Loeffler's endocarditis is an acute form of primary restrictive cardiomyopathy. We report the case of a young woman with pleuritic chest pain associated with fever and hypereosinophilia. She was hospitalized with suspected acute myopericarditis and was treated with aspirin, leading to clinical improvement. Ten days after discharge, she was rehospitalized due to recurrence of chest pain. The echocardiogram showed what appeared to be a mass filling the apex of the right ventricle (RV). She was referred for magnetic resonance imaging, which revealed marked myocardial thickening in the apex of the RV. The patient underwent an endomyocardial biopsy, resulting in a diagnosis of eosinophilic endocarditis. After treatment with prednisolone, all symptoms and the eosinophilia disappeared, and there was complete remission of the RV abnormalities. After three years of follow-up, the patient remains asymptomatic. This case shows that, even without an etiologic diagnosis of eosinophilia, the prognosis for Loeffler's endocarditis can be favorable if treatment is initiated early.
A endomiocardite de Löffler é uma miocardiopatia restritiva primária aguda. Relatamos o caso clínico de uma jovem que inicia dor torácica pleurítica associada a febre e hipereosinofilia. Internada por suspeita de miopericardite aguda e submetida a tratamento com ácido acetilsalicílico, verificou-se melhoria clínica. Dez dias após a alta é reinternada por recorrência da dor. O ecocardiograma mostrou uma aparente massa ocupando o apex do ventrículo direito (VD). Referenciada para ressonância magnética cardíaca, esta demonstrou um marcado espessamento do miocárdio no apex do VD. Foi submetida a biópsia endomiocárdica que diagnosticou uma endomiocardite eosinofílica. Após o início do tratamento com prednisolona, verificou-se o desaparecimento da sintomatologia, da eosinofilia e uma regressão completa das alterações no VD. Ao fim de 3 anos de seguimento mantém-se assintomática. O caso descrito revela que o prognóstico da endomiocardite de Löffler, mesmo sem um diagnóstico etiológico da eosinofilia, poderá ser favorável, se o tratamento for iniciado precocemente.
The most common cardiac manifestation of hypereosinophilic syndrome is Loeffler's endocarditis, an acute form of primary restrictive cardiomyopathy resulting from sustained overproduction of eosinophils and infiltration of tissues. Ideally, treatment should be directed at the cause of the hypereosinophilia but this remains unknown in most cases. The condition has a poor prognosis.
Case reportA 34-year-old woman, a doctor, had a personal history of pulmonary tuberculosis at age 14, bronchial asthma and eosinophilia (400–2200/mm3) diagnosed in 2000, and sinusitis with nasal polyposis operated in 2005. She was routinely medicated with fluticasone, salmeterol and salbutamol inhalers.
In April 2008, she began experiencing intermittent pleuritic pain at the level of the left scapula associated with dry cough and asthenia. An initial diagnosis of respiratory infection was made, but two courses of antibiotic therapy (azithromycin and levofloxacin) produced no improvement. Investigation of the setting at this time included ECG and transthoracic echocardiography (TTE), which revealed no abnormalities. The pain was therefore assumed to be of muscular origin, and the symptoms were treated with paracetamol and anti-inflammatory drugs. At the end of June, the pain worsened and the patient developed a fever, but physical examination revealed no significant changes. The ECG showed new-onset incomplete right bundle branch block, poor R-wave progression in V1–V3 and negative T waves in V1–V5. Laboratory tests revealed leukocytosis (13 500/mm3) with 50% eosinophils (6800/mm3, normal <400), and elevated IgE (515IU/ml, normal <88), troponin I (1.2ng/ml, normal <0.1), BNP (158pg/ml, normal <100) and CRP (321mg/dl, normal <5). The chest X-ray showed a small left pleural effusion, with no pulmonary parenchymal alterations, and increased cardiothoracic index. TTE revealed non-dilated cardiac chambers and good left (LV) and right ventricular (RV) global and regional systolic function. The cardiac valves showed no significant morphological or functional abnormalities. There was pericardial thickening, with a moderate circumferential effusion (12mm in parasternal long-axis view), but no hemodynamic compromise (Figure 1).
The patient was hospitalized on July 14, 2008 with a diagnosis of myopericarditis. Treatment was begun with aspirin in anti-inflammatory doses and opioid analgesics, which brought some pain relief. Laboratory tests showed a reduction in troponin I, CRP and BNP levels, while TTE showed reduced pericardial effusion and persistence of pericardial thickening. Given her persistently high eosinophil count, even for a patient with asthma, and the coexistence of a left pleural effusion, other diagnostic hypotheses besides acute viral myopericarditis included: (a) recurrence of pulmonary tuberculosis, (b) helminthiasis, (c) hypereosinophilic syndrome, and (d) Churg-Strauss syndrome. Immunological study including ANA, ANCA and rheumatoid factors was negative; direct examination of expectoration was negative for BK virus; stool cultures were negative for eggs, cysts and parasites, as was serology for CMV IgM, EBV and herpes simplex 1 and 2 antibodies, influenza A and B, adenovirus, echovirus and Coxsackie virus. Thoracic computed tomography showed a small left pleural effusion. The patient was discharged on July 16, 2008, reporting only mild left back pain on breathing deeply and medicated with aspirin 1000mg every eight hours.
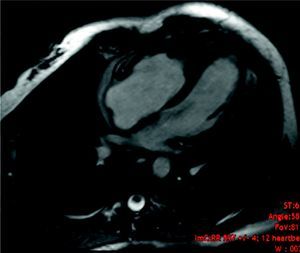
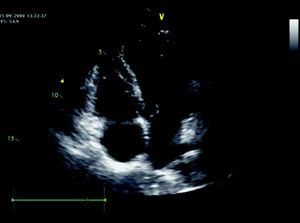
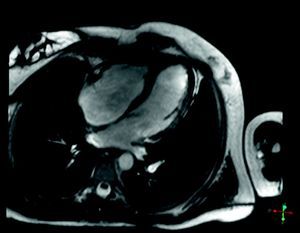
Ten days after discharge, the patient experienced recurrence of chest pain, with no fever. Control TTE showed RV apical hypokinesia and an apical mass of the same signal intensity as the myocardium with no cleavage plane between the mass and the myocardial wall (Figure 2). Pericardial thickening persisted with a moderate effusion. In the light of the new findings, the RV mass was considered to be a thrombus or tumor, or to be secondary to hypereosinophilic syndrome. Oral anticoagulation with warfarin was begun given the suspicion of a thrombus and the patient was transferred to Coimbra University Hospital for cardiac magnetic resonance imaging (CMRI) and endomyocardial biopsy (EMB). CMRI revealed marked thickening of the RV apex, of infiltrative appearance (Figure 3). Delayed enhancement showed heterogeneous areas of hyperintense signal in the RV apex, septal wall and LV apex, some of which had a subepicardial distribution. EMB revealed fragmentation of muscle bundles by eosinophils, with myocyte destruction and coagulation necrosis, compatible with eosinophilic endocarditis. The diagnosis of Loeffler's endocarditis was therefore established and treatment begun with oral prednisolone (1mg/kg/day), anticoagulation with warfarin being continued. During follow-up, the patient was completely free of pain, her eosinophil count normalized and the RV myocardial thickening disappeared (Figure 4), confirmed by CMRI (Figure 5). Anticoagulation was maintained for three months and corticosteroid therapy for six months. She subsequently had one episode of sustained back pain without hypereosinophilia or echocardiographic alterations, and was treated with corticosteroids for four weeks. The patient has been evaluated every six months by ECG, laboratory tests and TTE, and three years after beginning treatment, control CMRI shows her to be in complete remission.
In the case presented, the possibility of Loeffler's endocarditis was considered given that the patient had eosinophilia and a mass in the RV apex, which CRMI showed to be a myocardial infiltrate, the diagnosis being confirmed by EMB. Besides asthma, which is not usually associated with such high eosinophil counts, hypereosinophilia can have many causes, the most common being autoimmune disease, rheumatoid arthritis, parasitic infection and eosinophilic leukemia.1 Immunological study performed during the patient's first hospitalization excluded the first two hypotheses. She had no contact with animals and had not recently traveled abroad, no causative agent was isolated from stool cultures, and clinical improvement was observed with anti-inflammatory drugs, thus excluding parasitic infection. No bone marrow biopsy was performed to exclude eosinophilic leukemia, but the improvement observed with corticosteroid therapy does not support this hypothesis. Although ideally treatment should be directed at the cause of hypereosinophlia,2 when there is no etiological diagnosis, studies have shown regression of myocardial infiltrate with corticosteroids.3,4 Warfarin was initially maintained due to the association between Loeffler's endocarditis and embolic events.1 The effect of anti-inflammatory and immunosuppressive therapy with corticosteroids and cytotoxic agents varies, but cases of hypereosinophilic syndrome with acute manifestations tend to respond better.5,6 While prognosis is generally poor, rapid resolution with corticosteroid therapy has been described.3,4
ConclusionLoeffler's endocarditis is a rare entity, and TTE and CMRI play a crucial role in its diagnosis. Ideally treatment should be directed at the cause of hypereosinophilia but this remains unknown in most cases, resulting in poor prognosis. The case presented shows that in some patients, even without an etiologic diagnosis of eosinophilia, the prognosis of Loeffler's endocarditis can be favorable if treatment is initiated early.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Faria R. Endomiocardite de Löffler - a propósito de um caso clínico. Rev Port Cardiol 2012; doi:10.1016/j.repc.2012.04.003