6) | 7 (5) | 18 (9) | 18 (8) | 10 (4) | 21 (7) | 16 (5) | 0.602a |
| 45–65 | 792 (57) | 74 (52) | 117 (57) | 137 (57) | 135 (59) | 153 (54) | 176 (58) | |
| ≥65 | 517 (37) | 60 (43) | 70 (34) | 85 (35) | 83 (36) | 108 (38) | 111 (37) | |
| Gender | ||||||||
| Male | 1068 (76) | 108 (77) | 154 (75) | 180 (75) | 174 (76) | 215 (76) | 237 (78) | 0.958a |
| Female | 330 (24) | 32 (23) | 51 (25) | 60 (25) | 54 (24) | 67 (24) | 66 (22) | |
| BMI (initial) | ||||||||
| <25 | 420 (33) | 39 (28) | 60 (29) | 85 (36) | 75 (33) | 59 (40) | 102 (34) | 0.382 |
| 25–30 | 614 (49) | 72 (51) | 101 (49) | 112 (47) | 110 (49) | 69 (47) | 150 (50) | |
| ≥30 | 224 (18) | 30 (21) | 44 (21) | 41 (17) | 41 (18) | 18 (12) | 50 (17) | |
| Smoking | ||||||||
| No | 954 (69) | 105 (74) | 137 (67) | 159 (68) | 164 (72) | 199 (71) | 190 (63) | 0.098a |
| Yes | 437 (31) | 36 (26) | 67 (33) | 75 (32) | 63 (28) | 83 (29) | 113 (37) | |
| Dyslipidemia | ||||||||
| No | 404 (29) | 41 (29) | 52 (25) | 82 (37) | 65 (29) | 79 (28) | 85 (28) | 0.139a |
| Yes | 968 (71) | 99 (71) | 153 (75) | 139 (63) | 160 (71) | 202 (72) | 215 (72) | |
| Diabetes | ||||||||
| No | 846 (62) | 104 (74) | 131 (64) | 153 (64) | 94 (41) | 177 (65) | 187 (65) | <0.001a |
| Yes | 527 (38) | 37 (26) | 74 (36) | 87 (36) | 134 (59) | 94 (35) | 101 (35) | |
| Hypertension | ||||||||
| No | 542 (39) | 58 (41) | 70 (34) | 98 (41) | 97 (43) | 110 (39) | 109 (36) | 0.418a |
| Yes | 857 (61) | 83 (59) | 135 (66) | 142 (59) | 131 (57) | 172 (61) | 194 (64) | |
BMI: body mass index.
According to the responses to the IPAQ, most of the population (63%) had low levels of physical activity before the CRP; only 3% reported vigorous activity. In the last two years of the study period, the prevalence of sedentary behavior increased, with rates of 72% and 76% in 2012 and 2013, respectively (Table 3).
Levels of physical activity in the study population according to the International Physical Activity Questionnaire, overall and by year.
| Total (n=1399) | 2008 (n=141; 10%) | 2009 (n=205; 15%) | 2010 (n=240; 17%) | 2011 (n=228; 16%) | 2012 (n=282; 20%) | 2013 (n=303; 22%) | pa | |
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Sedentary | 865 (63) | 65 (46) | 98 (48) | 133 (56) | 145 (64) | 202 (72) | 222 (76) | <0.001 |
| Moderate activity | 472 (34) | 65 (46) | 96 (47) | 93 (39) | 76 (33) | 74 (26) | 68 (23) | |
| Vigorous activity | 47 (3) | 10 (7) | 11 (5) | 12 (5) | 7 (3) | 4 (1) | 3 (1) |
The most frequent reason for referral (62%) to the program was acute coronary syndrome (ACS) (Table 4).
Reasons for referral, overall and by year.
| Total (n=1399) | 2008 (n=141; 10%) | 2009 (n=205; 15%) | 2010 (n=240; 17%) | 2011 (n=228; 16%) | 2012 (n=282; 20%) | 2013 (n=303; 22%) | |
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| ACS | 856 (62) | 93 (66) | 123 (60) | 135 (57) | 150 (66) | 172 (61) | 183 (61) |
| Elective angioplasty | 196 (14) | 16 (11) | 36 (18) | 41 (17) | 28 (12) | 43 (15) | 32 (11) |
| Valve surgery | 32 (2) | 0 (0) | 5 (2) | 10 (4) | 5 (2) | 6 (2) | 6 (2) |
| CABG | 142 (10) | 8 (6) | 15 (7) | 30 (13) | 25 (11) | 31 (11) | 33 (11) |
| Other | 143 (10) | 19 (13) | 24 (12) | 19 (8) | 17 (8) | 22 (8) | 42 (14) |
| Control CV risk factors | 18 (1) | 5 (4) | 2 (1) | 1 (0) | 1 (0) | 6 (2) | 3 (1) |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; CV: cardiovascular.
Of the initial sample of 1399 participants, complete data at the end of the CRP were only available for 1125, mainly because of patients lost to follow-up or leaving the program for medical or personal reasons. However, these losses did not significantly alter the prevalence of risk factors in the population (Table 5).
Sociodemographic and clinical characteristics of participants assessed at the beginning and end of the cardiac rehabilitation program (n=1125).
| n | (%) | |
|---|---|---|
| Age (years) | ||
| <45 | 71 | (6) |
| 45–65 | 666 | (57) |
| ≥65 | 388 | (37) |
| Gender | ||
| Male | 886 | (76) |
| Female | 238 | (24) |
| Reason for referral | ||
| ACS | 695 | (62) |
| Elective angioplasty | 161 | (14) |
| Valve surgery | 23 | (2) |
| CABG | 118 | (10) |
| Other | 103 | (10) |
| Control CV risk factors | 18 | (1) |
| Dyslipidemia | ||
| No | 331 | (29) |
| Yes | 770 | (71) |
| Diabetes | ||
| No | 699 | (62) |
| Yes | 408 | (38) |
| Hypertension | ||
| No | 456 | (39) |
| Yes | 669 | (61) |
| BMI | ||
| <25 | 341 | (33) |
| 25–30 | 494 | (49) |
| ≥30 | 175 | (18) |
| Smoking | ||
| No | 784 | (69) |
| Yes | 341 | (31) |
| IPAQ | ||
| Sedentary | 668 | (63) |
| Moderate activity | 403 | (34) |
| Vigorous activity | 44 | (3) |
BMI: body mass index; IPAQ: International Physical Activity Questionnaire; Other: heart failure, angina, intermittent claudication, or following implantation of biventricular pacemaker or cardioverter-defibrillator.
Analysis of the influence of cardiovascular risk factors on changes in functional capacity was thus limited to these 1125 patients.
The mean gain in functional capacity on completion of the program was 1.45±1.19 METs; the maximum gain was 7.8 METs (Table 6). Functional capacity improved in 93% of participants (Table 7).
A multivariate logistic regression model was used to determine the influence of different cardiovascular risk factors on changes in functional capacity as assessed by exercise testing. Although the goodness of fit was low (R=0.213; R2=0.045), patients with diabetes showed significantly less improvement in functional capacity than those without diabetes.
Another risk factor associated with changes in functional capacity was age. Patients aged 45–64 and over 65 more often had improved functional capacity than those aged <45. Furthermore, those referred for a CRP following coronary artery bypass grafting (CABG) had significantly greater mean improvement in functional capacity (0.44 METs) than those admitted for ACS. By contrast, those who had undergone elective angioplasty and those referred for control of cardiovascular risk factors showed less improvement in functional capacity than those referred following ACS.
No significant differences were seen between the groups in the other variables (Table 8).
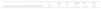
Results of univariate and multivariate regression analysis of changes in functional capacity in metabolic equivalents following the program.
| Changes in functional capacity during the program | Unadjusted β | Adjusted βa | |||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean (SD) | p | 95% CI | 95% CI | |||
| Age (years) | |||||||
| <45 | 71 (6) | 1.10 (1.19) | 0.042b | – | – | – | – |
| 45–65 | 666 (57) | 1.47 (1.17) | 0.366 | 0.074–0.657 | 0.429 | 0.116–0.742 | |
| ≥65 | 388 (37) | 1.47 (1.22) | 0.372 | 0.071–0.673 | 0.404 | 0.066–0.743 | |
| Gender | |||||||
| Male | 886 (76) | 1.47 (1.21) | 0.292b | – | – | – | – |
| Female | 238 (24) | 1.38 (1.11) | −0.092 | −0.262–0.079 | −0.104 | −0.292–0.084 | |
| Reason for referral | |||||||
| ACS | 695 (62) | 1.46 (1.15) | <0.001c | – | – | – | – |
| Elective angioplasty | 161 (14) | 1.20 (1.11) | −0.254 | −0.455–−0.052 | −0.215 | −0.448–0.019 | |
| Valve surgery | 23 (2) | 1.65 (1.22) | 0.194 | −0.294–0.682 | 0.299 | −0.255–0.853 | |
| CABG | 118 (10) | 1.90 (1.43) | 0.437 | 0.208–0.667 | 0.435 | 0.175–0.694 | |
| Other | 103 (10) | 1.28 (1.16) | −0.175 | −0.418–0.068 | −0.127 | −0.398–0.144 | |
| Control CV risk factors | 18 (1) | 0.67 (0.49) | −0.792 | −1.342–−0.242 | −0.718 | −1.410–0.026 | |
| Dyslipidemia | |||||||
| No | 331 (29) | 1.53 (1.16) | 0.132b | – | – | – | – |
| Yes | 770 (71) | 1.42 (1.21) | −0.118 | −0.273–0.036 | −0.106 | −0.275–0.064 | |
| Diabetes | |||||||
| No | 699 (62) | 1.51 (1.18) | 0.041b | – | – | – | – |
| Yes | 408 (38) | 1.36 (1.21) | −0.152 | −0.297–−0.006 | −0.191 | −0.356–−0.027 | |
| Hypertension | |||||||
| No | 456 (39) | 1.41 (1.24) | 0.342b | – | – | – | – |
| Yes | 669 (61) | 1.47 (1.16) | 0.069 | −0.073–0.211 | 0.142 | −0.023–0.306 | |
| BMI | |||||||
| <25 | 341 (33) | 1.46 (1.19) | 0.281b | – | – | – | – |
| 25–30 | 494 (49) | 1.49 (1.23) | 0.029 | −0.138–0.195 | 0.015 | −0.159–0.190 | |
| ≥30 | 175 (18) | 1.32 (1.19) | −0.139 | −0.360–0.081 | −0.046 | −0.280–0.188 | |
| Smoking | |||||||
| No | 784 (69) | 1.45 (1.18) | 0.739b | – | – | – | |
| Yes | 341 (31) | 1.43 (1.23) | −0.026 | −0.177–0.126 | −0.014 | −0.199–0.172 | |
| IPAQ | |||||||
| Sedentary | 668 (63) | 1.43 (1.15) | 0.824b | −0.004 | −0.367–0.359 | −0.035 | −0.415–0.346 |
| Moderate activity | 403 (34) | 1.48 (1.24) | 0.042 | −0.328–0.413 | 0.003 | −0.385–0.390 | |
| Vigorous activity | 44 (3) | 1.44 (1.34) | – | – | – | ||
BMI: body mass index; CI: confidence interval; IPAQ: International Physical Activity Questionnaire; METs: metabolic equivalents; Other: heart failure, angina, intermittent claudication, or following implantation of biventricular pacemaker or cardioverter-defibrillator; SD: standard deviation.
Multivariate analysis in this study identifies three predictors of changes in functional capacity following CRP: age, diabetes and reason for referral.
There is a statistically significant relation between the presence of diabetes and smaller gains in functional capacity during CRP. There is evidence in the literature that patients with diabetes have skeletal muscle dysfunction associated with microvascular disease, leading to reduced functional capacity. This dysfunction is reflected in loss of phosphocreatine, decreased pH and more rapid deoxygenation of skeletal muscle during exercise and slower recovery.10,11 There is also evidence that myocardial oxygen demand is higher in patients with diabetes than in non-diabetic individuals.11 The increased availability of fatty acids in diabetes results in increased absorption and oxidation in the mitochondria of cardiac muscle and increases mitochondrial expression of uncoupling proteins, both of which reduce the quantity of ATP produced per molecule of oxygen consumed.12,13
In view of the above, diabetic patients can be expected to show less improvement. It may therefore be advantageous to focus greater efforts on these patients, by increasing the number of CRP sessions per week or by encouraging better adherence to home-based exercise protocols outside the formal sessions.
Age was also a statistically significant predictor of changes in functional capacity in our study, with middle-aged (45–65) and older (over 65) patients achieving greater improvement than younger patients (aged <45). These findings are in agreement with those of similar studies, which report higher gains in functional capacity in older patients.14,15 Functional capacity declines by 8–10% per decade in non-athletes, largely due to reduced peak heart rate and peak aerobic capacity.16 However, older patients who undergo an appropriate individualized CRP present the same benefits as other individuals, and in fact their gains can be greater, perhaps due to their initially lower baseline functional capacity.
For these reasons, more older patients should be referred for these programs, due to their clear benefits in terms of functional capacity.
Overweight and obesity were not statistically significant predictors of changes in functional capacity in our study. This conflicts with the results of other studies in which obesity was associated with reduced exercise performance during each phase II session, ultimately resulting in smaller gains in functional capacity by the end of the program.17 An inverse relation between obesity and functional capacity has also been reported,18 with studies showing that excessive body adiposity leads to lower oxygen uptake by skeletal muscle and hence worse functional capacity.19 In addition, type II muscle fibers are increased and type I fibers are decreased in obese individuals, which is also associated with a significant reduction in oxygen uptake.20 The fact that obese individuals in our study did not, as might be expected, present worse performance can be explained by the individualized interventions that they underwent in terms of exercise and diet throughout the program.
Patients referred for the CRP following CABG showed greater improvement in functional capacity than those referred following ACS without surgery. This may be explained by the lower baseline functional capacity of the CABG patients, and thus greater benefit.
There was no statistically significant evidence of a gender influence on changes in functional capacity, which is in agreement with similar studies.21
Hypertension was not shown to affect changes in functional capacity, although there is evidence in the literature of an inverse relation between functional capacity and hypertension.22,23 Hypertensive patients would be expected to have worse baseline functional capacity, but to improve with regular exercise over the course of a CRP. While this was not observed in our study, it should be borne in mind that all patients on a CRP are closely monitored in terms of cardiovascular risk factors and medication, and so the influence of hypertension on functional capacity in our sample may have been minimized by blood pressure control and optimization of drug therapy, together with control of diet, particularly salt intake.
Dyslipidemia also did not influence functional capacity. Several studies have shown a strong correlation between improved functional capacity and reductions in total cholesterol, total triglycerides and low-density lipoprotein and increases in HDL.24,25
Smoking status at the beginning of the CRP did not appear to influence functional capacity. Smoking is known to be inversely related to functional capacity, but it has also been shown that functional capacity can at least partially recover in the long term following smoking cessation. If long-term follow-up data were analyzed, a positive relation would probably be found between smoking cessation and improvement in functional capacity.26,27
Sedentary behavior as assessed by the IPAQ was not shown to be a predictor of changes in functional capacity. It is associated with peripheral alterations, including loss of skeletal muscle and impaired muscle oxidative capacity, that reduce functional capacity.28,29 There is also evidence of a relation between sedentary behavior and vascular dysfunction, possibly due to reduced endothelium-dependent vasodilation and increased endothelial cell damage.30,31 The lack of influence of level of physical activity on changes in functional capacity in the different IPAQ categories may be explained by the fact that patients who already took moderate or vigorous exercise would tend to improve less, since they were in better physical condition before the program. All the factors associated with sedentary behavior act together to limit the gains achieved by sedentary patients on a phase II CRP.
The proportion of sedentary patients entering the CRP rose over the years, reaching a peak of 76% in 2013. This trend is worrying in view of the finding in various studies of a significant relationship between low levels of physical activity and greater risk of cardiovascular events.32 The World Health Organization has identified physical inactivity as the fourth leading risk factor for global mortality.33
Finally, irrespective of the cardiovascular risk factors presented and their prevalence in the study sample, improvements in functional capacity were seen in 93% of the 1125 participants by the end of the program. This finding reinforces the importance of such programs for improving patients’ prognosis and survival.
Study limitationsThe study has certain limitations that could influence the results obtained. The fact that only the risk factors present at the start of the program were considered, and that changes in these factors were not analyzed as the program progressed, could affect the correlation between these factors and changes in functional capacity.
Psychological and social factors were not assessed, which to a certain extent limits the conclusions that can be drawn, since these factors have been shown to influence patient adherence to and performance on a PRC.34 The fact that neither medication nor severity of coronary artery disease (number of vessels involved, revascularization, and presence of systolic and/or diastolic dysfunction) were recorded means that these variables, which could also have affected the results, were not analyzed.
In view of the considerable impact that functional capacity has on the survival of these patients, it would be useful to determine predictors of improved functional capacity, related not only to cardiovascular risk factors but also to sociodemographic and psychological factors (not analyzed in this study) in order to design programs that will maximize patients benefit in this area. However, it cannot be assumed that patients’ response in terms of functional capacity depends solely on endogenous factors. Indeed, the results of our study demonstrate that the factors under analysis had little influence on changes in functional capacity, which suggests that response to CRP is multifactorial.
ConclusionsThis study highlights the importance of CRP in secondary prevention of CVD, showing that most participants achieve a significant improvement in functional capacity; it also identifies patient subgroups whose response is less positive, underscoring the need for individualized approaches.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Branco C, Viamonte S, Matos C, Magalhães S, Cunha I, Barreira A, et al. Fatores preditores da evolução da capacidade funcional num programa de reabilitação cardíaca. Rev Port Cardiol. 2016;35:215–224.