Anomalous origin of coronary arteries represents a clinical challenge because of the anatomical variability and possible functional consequences, the pathophysiological mechanisms involved, and the lack of large published series that would provide evidence to guide the clinical and therapeutic approach. The authors describe the case of a 55-year-old male patient with a long history of atypical chest pain who was considered to have a low to intermediate likelihood of coronary artery disease. Therefore, and also bearing in mind his physical limitations (congenital left leg atrophy), he was referred for cardiac CT to rule out coronary artery disease. The exam showed a left coronary artery arising from the right coronary cusp and with an interarterial course, between the aorta and pulmonary trunk. Although this is a potentially malignant anatomical variant with surgical indication, a conservative approach was chosen, considering the late diagnosis and particular risk-benefit profile.
A origem anómala das artérias coronárias constitui um importante desafio clínico pela variabilidade anatómica, possíveis repercussões funcionais, mecanismos fisiopatológicos implicados e também pela ausência de grandes séries na literatura que forneçam sólida evidência científica para a sua orientação clínica e terapêutica.
Os autores descrevem o caso de um doente de 55 anos, com antecedentes de hipertensão, dislipidemia e atrofia congénita da perna esquerda, que se apresentou com quadro de dor retroesternal atípica com um ano de evolução. Tendo em conta os fatores de risco cardiovasculares e exames complementares de diagnóstico previamente realizados, considerou-se ser um doente com probabilidade baixa a intermédia de doença coronária. Assim, e pela sua limitação funcional, realizou angioTC cardíaca que revelou uma origem anómala da coronária esquerda na cúspide coronária direita e com trajeto entre a aorta e a artéria pulmonar. Embora esta seja uma variante anatómica com potencial evolução maligna, optou-se por uma atitude conservadora após ponderação do risco-benefício no contexto clínico deste doente.
Coronary artery anomalies are the third leading cause of sudden death in young athletes1; their incidence in healthy individuals is estimated at 0.3–1%.2
Various different anomalies have been described, and classifications have been proposed based on anatomy (anomalies of origin, course and termination) and on prognosis (with or without clinical significance).2 With regard to the latter, most anomalies have no clinical significance and thus require no specific treatment.3
However, congenital coronary artery fistulas, myocardial bridging and anomalous origin in the pulmonary artery can be associated with malignant evolution.
Another potentially serious anomaly is origin of a coronary artery from the contralateral coronary sinus, which can lead to myocardial ischemia and sudden death when it courses between the aorta and pulmonary artery (interarterial course). Other courses—retroaortic, prepulmonary and subpulmonary, and septal—are considered benign.4,5
Origin of the left coronary artery in the right sinus of Valsalva is rare, with an estimated incidence of 0.09–0.11% in patients undergoing coronary angiography,6 but it is frequently associated with sudden cardiac death during intense physical activity and in adolescents and young adults, half of whom were previously asymptomatic.7,8 An interarterial course is seen in most of these patients9; their poor prognosis may be due to the acute angle of the artery from the ostium, stretching of the intramural segment, or compression between the commissure of the right and left coronary cusps.5
Cardiac CT angiography is a recent and valuable complementary exam that has high spatial resolution and provides three-dimensional views of the coronary arteries, with better definition of their origin and proximal portion, course, and relations with other cardiac structures than conventional angiography.10 The increasing popularity of this technique has greatly improved detection of coronary artery anomalies, which has made clinical decision-making more difficult, since there is, and is unlikely to be, sufficient evidence on which to base therapeutic strategies in doubtful cases such as the one presented.
Case reportA 54-year-old male patient was assessed in the cardiology outpatient clinic for atypical chest pain of about one year's evolution. He reported no other relevant cardiovascular symptoms, including fatigue, dyspnea, palpitations or syncope.
His cardiovascular risk factors included hypertension and dyslipidemia; he also had congenital left leg atrophy. He was medicated with simvastatin, propanolol, candesartan and aspirin.
The electrocardiogram showed sinus rhythm with incomplete right bundle branch block but no other significant alterations. He had undergone myocardial perfusion scintigraphy with adenosine a year before, which was negative for ischemia.
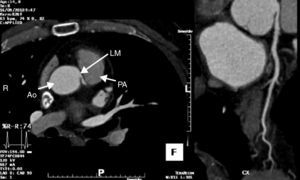
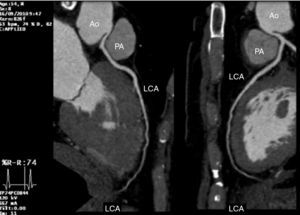
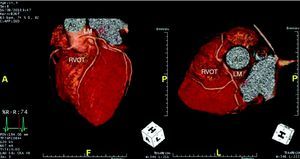
To clarify the clinical picture and since he was considered to have a low to intermediate likelihood of coronary artery disease, and also bearing in mind his physical limitations, he was referred for cardiac CT to rule out coronary artery disease. The exam showed a left coronary artery arising from the right coronary cusp and with an interarterial course, between the aorta and pulmonary trunk (Figures 1–3). No coronary plaque was detected and his calcium score was 0.
Given the clinical context of his age (54 years) and absence of typical angina or syncope, it was decided to perform ischemia testing. Although imaging exams such as dobutamine stress echocardiography, myocardial perfusion scintigraphy and magnetic resonance imaging have higher sensitivity and specificity for ischemia testing, treadmill exercise testing was chosen in order to determine the patient's actual maximum functional capacity. Beta-blocker therapy was suspended for the test.
The patient achieved maximal exercise (3min 12s with the Bruce protocol), reaching the maximum predicted heart rate with no angina or ST-segment alterations suggestive of ischemia, and with no arrhythmias. In the light of this result, it was decided to keep the patient under clinical surveillance with no referral for cardiac surgery.
DiscussionAlthough there is still disagreement on the subject, some guidelines recommend surgical coronary revascularization in patients with anomalous left coronary artery arising from the right sinus of Valsalva and coursing between the aorta and pulmonary artery (class I recommendation, level of evidence B in the ACC/AHA guidelines for the management of adults with congenital heart disease).11 When the right coronary has an anomalous origin, ischemia testing is recommended before referral for surgical correction (class I recommendation, level of evidence B).
However, this case had some unusual aspects: the patient was older than the age-group most affected; he had no symptoms that were unequivocally associated with anomalous origin of the coronary arteries, particularly typical exertional angina or history of syncope; and no ischemia was documented on exercise testing, in which the patient achieved the limit of his functional capacity (maximum predicted heart rate) without the effect of beta-blockers. The patient's congenital left leg atrophy may paradoxically have had a protective effect by preventing him from performing strenuous exercise, which can trigger malignant arrhythmias in this situation.
Therefore, considering all factors, it was decided that the risk-benefit ratio favored a conservative approach.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carvalho, S., et al. Origem anómala da coronária esquerda: variante interarterial maligna com evolução clínica benigna. Rev Port Cardiol 2012. doi:10.1016/j.repc.2011.11.010