Apical hypertrophic cardiomyopathy is part of the broad clinical and morphologic spectrum of hypertrophic cardiomyopathy. We report a patient with electrocardiographic abnormalities in whom acute coronary syndrome was excluded and apical hypertrophic cardiomyopathy was demonstrated by careful differential diagnosis.
A miocardiopatia hipertrófica apical faz parte do amplo espectro clínico e morfológico da miocardiopatia hipertrófica. Nós reportamos um doente com alterações electrocardiográficas no qual foi excluída uma síndrome coronária aguda e foi demonstrada uma miocardiopatia hipertrófica apical usando um processo correto de diagnóstico diferencial.
Apical hypertrophic cardiomyopathy (AHCM) is part of the broad clinical and morphologic spectrum of hypertrophic cardiomyopathy (HCM).1 Cases of AHCM with and without apical aneurysm mimicking myocardial infarction have occasionally been reported.2–4 We report a patient with abnormalities on the electrocardiogram (ECG) in whom acute coronary syndrome (ACS) was excluded and AHCM was demonstrated by careful differential diagnosis.
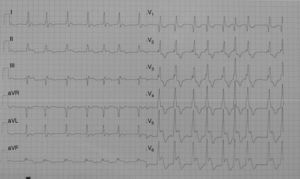
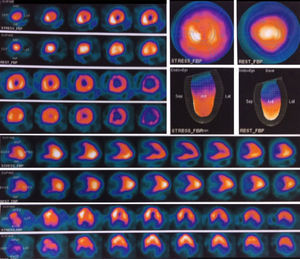
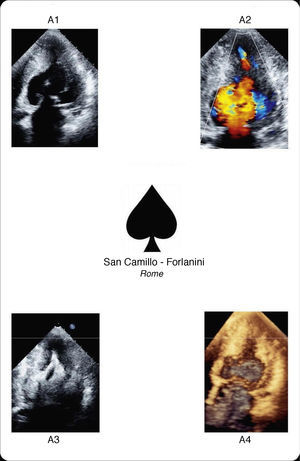
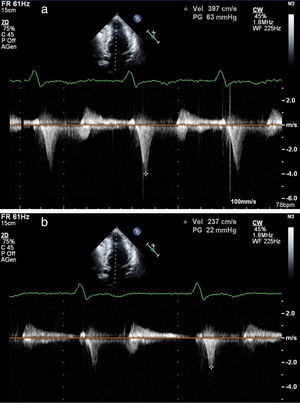
Case reportA 77-year-old Caucasian woman was examined by a primary care physician because of dyspnea and atypical chest pain. The ECG showed atrial fibrillation, mean heart rate of 85 bpm, right bundle branch block and 4-mm convex ST segment elevation in C4-C6 with biphasic T waves (Figure 1). Due to this atypical ECG, similar to a previous one performed two years before, rest-stress myocardial perfusion scintigraphy was prescribed. This revealed a reduction of left ventricular chamber volume suggestive of HCM without signs of ischemia or previous myocardial necrosis (Figure 2). The patient was referred to our echo lab in order to complete the diagnostic procedure. Transthoracic echocardiography (TTE) demonstrated AHCM, showing left ventricular (LV) apical hypertrophy with the typical ace of spades shape (Figure 3A1). The ace of spades was therefore studied in depth using color Doppler (Figure 3A2, Video 1), Sonovue contrast TTE (Figure 3A3, Video 2) and real-time three-dimensional echocardiography (Figure 3A4, Video 3). A small area of turbulent flow and a mid-ventricular gradient of about 63mmHg were found (Figure 4a). In order to evaluate possible modification of the mid-ventricular gradient, an intravenous bolus of atenolol (3mg) was administered. A significant decrease of about 40mmHg was observed while the ECG was unchanged (Figure 4b). Beta-blocker therapy was prescribed indefinitely. At six-month follow-up, the patient was asymptomatic and in good clinical condition.
AHCM is characterized by segmental hypertrophy confined to the distal portion of the LV chamber. The prevalence of AHCM among HCM patients is 15% in Japan, whereas in the USA it is only 3%. Among AHCM patients 54% are symptomatic, the most common symptoms being chest pain, palpitations, dyspnea and syncope. This condition may cause various complications including atrial fibrillation, acute myocardial infarction, embolic events, ventricular fibrillation, congestive heart failure, apical aneurysm and cardiac arrest. Moreover, it may mimic other conditions, such as cardiac tumors, LV apical thrombus, isolated ventricular non-compaction, endomyocardial fibrosis and coronary artery disease. The most common ECG findings, seen in about 93% of patients, are negative T waves in the precordial leads (>10mm deep in 47%), followed by signs of LV hypertrophy in 63% of cases. TTE usually shows LV apical hypertrophy and is thus usually the standard diagnostic tool for AHCM. Symptomatic patients may be treated with verapamil, beta-blockers and antiarrhythmic drugs, all of which may improve the signs and symptoms of this condition.
In conclusion, AHCM is a clinical condition that can cause various complications and simulate ACS. Its diagnosis enables ACS to be excluded in patients with atypical ST-segment elevation. TTE is usually sufficient to make the diagnosis, enabling appropriate medical treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.