A 50-year-old man with a history of drug addiction was admitted to the cardiology department for aortic valve fungal endocarditis complicated by severe aortic regurgitation, cerebral infarcts and right common iliac artery pseudoaneurysm. While awaiting transfer to the cardiothoracic surgery department, the patient presented acute arterial ischemia of the left leg, and distal left patellofemoral embolectomy was successfully performed. The patient was then transferred to the cardiothoracic center and the aortic valve was replaced by a bioprosthetic valve. After 14 days he was referred for vascular surgery, where the four-month hospitalization was complicated by left leg amputation. Four months after discharge, the patient was admitted to the emergency department for recurrent fungal endocarditis complicated by multiple renal and splenic infarcts and celiac trunk embolization. He was transferred to the cardiothoracic surgery department, but suffered cardiac arrest before surgical intervention.
Doente do género masculino, de 50 anos de idade, ex-toxicodependente, admitido no serviço de Cardiologia por endocardite fúngica da válvula aórtica complicada de insuficiência aórtica severa, enfartes cerebrais e pseudoaneurisma da artéria ilíaca comum direita. Enquanto aguardava transferência para o serviço de cirurgia cardiotorácica, o doente apresentou isquemia arterial aguda do membro inferior esquerdo, tendo realizado tromboembolectomia femuro-distal esquerda. Posteriormente, foi submetido à substituição da válvula aórtica por prótese biológica. Após catorze dias de internamento foi internado no serviço de Cirurgia Vascular, tendo o internamento de 4 meses sido complicado com amputação da perna esquerda. Quatro meses após a alta, o doente recorreu ao serviço de urgência por febre e dor abdominal. Foi-lhe diagnosticada recorrência de endocardite fúngica complicada por enfartes esplénicos e renais e êmbolo no tronco celíaco. O doente foi transferido de urgência para o serviço de Cirurgia Cardiotorácica. Antes da intervenção cirúrgica apresentou paragem cardiorrespiratória.
Fungal endocarditis is a rare entity with high mortality even with combined medical and surgical treatment.1–4 Risk factors include previous valve surgery and antibiotic therapy, intravenous drug use, intravascular catheter placement and immunosuppression.3,4Candida spp. are the most frequent etiological agents. Early surgical intervention immediately after initiation of antifungal therapy, particularly amphotericin B, is the treatment of choice.1,4 Recurrence is common; rates of 30–40% have been reported.3
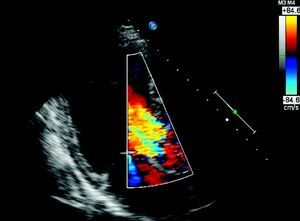
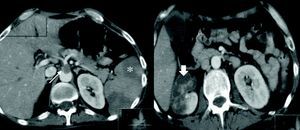
Case reportA 50-year-old man with a history of smoking, drug addiction and chronic hepatitis C went to the emergency department with asthenia, fever and headache of one month's evolution and abdominal pain for two days. On physical examination he presented fever; cardiac auscultation revealed a loud decrescendo diastolic murmur, grade III/VI, at the left sternal border; there were no signs of heart failure. Laboratory tests revealed acute renal failure (creatinine 2.5mg/dl and urea 60mg/dl compared to normal values one week previously), elevated C-reactive protein (77.5mg/l) and normocytic normochromic anemia (Hb 11.2g/dl). Abdominal computed tomography (CT) showed splenomegaly without visible infarcted areas and right hydrouretonephrosis caused by an aneurysm of the right common iliac artery (42mm maximum diameter). Transthoracic echocardiography (TTE) revealed a 15-mm vegetation on the non-coronary leaflet of the aortic valve (Figure 1) and severe aortic regurgitation (Figure 2), together with moderate to severe left ventricular systolic dysfunction (ejection fraction 35%); these findings were confirmed by transesophageal echocardiography. The patient was admitted to the cardiology department, where empirical antibiotic therapy was begun with vancomycin and meropenem; it was decided not to add an aminoglycoside due to his low glomerular filtration rate, estimated at 20ml/min/1.73m2. On the second day of hospital stay he showed signs of cognitive slowing, with no focal neurological alterations; subsequent cerebral magnetic resonance imaging (MRI) showed multiple recent cerebral infarcts. Amphotericin B-susceptible Candida albicans was isolated from blood cultures; antifungal therapy was begun and the surgical center was contacted in order to transfer the patient for aortic valve replacement. While awaiting transfer, he suddenly suffered intense pain, coolness and loss of pulses in his left leg due to acute ischemia, probably caused by cardioembolism from the fungal vegetation. He was transferred urgently to a vascular surgery center where distal left patellofemoral embolectomy was successfully performed. The patient was then transferred to the cardiothoracic center and the aortic valve was replaced by a bioprosthetic valve. Microbiological analysis of the aortic valve and the embolus removed from the left femoral artery revealed C. albicans. Postoperative TTE showed normal aortic prosthetic valve function and after 14 days the patient was transferred to the cardiology department of our hospital. During hospitalization he presented fever and elevated inflammatory markers; repeat TTE confirmed normal prosthetic valve function, with no evidence of vegetations. MRI of the abdomen and lower limbs detected a large pseudoaneurysm of the right iliac artery, the external iliac artery being occluded distal to the pseudoaneurysm, multiple swellings compatible with abscesses in the left groin and thigh (the access site for the previous vascular surgery), and abscesses in the anterolateral muscle compartment of the left leg (Figure 3). In view of the existence of a focus of infection and the absence of evidence of endocarditis on TTE, it was decided not to perform transesophageal echocardiography. The patient was transferred to the vascular surgery department, where he underwent total aneurysmectomy with femoro-femoral crossover bypass using an inverted right greater saphenous vein graft, together with exploration and drainage of the abscesses in the left leg. Microbiological study of the pseudoaneurysm revealed Staphylococcus epidermidis. During hospitalization in the vascular surgery department intermittent fever persisted and the patient's general condition progressively deteriorated. S. epidermidis was detected in repeat blood cultures and broad-spectrum antibiotic therapy was begun with vancomycin and meropenem. CT of the pelvis and thighs revealed two new pseudoaneurysms, in the left internal iliac artery and the left superficial femoral artery. The patient underwent further surgery, during which it became clear that the clinical situation had progressed rapidly, with rupture of the left femoral pseudoaneurysm and extensive hemorrhagic infiltration and abscesses in the thigh. The left internal iliac and left superficial femoral arteries were ligated and devitalized tissue and purulent collections were thoroughly debrided. Late in the procedure it was decided to proceed to open transfemoral amputation of the leg, due to gangrene. The patient remained in the vascular surgery department for four months, during which antifungal therapy was maintained; transfemoral reamputation was performed and surgical debridement of abscesses in the stump were required on several occasions. After partial closure of the residual limb he was discharged, clinically stable; it was decided not to continue antifungal therapy due to its possible hepatic toxicity and the patient's chronic hepatitis C.
Four months after discharge, the patient was admitted to the emergency department with fever and abdominal pain. Abdominal CT revealed multiple renal and splenic infarcts and celiac trunk embolization (Figure 4). TTE showed an 8-mm vegetation on the aortic prosthesis and moderate aortic regurgitation. He was transferred to the cardiothoracic surgery department for emergency surgery, but suffered cardiac arrest before reaching the operating room. Blood cultures from the emergency department revealed the presence of C. albicans.
DiscussionFungal endocarditis tends to affect relatively young patients, with a mean age of 40 years, although those with prosthetic valve endocarditis may be older.2,5 The characteristic echocardiographic feature is the presence of large vegetations, which carry a high risk for central and peripheral embolization. The most common complications are embolization (which can lead to occlusion of the limb arteries), neurological alterations and heart failure.1 Early surgical intervention, immediately after beginning antifungal therapy, is the treatment of choice.
There is a lack of clear recommendations in the literature concerning the best antifungal therapy, and in particular its duration.
Although rare, fungal infection of prosthetic valves is more common than of native valves; Candida spp. are most often involved. Boland et al., of the Mayo Clinic, presented a 40-year series of fungal prosthetic valve endocarditis, with 21 cases and mortality of 57%. C. albicans was isolated in most cases; the majority of patients were immunocompetent. The aortic valve was most frequently affected, with 43% of patients presenting endocarditis a year after valve implantation. All patients received antifungal therapy, 95% of them with amphotericin B.5
One of the first prospective studies on endocarditis was by Falcone et al., an Italian multicenter study including 903 patients. Candida endocarditis was diagnosed in 15 cases; two-thirds were treated with caspofungin alone or in combination with other antifungals. Evidence that amphotericin B fails to penetrate well into clots and vegetations, and hence has lower in vivo activity than predicted by in vitro testing, compared to the greater activity of caspofungin, means that the latter is a more promising antifungal. According to a meta-analysis by Steinbach et al., this study also showed that whichever antifungal is used, the cornerstone of treatment for fungal endocarditis is early surgery.6
More recently, in a meta-analysis on the role of fluconazole in patients who are not eligible for valve replacement, Smego et al. concluded that fluconazole in isolation is associated with a high rate of recurrence or death (42%) and should therefore not be used alone; however, when used in conjunction with another antifungal it led to clinical improvement in 88% and 68% of patients with fungal endocarditis of native and prosthetic valves, respectively. In this meta-analysis the best results were obtained with chronic suppressive therapy with fluconazole for at least six months.7
The 2009 guidelines of the Infectious Diseases Society of America recommend surgical valve replacement in cases of Candida endocarditis in association with antifungal therapy, specifically liposomal amphotericin B (3–5mg/kg/day) with or without flucytosine (25mg/kg 4 times daily), or amphotericin B deoxycholate (0.6–1mg/kg/day) with or without flucytosine, or an echinocandin (e.g., caspofungin 50–150mg/day); treatment should continue for at least six weeks after valve replacement and for longer in patients with perivalvular abscesses or other complications. For patients who cannot undergo valve replacement, long-term suppression with fluconazole at a dosage of 400–800mg (6–12mg/kg) daily is recommended. For prosthetic valve fungal endocarditis, the same recommendations apply, and suppressive therapy should be lifelong if valve replacement is not possible.8
In the case presented, it was decided not to prolong antifungal therapy due to the high risk of hepatic toxicity in a patient with known liver disease.
ConclusionsFungal endocarditis is a rare disease, although its incidence is increasing, with high mortality. Treatment is based on early surgical intervention together with a long course of antifungal therapy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ribeiro, S, et al. Endocardite fúngica com embolização central e periférica: um caso clínico. Rev Port Cardiol. 2012. doi:10.1016/j.repc.2011.12.019.