Cardiac computed tomography (CT) documents the presence of coronary artery disease, regardless of the degree of stenosis. The prognostic value of non-obstructive coronary artery disease documented by cardiac CT has recently been validated. However, there are still no clear guidelines on the management of such patients, particularly concerning initiation of more aggressive pharmacological measures for primary prevention. The approach to these patients remains controversial, especially in cases in which there is a discrepancy between cardiovascular risk and the atherosclerotic burden as documented by cardiac CT.
The authors describe the case of a patient with a discrepancy between the extent of documented coronary atherosclerosis and that estimated according to pretest probability and cardiovascular risk scores. As this individual had more severe coronary atherosclerosis than expected (calcium score above the 90th percentile and non-obstructive coronary artery disease on cardiac CT) but was a competitive athlete and otherwise asymptomatic and without risk factors or cardiovascular history, with a very low estimated cardiovascular risk, it was difficult to decide on the risks and benefits of pharmacological primary prevention.
A tomografia computorizada cardíaca (angioTC cardíaca) permite documentar a presença de doença coronária, independentemente do seu grau de estenose. Recentemente, foi validado o valor prognóstico da doença coronária não obstrutiva documentada por angioTC cardíaca. No entanto, não existem ainda recomendações claras acerca da abordagem destes doentes, nomeadamente sobre o início de medidas farmacológicas mais agressivas em prevenção primária. A abordagem destes doentes permanece controversa, sobretudo nos casos em que existe uma discrepância entre o risco cardiovascular e a carga aterosclerótica objetivada na angioTC.
Os autores descrevem o caso de um doente com discrepância entre a extensão da aterosclerose coronária objetivada e a sua estimativa de acordo com os scores de probabilidade pré-teste e de eventos cardiovasculares. Tratando-se de um indivíduo com documentação de aterosclerose coronária acima do esperado - score de cálcio superior ao percentil 90 e doença coronária não obstrutiva na angioTC cardíaca, mas por outro lado, assintomático e sem fatores de risco nem antecedentes cardiovasculares, com uma estimativa de risco cardiovascular muito baixa e atleta de competição, torna-se difícil decidir acerca do risco/benefício de medidas farmacológicas de prevenção primária.
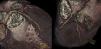
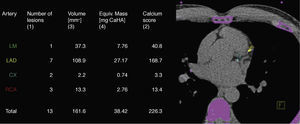
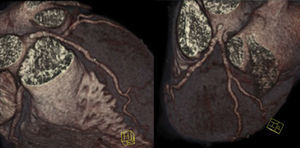
We describe the case of a 47-year-old man with no cardiovascular risk factors or relevant personal or family history, a competitive athlete participating in the Ironman triathlon of long-distance swimming (3.8 km), cycling (180 km) and running (42.2 km). He denied taking any regular medication or substance abuse (tobacco, alcohol or anabolic steroids). Following a respiratory infection, he was referred by his general practitioner for thoracic computed tomography (CT), which showed an incidental finding of “coronary artery calcification”. He was accordingly referred for cardiac CT to quantify the extent of coronary calcification and to exclude obstructive coronary artery disease (CAD). His calcium score was 226, with involvement of all the epicardial coronary arteries, but particularly in the proximal anterior descending artery (Figure 1). According to published normograms,1 this figure is well above that expected for a man of his age (above the 90th percentile), and in the expected range (50th percentile) for someone in the sixth decade of life.
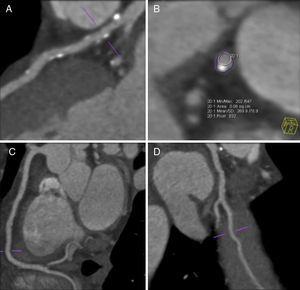
Contrast imaging excluded obstructive CAD but revealed mixed plaques, predominantly calcified, throughout the coronary tree, particularly in the left main and the proximal segment of the anterior descending artery. Positive remodeling was evident in some plaques (Figures 2 and 3).
On the basis of these exams the patient was referred to a cardiologist. He was asymptomatic and the physical examination showed no relevant alterations, with blood pressure 140/80 mmHg, heart rate 60 bpm and body mass index 23.7 kg/m2. Cardiac auscultation revealed regular S1 and S2 and no murmurs, and pulmonary auscultation showed normal breath sounds, with no adventitious sounds; there was no peripheral edema, and distal pulses were palpable, strong and symmetric.
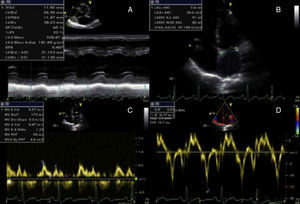
The patient had undergone laboratory tests, exercise testing and echocardiography less than six months previously as part of a medical checkup at work. Laboratory tests revealed hemoglobin 14.0 g/dl, fasting blood glucose 84 mg/dl, total cholesterol 217 mg/dl, LDL cholesterol 116 mg/dl, HDL cholesterol 116 mg/dl and triglycerides 70 mg/dl. The exercise test, following the Bruce protocol, lasted 21 minutes, reaching 19.3 METs, with normal chronotropic (101% of maximum predicted heart rate) and blood pressure changes (baseline blood pressure 130/80 mmHg and 200/80 mmHg at peak exercise); the patient experienced no angina or other symptoms during the test and there were no electrocardiographic changes suggestive of ischemia or arrhythmia. Echocardiography revealed alterations typical of athlete's heart (mild eccentric left ventricular hypertrophy) but no ventricular dilatation, normal ejection fraction and diastolic function, and slight left atrial dilatation (Figure 4).
According to scores of likelihood of CAD, the patient had a low probability of CAD, particularly given his age and the absence of symptoms – Diamond and Forrester method: low probability; Morise score: 6 points (low probability with <8).
His estimated risk of cardiovascular events was also low (HeartScore 1% and Framingham score 4%), again in the light of his age, absence of risk factors and favorable lipid profile.
Although this was an asymptomatic individual with low cardiovascular risk, it was decided to begin pharmacological therapy with a statin (rosuvastatin 5 mg/day) as well as maintaining preventive measures to control cardiovascular risk factors, given the presence of atherosclerotic CAD on cardiac CT and high calcium score. He was also advised to reduce the intensity of his sporting activity, particularly in highlevel competition.
DiscussionThe case presented describes a patient with a significant discrepancy between the coronary atherosclerotic burden documented by cardiac CT and low estimated cardiovascular risk. This raises various questions to which there are as yet no conclusive answers, particularly regarding indications for cardiac CT and the management of patients with documented non-obstructive CAD, a patient group that is increasingly encountered in clinical practice and for whom there are no clear guidelines.
The first step in the approach to a patient with suspected CAD should be comprehensive clinical assessment, including calculation of the pretest probability of CAD and estimation of cardiovascular risk. There are numerous scores for this risk stratification, the Diamond and Forrester method and the Morise score being most commonly used for determining pretest probability of CAD, and the HeartScore and Framingham score for cardiovascular events. Our patient had a low probability of CAD and low risk for cardiovascular events on all these scoring methods.
In the case presented, the first point to discuss is the patient's referral for cardiac CT and calcium scoring, neither of which is indicated for asymptomatic patients at low cardiovascular risk; both exams have a class III recommendation (“no benefit”) in the American College of Cardiology Foundation/American Heart Association guideline for assessment of cardiovascular risk in asymptomatic adults.2 Increased availability of diagnostic exams can lead to their indiscriminate use in cases for which they are not indicated, and results can be difficult to interpret. In the case presented, the results of these exams meant that the patient's risk level increased beyond that indicated by his scores on pretest probability of CAD and cardiovascular risk, both because of the higher long-term mortality associated with higher calcium scores,3 and because non-obstructive CAD, as well as obstructive disease, is associated with worse prognosis than in those without coronary stenosis, as shown by analysis of the 23 854 patients in the recent multicenter CONFIRM registry.4 The alterations found in this patient – elevated calcium score and non-obstructive plaques – will have a negative prognostic impact.
The question also arises of what preventive measures to adopt. Atherosclerotic disease is a subclinical manifestation of CAD and can be considered a qualifier, putting a patient at a higher risk level with indication for different preventive measures from those with the same risk profile but without such alterations.5 Independently of the patient's lipid profile, which was favorable in this case with the higher HDL cholesterol often found in athletes, statin therapy can be indicated, as well as standard preventive measures to control cardiovascular risk factors.6,7 Thus, as well as controlling risk factors by maintaining a healthy lifestyle, the strategy adopted included beginning statin therapy, given the proven reduction in degree of stenosis and plaque volume in patients medicated with statins.8 Another drug class with demonstrated benefits in CAD patients is antiplatelet agents; however, according to the European guidelines on cardiovascular disease prevention, they should only be prescribed in patients with established CAD or high cardiovascular risk (HeartScore >10%).5 We accordingly decided not to prescribe antiplatelet therapy, especially in the light of the significant adverse effects of these drugs, particularly in someone exposed to the risk of bleeding due to his sports activities.
Another important point is whether such an individual should reduce or cease vigorous exercise, particularly in high-level competition. According to the recommendations of the 36th Bethesda Conference, the triathlon requires high levels of both dynamic and static exercise9; the Ironman event demands even higher levels. The Bethesda Conference stated that athletes with CAD at mildly increased cardiovascular risk can participate in low dynamic and low/moderate static competitive sports but should avoid intensely competitive situations; it also recommended thorough evaluation in athletes with a calcium score of more than 100.9 Our patient was accordingly advised to cease participation in high-level competitions and to reduce the intensity of his sporting activity.
ConclusionAssessment of cardiovascular risk and of pretest probability are the first steps in the approach to patients with suspected CAD. The presence of non-obstructive CAD has prognostic impact, and more aggressive preventive measures should be implemented even in individuals at low cardiovascular risk. However, the best approach to adopt, particularly concerning initiation of pharmacological therapy, is still unclear. Furthermore, in patients who are competitive athletes, there is also disagreement concerning the need to advise them to reduce their sporting activities. The best attitude is probably to assess each case individually, according to the type and intensity of the sporting activity.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Dores H, de Araújo Gonçalves P, Carvalho MS, et al. Doença coronária não obstrutiva documentada por tomografia computorizada cardíaca: contraste entre a carga aterosclerótica e o risco cardiovascular. Rev Port Cardiol. 2013;32:613–618.