Coronary artery aneurysms are uncommon but potentially hazardous entities found on a small percentage of coronary angiograms. The best management strategy remains to be determined; the coexistence of obstructive coronary artery disease is the main determinant of prognosis.
We report the case of a middle-aged woman with mixed aneurysmal and obstructive coronary artery disease presenting as an acute myocardial infarction, probably due to atherosclerosis. The unusual severity and complexity of the angiographic presentation of this case, with involvement of all major coronary arteries, raises important issues in terms of the patient's treatment options.
Os aneurismas das artérias coronárias são entidades raras, presentes numa pequena percentagem das angiografias coronárias, embora associadas a complicações potencialmente graves. A melhor conduta no tratamento destas situações ainda não foi estabelecida e a coexistência de doença coronária obstrutiva é o principal determinante prognóstico.
Reportamos o caso de uma mulher de meia-idade com doença coronária mista, obstrutiva e aneurismática, diagnosticada no contexto de enfarte agudo do miocárdio e de provável etiologia aterosclerótica. A gravidade e a complexidade incomuns da apresentação angiográfica do nosso caso, levantaram aos autores questões importantes no domínio da decisão terapêutica.
Coronary artery aneurysms (CAA) are uncommon entities found on a small percentage of coronary angiograms (0.3%–4.9%).1 They may be single or multiple, associated with stenotic coronary disease or not, symptomatic or asymptomatic, and may lead to serious complications. The best management strategy for coronary artery aneurysms has not been established and prognosis appears to be directly related to the severity of the concomitant obstructive coronary artery disease.2
The purpose of this case report is to highlight the clinical presentation, work-up and treatment options for a patient with mixed aneurysmal and stenotic coronary artery disease involving all three major coronary arteries.
Case reportA 52-year-old Caucasian woman with a history of hypertension and glaucoma presented at our emergency department with persistent chest pain for a few hours. The pain occurred during rest, radiated to the left arm and was accompanied by profuse sweating. The patient had no personal or family history of injury, connective tissue disease, or rheumatic fever. The physical examination was unexceptional.
Laboratory exams performed on admission to the hospital showed no abnormalities.
A 12-lead electrocardiogram (ECG) showed sinus rhythm, heart rate 43 bpm, poor progression of R wave in the precordial leads, ST depression in leads V3 to V6 and inverted T waves in leads V1 to V4.
Troponin I levels were initially negative, but rose during the course of the patient's hospitalization, reaching a maximum of 23.76 ng/ml.
The patient was admitted to intensive care and was started on aspirin, clopidogrel, unfractionated heparin and a statin. Soon after admission, electrical instability developed (ectopic ventricular beats with R on T phenomena and nonsustained ventricular tachycardia episodes) and urgent coronary catheterization was performed.
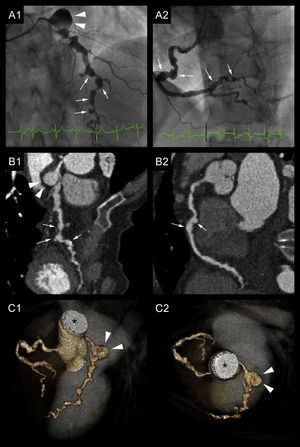
Coronary angiograms revealed a large aneurysm involving the origin of the circumflex artery, with a maximum diameter of 16mm, and irregular enhancement in the periphery with thrombus (Video 1 and Figure 1A1). The distal bed of the circumflex artery was very poorly perfused by collaterals of the right coronary artery. The left anterior descending artery also showed multiple saccular aneurysms and multilevel stenosis up to 70% with poor distal run-off (Videos 1 and 2 and Figure 1A1). The right coronary artery presented mild diffuse ectasia, multiple aneurysms and significant stenosis in the mid and distal portions (Video 3 and Figure 1A2). An aortogram with runoff showed a normal thoracic aorta.
Abnormal coronary artery appearance in different techniques. A large aneurysm (arrowheads) is seen at the distal edge of the left main trunk (A1, B1, C1 and C2). The left anterior descending artery (LAD) presents several aneurysms (arrows) but also severe stenotic lesions (resembling a string of beads) with a poor distal bed (A1, B1 and C1). Note the absence of circumflex artery visualization. The ectatic right coronary artery (RCA) also presenting aneurysmal formations (arrows) and obstructive lesions (A2, B2 and C2). A: coronary angiograms of the LAD and RCA. B: curved planar reformation (CPR) in multislice computed tomography (MSCT) of the LAD and RCA. C: Three-dimensional MSCT reconstructions (volume-rendering technique). *: ascending aorta.
Multislice computed tomography (MSCT) confirmed the appearance of the coronary arteries resembling a string of beads due to the presence of multiple aneurysms interspersed with critical stenotic lesions (Figure 1B and C). No other cardiac abnormalities were detected.
A two-dimensional echocardiogram revealed ejection fraction of 45% with lateral and posterior hypokinesis, left atrial enlargement (area 21 cm2) and minor valvular abnormalities.
Renal and liver function tests were normal, and those for other inflammatory markers, rheumatoid factor, venereal disease, cryoglobulin, complement activity, antiphospholipid antibodies, antinuclear antibodies, extractable nuclear antigens, and antineutrophil cytoplasmic antibodies were negative, as were tests for hepatitis B and C and human immunodeficiency virus. Coagulation inhibitor system function was normal.
MSCT of our patient indicated no other malformation of arteries in the head, trunk, or extremities.
After consultation with a multidisciplinary team that included a cardiothoracic surgeon, an interventional cardiologist and the attending cardiologist, any interventional treatment for our patient was deemed too high-risk. A surgical approach was hampered by the severity of obstructive coronary disease and the absence of suitable vessels for bypass. Likewise, the multiplicity and complexity of the stenotic and aneurysmal lesions ruled out any percutaneous stenting or embolization. A conservative approach was unanimously decided upon, including maximization of antithrombotic therapy (double antiplatelet therapy and a vitamin K inhibitor) and anti-ischemic therapy (statin, ACE inhibitor, beta-blocker and nitrates).
The patient had an uneventful hospitalization and was discharged home on the fifth day. At the 12-month follow-up she was still asymptomatic.
DiscussionThe first pathologic description of a CAA was by Morgagni in 1761.3 It was first diagnosed by angiography by Munker and colleagues in 1958.4 CAA is defined as a segmental dilatation of the vessel, with a diameter ≥1.5 times (according to some authors, ≥2 times) that of an adjacent normal section. Ectasia is characterized by a more diffuse dilatation involving at least 50% of the vessel length. Coronary ectasia and aneurysm are thought to represent subsequent stages of a dilatative process. The right coronary artery is most frequently involved (40%–61%), followed by the left anterior descending coronary artery (15%–32%) and the left circumflex artery (15%–23%). Three-vessel or left main involvement is rare.5
Almost half of cases of CAA occur as a consequence of atherosclerosis. The next most common cause is congenital (20%–30%). Other causes include vasculitis (such as Kawasaki disease, Takayasu's arteritis and polyarteritis nodosa), systemic lupus erythematosus, connective tissue disorders, Ehlers–Danlos syndrome, Marfan syndrome, infections (such as narcotic emboli, syphilis and Lyme disease), trauma, cocaine abuse, as a complication of percutaneous transluminal coronary angioplasty, and of idiopathic origin.5
The exact pathogenic mechanism is unknown; possible contributory factors include genetic predisposition, traditional risk factors for coronary artery disease, direct arterial wall damage and abnormal vessel wall metabolism.6,7
The simultaneous presence of CAA and coronary artery disease in our patient, along with the presence of multiple aneurysms and involvement of more than one coronary artery, indicate atherosclerosis as the main cause. By contrast, congenital, traumatic, or dissecting aneurysms are mainly single.5
The clinical presentation of CAA is varied. Atherosclerotic aneurysms usually present with ischemic symptoms such as angina and myocardial infarction. They also portend life-threatening complications such as rupture, vasospasm, thromboembolism, compression of surrounding structures and, more rarely, fistulization into one of the cardiac chambers.6 These cases may present in extremis with tamponade, heart failure or even sudden death.
CAA are commonly associated with aneurysms of other locations, particularly aortic and iliofemoral.1
Coronary angiography is the gold standard in the diagnosis of CAA. MSCT is an excellent alternative diagnostic method, especially in determining the exact anatomy and its relation to adjacent structures.1
The best management strategy for CAA has not been defined. Medical, interventional and surgical strategies have been described, but an individualized approach is recommended according to the location of the aneurysm and the clinical context.8
Conservative therapy includes antiplatelet and anticoagulant agents to prevent thrombus formation in the aneurysm and distal embolization.8
Surgical treatment is preferred for symptomatic patients who have evidence of embolization from the aneurysm to the distal coronary bed and those with large aneurysms, to avoid potential complications. Surgery is also indicated in cases of CAA enlargement in serial angiographic measurements.9 Various surgical techniques can be applied, such as isolating or resecting the aneurysm and reconstructing the coronary course using an interposition graft, or maintaining distal coronary flow via concomitant coronary artery bypass grafting.10
Because of the severe atherosclerosis and absence of suitable arteries for bypass grafting, our patient was not considered a good surgical candidate.
Percutaneous treatment is a newer option and includes coil embolization and stenting. According to Szalat et al.,11 polytetrafluoroethylene-covered stents appear to be of value in patients with aneurysms smaller than 10mm in diameter as no cases of in-stent restenosis were reported in this group. Alternatively, drug-eluting stents reduce risk of in-stent restenosis; however, malapposition of such stents in aneurysmal segments increases risk of stent thrombosis, and may contribute to further aneurysm formation.12
The prognosis of CAA is directly related to the severity of the concomitant obstructive coronary artery disease. According to the Coronary Artery Surgery Study registry,2 there was no difference in five-year survival between patients with and without aneurysms who had obstructive coronary artery disease.
Our patient has remained asymptomatic with medical treatment alone, under close surveillance every three months.
ConclusionWe report the case of a middle-aged woman who presented with an acute myocardial infarction and had mixed aneurysmal and obstructive coronary artery disease. Several cases of coronary artery aneurysms have been published. Our case is unusually complex, with all three major coronary arteries involved by diffuse atherosclerotic disease presenting simultaneously in different forms: multiple aneurysms of varying sizes interspersed with critical stenotic lesions all along the coronary beds. The presence of coronary aneurysms per se is not an indication for surgical treatment. Rather, the severity of coexisting obstructive coronary artery disease is the principal factor in deciding whether to proceed with surgery in patients with CAA. However, surgical management of our patient was ruled out by the poor distal vessel runoff and a percutaneous approach was also considered impracticable.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.