We describe two cases in which a permanent pacemaker was implanted via the femoral vein, because the cephalic and subclavian veins were not patent.
The technique and its indications, advantages and potential complications are reviewed.
Apresentamos dois casos em que foi implantado pacemaker definitivo por via femoral, pelo facto de não ser possível fazê-lo através da veia cefálica ou subclávia. Descrevemos a técnica, as suas indicações, as vantagens e as complicações associadas.
Permanent pacemaker implantation via the femoral vein is an alternative for patients in whom access via the superior vena cava is impossible or contraindicated.1
We report two recent cases and review the technique and its indications, advantages and potential complications.
Case report 1A.A., an 85-year-old woman, confined to bed or armchair and dependent for daily activities but with good personal relationships, had a history of type 2 diabetes (with diabetic nephropathy and under regular hemodialysis for nine years with a tunneled central venous catheter [CVC] for vascular access), chronic anemia of chronic disease, permanent atrial fibrillation, hypertension, Parkinson's disease and degenerative osteoarthritis.
The patient was medicated with insulin, carbidopa-levodopa, aspirin, darbepoetin alfa, calcium carbonate, B-complex vitamins, folic acid, omeprazole and metoclopramide.
She was admitted for sepsis arising from infection of the CVC in the right subclavian vein; intravenous antibiotic therapy with vancomycin and gentamicin was begun. Staphylococcus epidermidis was subsequently isolated in blood cultures.
Replacement of the CVC was attempted, but the catheter could not be moved and the patient became hemodynamically unstable; it was therefore decided to leave the CVC in place and to prolong antibiotic therapy, to which there was a good clinical response.
During hospitalization, periods of symptomatic atrial fibrillation with rapid ventricular rate were observed, alternating with periods of slow ventricular rate. A diagnosis of brady-tachycardia syndrome was therefore made, and the patient was referred for permanent pacemaker implantation.
Transthoracic echocardiography excluded significant structural heart disease.
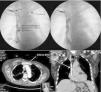
Attempts were made to introduce the leads via the left cephalic and subclavian veins but they could not be advanced. It was also impossible to obtain vascular access via the right subclavian vein due to the presence of the CVC. Obstruction of the superior vena cava was documented by both fluoroscopy and computed tomography angiography (Figure 1).
Top: Initial attempt at pacemaker implantation in the first patient, A.A., via puncture of the left subclavian vein, but the guidewire could not be advanced. The patient had a central venous catheter (CVC) in the right subclavian vein. Contrast administration showed obstruction of the superior vena cava (SVC). Bottom: computed tomography angiography images showing the CVC at the junction between the SVC and the right atrium, apparently adhering to a reduced-caliber SVC, which, combined with the collateral circulation observed, suggests secondary fibrosis of the SVC wall.
In view of the patient's limited mobility and the absence of alternative access sites, it was decided to implant a single-chamber permanent pacemaker in VVI mode via the femoral vein.
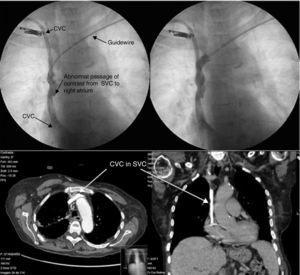
Following puncture of the right femoral vein, an 85-cm active-fixation ventricular lead was advanced up to the right ventricular apex. The lead was then tunneled subcutaneously to the right flank, where a pocket was fashioned to house and secure the pacemaker generator (Figure 2).
Fluoroscopy images during placement of a single-chamber permanent pacemaker via the right femoral vein in patient A.A. A Relia SR pacemaker (Medtronic®) in VVI mode was implanted, with an 85-cm lead. (A) Site of lead insertion in the femoral vein and position of the generator in the right flank; (B and C) course of the lead up to the apex of the RV; (D) lead positioned in the RV. IVC: inferior vena cava; RV: right ventricle.
The procedure was uneventful, with good sensing and pacing parameters.
The patient was discharged with no further complications and is currently well. The pacemaker is functioning normally four months after implantation.
Case report 2H.P., an 81-year-old woman, partially dependent due to limited right arm mobility and osteoarthritis, had a personal history of breast cancer diagnosed ten years previously and treated by right radical mastectomy, radiotherapy and chemotherapy, chronic lymphedema of the right arm, type 2 diabetes, hypertension, hypothyroidism and NYHA class II heart failure.
She was chronically medicated with oral antidiabetics, statins, amlodipine, valsartan, furosemide, spironolactone, levothyroxine, alprazolam and betahistine.
She was admitted for signs of decompensated heart failure and dizziness. On observation, she presented symptomatic bradycardia, with intermittent periods of Mobitz II and complete atrioventricular block. No electrolyte abnormalities or other reversible causes of bradyarrhythmia were identified.
Transthoracic echocardiography showed mild left ventricular systolic dysfunction (previously documented); analysis of wall motion were hindered by poor image quality, but no other relevant alterations were observed.
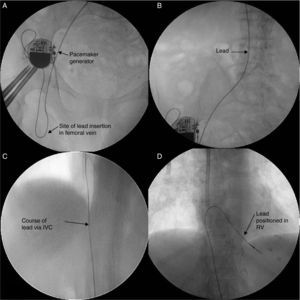
The patient was referred for permanent pacemaker implantation. Access via the left cephalic and subclavian veins was initially attempted but the leads could not be advanced (Figure 3). Despite marked lymphedema of the right arm, access via the right subclavian was also attempted but without success. Angiography confirmed obstruction at the level of the superior vena cava (Figure 3).
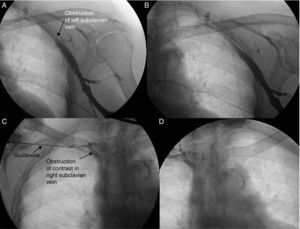
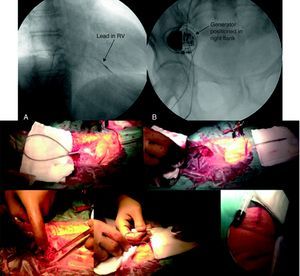
It was thus decided to implant a single-chamber permanent pacemaker via the right femoral vein, the lead being tunneled subcutaneously to the right flank and a generator pocket fashioned in the abdomen (Figure 4).
Single-chamber Relia SR pacemaker (Medtronic®) implanted via the right femoral vein in patient H.P. Top: (A) lead placed in right ventricle; (B) generator positioned in right flank. Bottom: photographs taken during pacemaker implantation, showing incisions made in the femoral region for lead insertion and in the right flank for generator placement, the subcutaneous tunneling between them, and the final result. RV: right ventricle.
The procedure and remaining hospital stay were uneventful and the patient was discharged two days later. The pacemaker is functioning normally five months later, with good sensing and pacing thresholds.
Discussion and ConclusionsPermanent pacemaker implantation using the femoral vein was first described in the early 1980s,2 but it remains unfamiliar to most operators.
However, femoral access for transvenous temporary pacing is a frequent option, due to ease of implantation and low risk of periprocedural complications.3
The most common indications for transfemoral pacing are: abnormalities of the venous system, particularly obstruction of the subclavian vein or the superior vena cava; structural alterations of the anterior thoracic wall, for example following radiotherapy or mastectomy; pacemaker implantation in children; and the presence of multiple leads in the superior vena cava or recurrent infections of the generator pocket.
Femoral access is an effective alternative to the conventional approach. Other options include venous recanalization using laser energy or surgical placement of epicardial leads. However, laser-assisted recanalization would carry significant risk in the cases presented due to the length of the obstructed segments and the patients’ comorbidities and frailty.
The incision to introduce the leads via the femoral vein was made below the inguinal ligament in order to minimize discomfort from the scar. Others, such as Ellestad et al., have opted to use an iliac vein approach.4
We decided in both cases to create the generator pocket in the abdominal region to avoid discomfort in the groin and thigh area with movement. Creation of a generator pocket in the upper thigh, an area with less subcutaneous tissue, is also likely to increase discomfort and the risk of erosion.5
Dislodgment of leads, particularly atrial leads, is a common complication of femoral or iliac vein approaches, occurring in around 20% of cases.1,4
Although not reported in the literature, a higher incidence of lead fracture might be expected with this approach, but this can be minimized by making a wider curve in the U-turn from the femoral vein to the generator pocket in the abdominal region, allowing some slack in the subcutaneous course of the lead in order to prevent pulling when the leg is flexed. Furthermore, the groin is a less mobile region than the pectoral area, especially in elderly patients, and avoids crush injuries caused by the clavicle.
Rates of infection and deep vein thrombosis appear to be similar to the subclavian approach.6
Despite the lack of studies on the subject, most authors report a low rate of complications and the procedure, while more surgical in nature, is relatively easy to perform.1,4
In addition to pacemaker implantation, placement of cardioverter-defribillators5,7 and biventricular pacemakers8–10 using the femoral approach has also been reported.
Pacemaker implantation via the femoral vein should be considered when conventional access in the pectoral region is not possible.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodrigues P, Reis H, Lagarto V, et al. Implantação de pacemaker definitivo por via femoral. Rev Port Cardiol. 2014;33:733.