Peripheral arterial disease involvement of the superficial femoral artery (SFA) is common. Different endovascular techniques are used successfully for revascularization of this artery. A retrograde approach to chronic total occlusion (CTO) of the SFA through the ipsilateral popliteal artery has been used occasionally if an antegrade approach is not feasible or has failed. Some of the known complications encountered during this approach are arteriovenous fistula formation at the access site, occlusion of the popliteal artery if closure devices are used, and bleeding. There are no reports of perforation or bleeding of the SFA or the external iliac artery (EIA) during a popliteal approach, probably due to lack of flow in the occluded segment of the SFA. We report a case in which a retroperitoneal hematoma occurred due to retrograde blood flow through the established true channel in the proximal SFA and subsequently to the dissection plane with a wire tip perforation in the EIA, which was treated by stopping retrograde filling with prolonged balloon inflation in the distal SFA before the CTO.
O envolvimento da artéria femoral superficial (AFS) na doença arterial periférica é comum. Existem diversas técnicas endovasculares usadas com sucesso para a revascularização desta artéria. A abordagem retrógrada da oclusão total crónica (OTC) da AFS através da artéria poplítea ipsilateral tem sido usada ocasionalmente quando a abordagem anterógrada não é possível ou após tentativa anterógrada falhada. Algumas das complicações conhecidas encontradas durante esta abordagem são a formação de fístula arteriovenosa no local do acesso, oclusão da artéria poplítea se se utilizam dispositivos de encerramento e hemorragia. Não estão descritos perfuração ou sangramento da AFS ou da artéria ilíaca externa (AIE) durante a abordagem poplítea, provavelmente devido à falta de fluxo no segmento ocluído da AFS. Aqui reportamos um caso em que ocorreu um hematoma retroperitoneal devido ao fluxo sanguíneo retrógrado através do verdadeiro canal estabelecido na AFS proximal e em consequência de plano de dissecção e perfuração com a ponta do fio-guia na AIE e o seu tratamento por paragem do preenchimento retrógrado através de insuflação de balão prolongada na AFS distal, antes da OTC.
The prevalence of peripheral arterial disease is increasing worldwide due to increase in life expectancy, obesity and diabetes.1 Symptomatic atherosclerosis of the lower extremity arteries commonly involves the superficial femoral artery (SFA) and is characterized by long, diffuse lesions and long total occlusions.1,2 Endovascular therapy has seen major advances in the last decade with the introduction of several new techniques and devices.3,4
Retrograde popliteal access has been proposed as a safe and effective means to increase the success rate of percutaneous transluminal angioplasty (PTA) for SFA occlusions after a failed antegrade attempt by means of ipsilateral or contralateral femoral access.5,6 The rationale for this increased success rate is that the distal occlusion stump in this vessel, as in others, is usually tapered, thereby increasing the likelihood of intraluminal seating of guidewires.7–9 However, the retrograde popliteal approach to SFA occlusions is a relatively new technique and there have been few reports concerning complications with this approach.
We report a case of attempted angioplasty of a CTO of the left SFA through a retrograde ipsilateral popliteal approach that was complicated by dissection and perforation causing retroperitoneal bleeding, and the management strategy successfully used to control the bleeding.
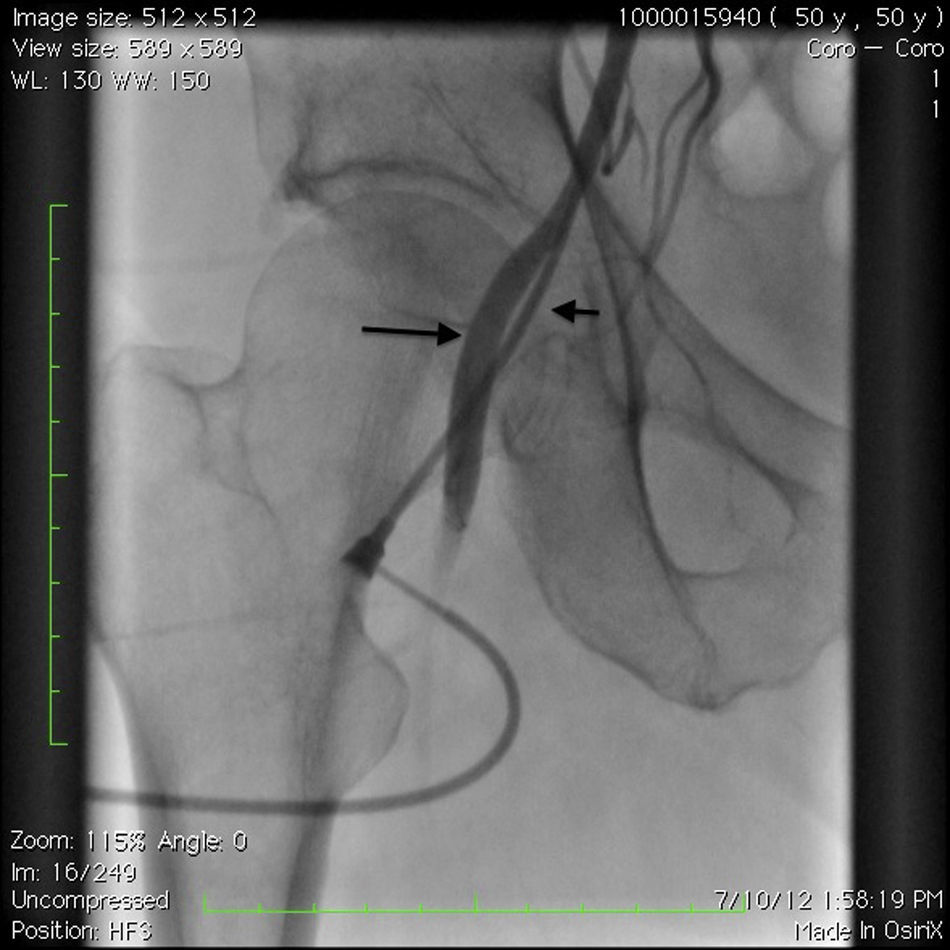
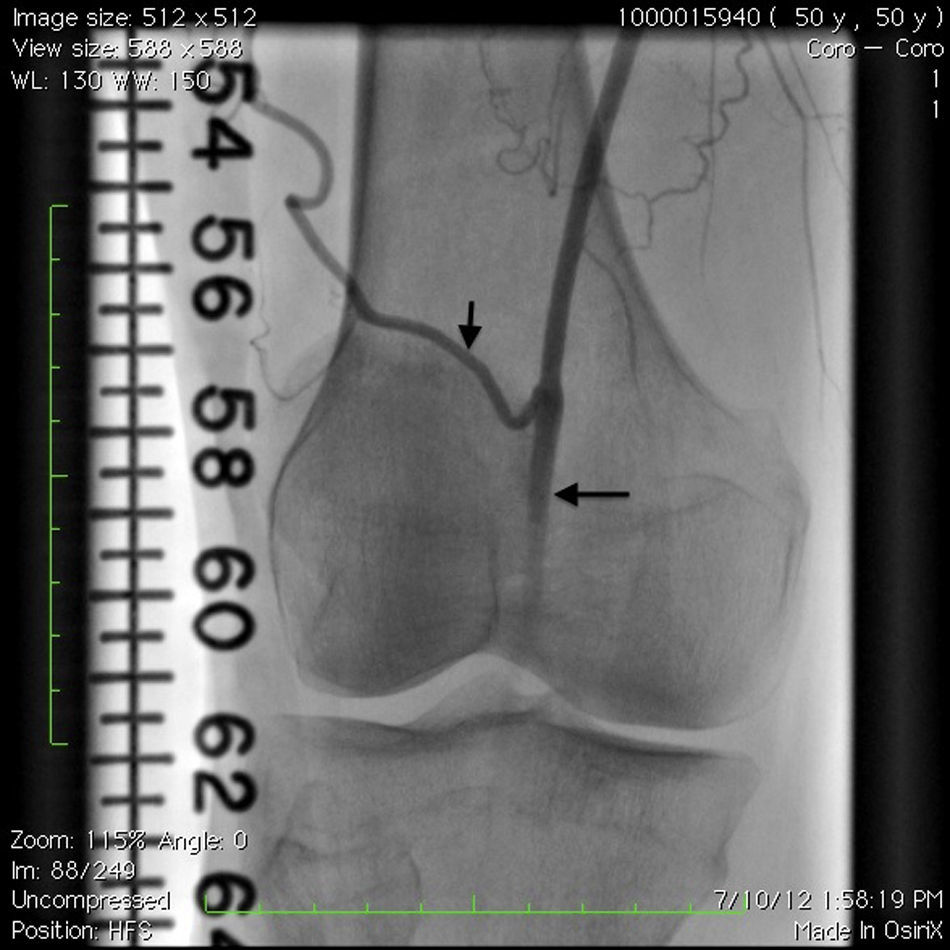
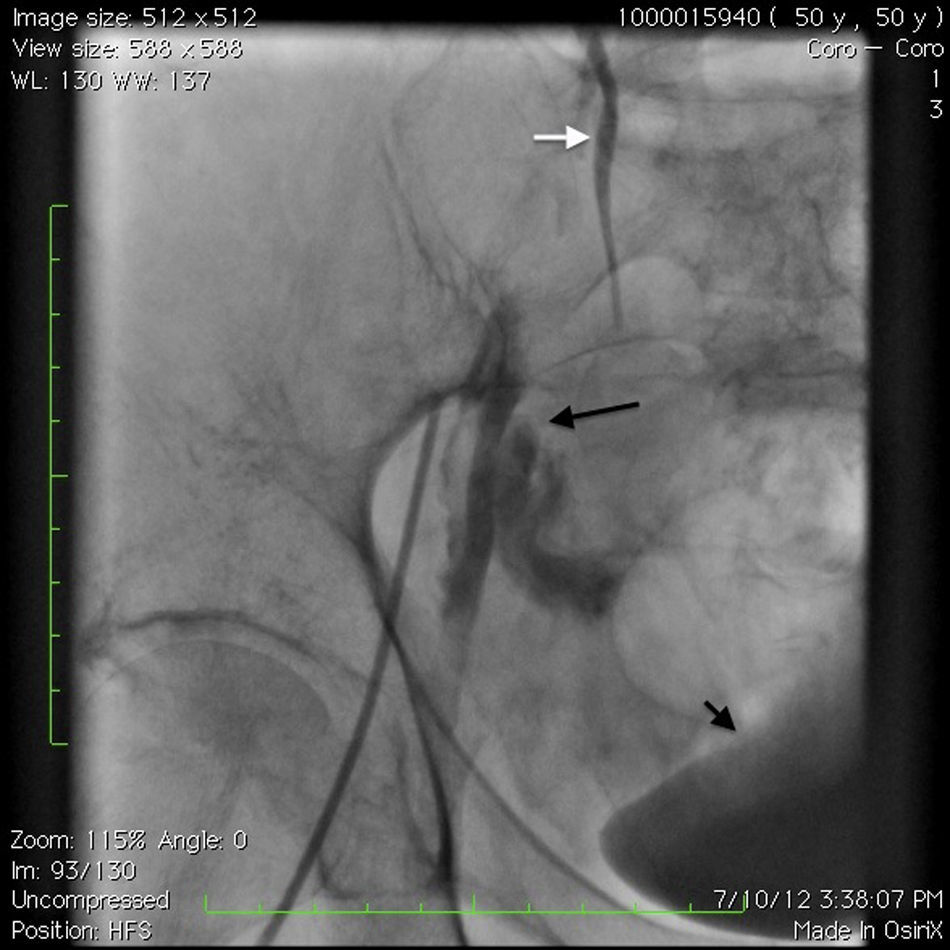
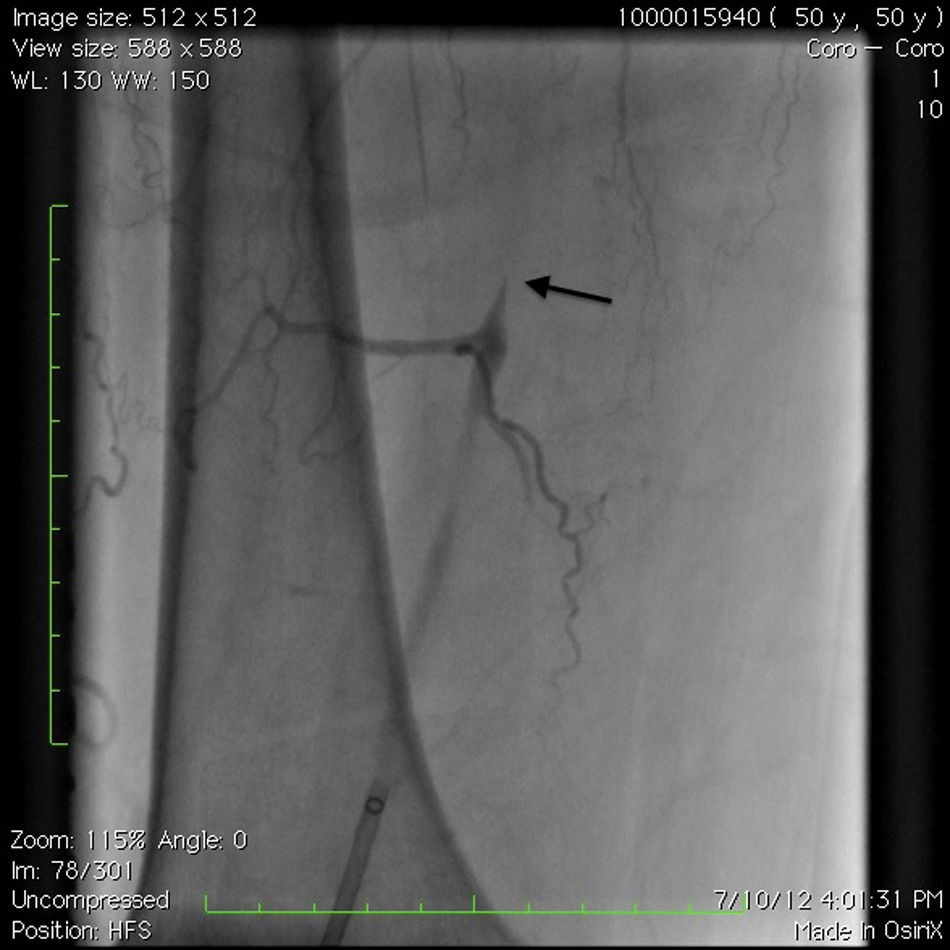
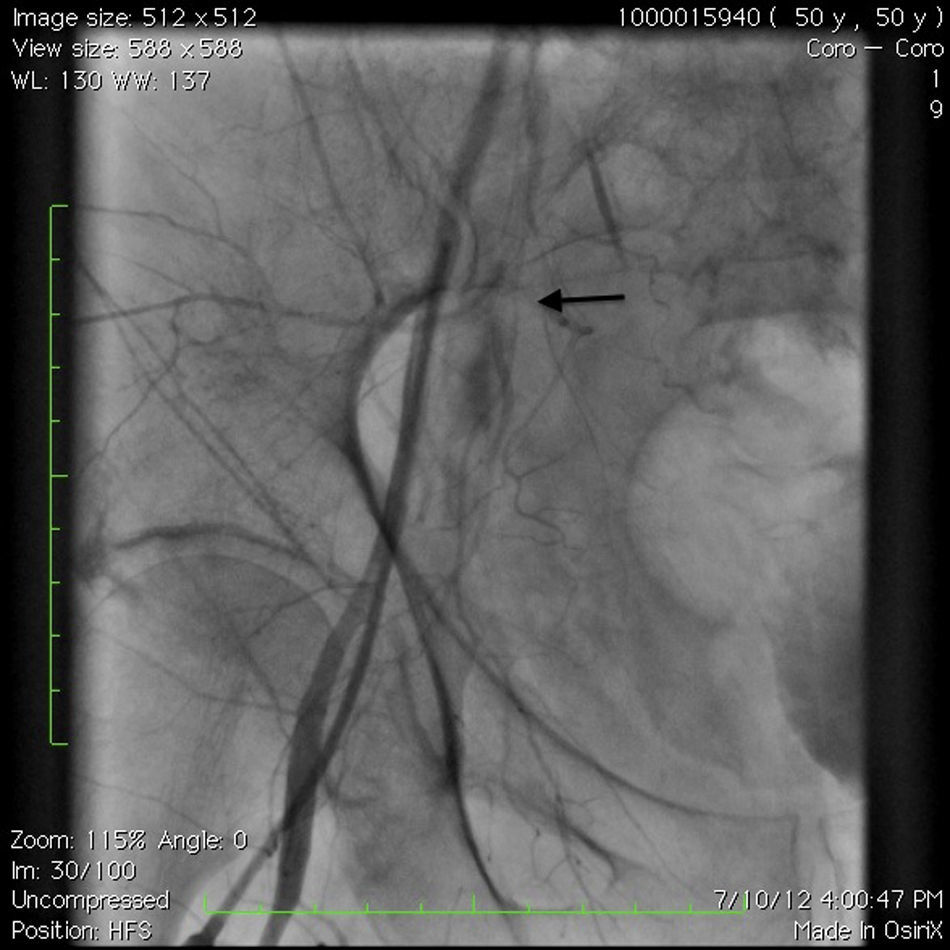
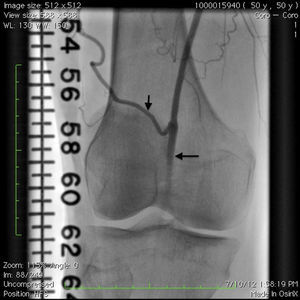
Case reportA 50-year-old Caucasian woman with hypertension, tobacco abuse, and peripheral arterial disease with life-limiting claudication had stents placed in bilateral 80% ostial iliac artery lesions two months previously. She was also noted to have a CTO of the left SFA at the ostium with no obvious stump (Figure 1) which was reconstituting distally via collaterals just above the popliteal artery (Figures 2 and 3). Due to her ongoing symptoms despite optimal medical therapy, it was decided to intervene on the SFA. Since there was no obvious stump of the occluded SFA proximally, we decided to approach the CTO through a retrograde approach.
A 4F sheath was first placed into the left femoral artery with the patient supine, and then the patient was placed in a prone position. After obtaining an angiogram of the left lower extremity, the popliteal artery was accessed under fluoroscopic guidance and a short 6-cm 6F sheath was placed. After adequate anticoagulation was achieved with heparin, a Confianza pro 12 wire (Asahi Intecc, Nagoya, Japan) was used to cross the CTO with support from a Trailblazer support catheter (ev3, Plymouth, MN), which appeared to be in the true lumen of the SFA until the proximal to ostial SFA, from where it went into multiple dissection planes. Then, the Confianza pro 12 wire was replaced by a 0.035 Glidewire Advantage wire (Terumo Interventional Systems, Somerset, NJ), which also went to different dissection planes; there was a collateral vessel at the proximal SFA extending to the external iliac artery.
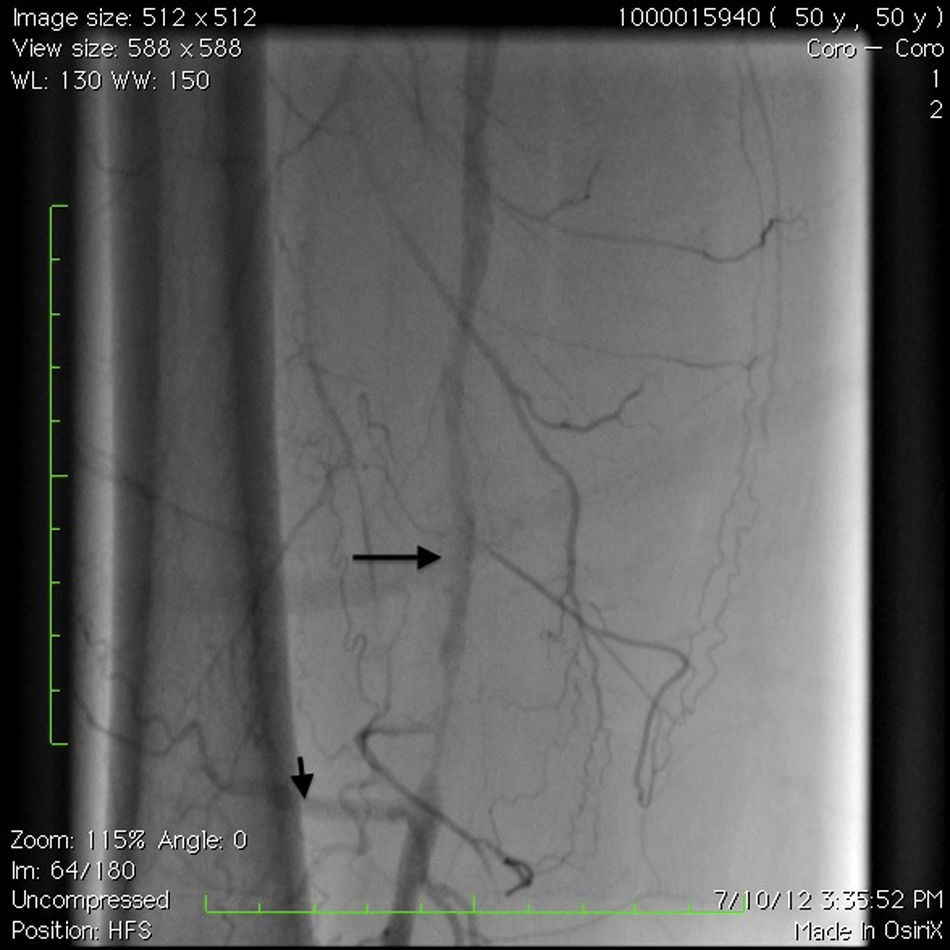
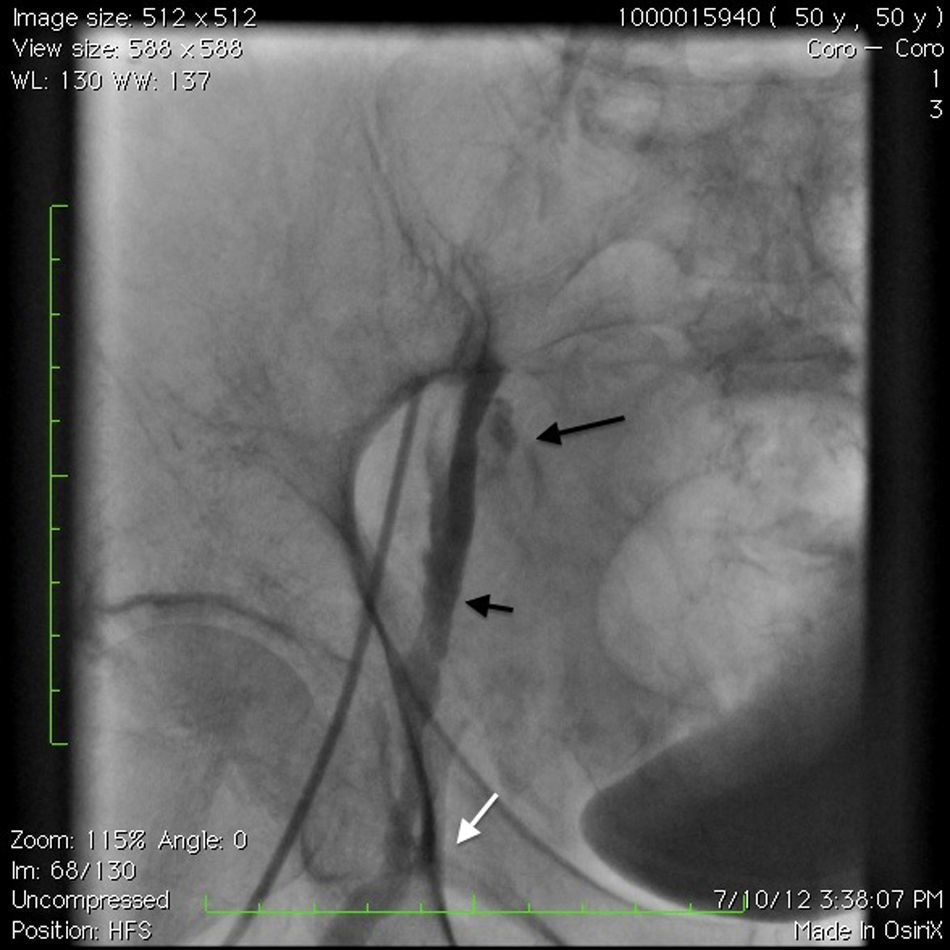
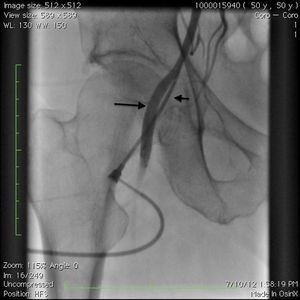
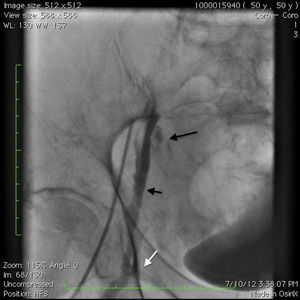
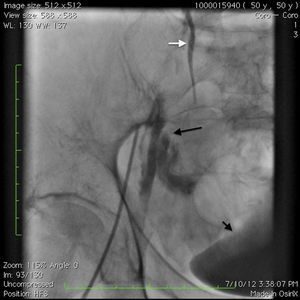
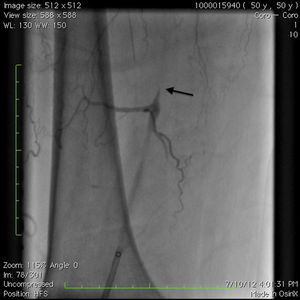
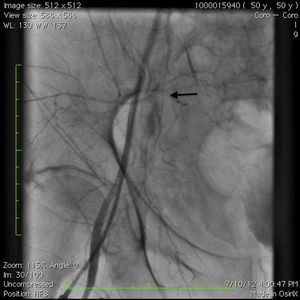
An angiogram from the left femoral sheath at this time showed retrograde filling of the distal and proximal SFA (Figure 4) and then the dissection plane in the EIA with a wire tip perforation and bleeding (Figures 5 and 6) to the retroperitoneal region at the external iliac artery with displaced bladder (Figure 6). Protamine was given to reverse the heparin and a 7-minute balloon inflation was performed in the distal SFA using a 5.0 mm×40 mm Evercross balloon (ev3, Plymouth, MN) to stop the retrograde bleeding. On repeat angiography, the distal SFA CTO was reoccluded and the dissection plane appeared to be sealed, with no further bleeding into the retroperitoneal region (Figures 7 and 8). Other than mild nausea after protamine, the patient reported no major symptoms during this procedure. When activated coagulation time was 130 s, the femoral and popliteal sheaths were removed. A 3-g/dl drop in hemoglobin was noted after the procedure that remained stable over the next two days. Popliteal and pedal pulses were palpable and unchanged following the procedure.
A retrograde popliteal approach to SFA occlusions was first described by Tonnesen et al. in 1988.5 Since then, this approach has proved a useful alternative for angioplasty of some SFA occlusions, indications being occlusion of the SFA origin, adverse collateral anatomy, and other difficulties in obtaining access to the common femoral artery.10 Complications involving this approach are usually infrequent according to prior reports.5,6,10–12 Since this approach has been increasingly used recently and little is known about potential complications during this procedure, we decided to report our experience and the management strategies we adopted in treating the complications described. Retrograde dissections and perforation during a popliteal approach may be benign when there is no retrograde flow, but as seen in our case, after wiring and advancement of support catheters inside the CTO retrograde flow can be established, especially with a partially obstructive popliteal sheath and lack of antegrade flow from the proximal end of the occlusion. In the case reported, if we had been able to establish antegrade flow by accessing the true lumen proximally, we could also have stopped the retrograde filling. During all this time the patient was in a prone position and the balloon was advanced through the popliteal sheath and inflated at the distal SFA to stop retrograde filling. The other option could have been to turn the patient to a supine position and to inflate the balloon in the proximal EIA, stopping the blood flow to the profunda femoris and collaterals to the popliteal and subsequently to the dissection plane. This approach would have taken longer and would have been physically more difficult for the patient.
ConclusionOur case report illustrates a dangerous complication that can occur during an intervention on an occluded SFA via a popliteal approach when the artery is partially recanalized and retrograde flow is present. Occasional cine angiograms after wiring the lesion (especially if there is any sign of bladder displacement) and once the presence of retrograde flow is established avoiding wires that may increase the chance of perforations, staying below the common femoral artery level, may decrease the risk of retroperitoneal hematoma. Balloon positioning and inflation at the distal SFA through the popliteal sheath will effectively stop the retrograde filling and can be used in such cases in the absence of antegrade filling of the perforation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.