Left ventricular aneurysm and pseudoaneurysm are two complications of myocardial infarction in which the role of imaging is paramount. The authors describe a case of a true aneurysm of the posterior wall, for which cardiac magnetic resonance was useful, although only intra-operative assessment confirmed the diagnosis.
Os aneurismas e pseudo-aneurismas do ventrículo esquerdo são 2 complicações do enfarte do miocárdio, onde as técnicas de imagem desempenham um papel fundamental. Os autores apresentam um caso clínico de aneurisma verdadeiro da parede posterior, em que a Ressonância Magnética cardíaca foi útil, embora apenas o exame intraoperatório tenha confirmado o diagnóstico.
Left ventricular aneurysm and pseudoaneurysm are two complications of myocardial infarction in which the role of imaging is paramount. Left ventricular free wall rupture is a catastrophic complication in 4% of patients after myocardial infarction and in 23% of associated deaths.1
Differential diagnosis between left ventricular aneurysm and pseudoaneurysm can be difficult. We present the case of a patient with a true aneurysm of the posterior wall, which illustrates the complementarity of non-invasive imaging techniques (echocardiography and magnetic resonance) in diagnosing these mechanical complications of myocardial infarction, as well as the difficulty in establishing a definitive differential diagnosis between the two entities.
Case reportAn 83-year-old man suffered an inferolateral ST-elevation myocardial infarction in October 2007, and underwent angioplasty of the circumflex artery with bare-metal stenting. Around 20 months after this episode, he was admitted to the emergency department due to ventricular tachycardia with hemodynamic repercussions (acute pulmonary edema and hypotension). After conversion to sinus rhythm, the ECG revealed only an inferolateral necrotic scar, with no other alterations. Clinical improvement was seen with medical therapy, including amiodarone, atenolol, furosemide, enoxaparin and captopril. Transthoracic echocardiography showed left chamber dilatation, moderate mitral regurgitation and left ventricular dysfunction, with ejection fraction of 41%.
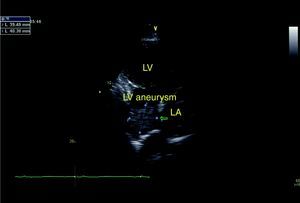
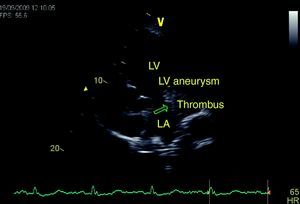
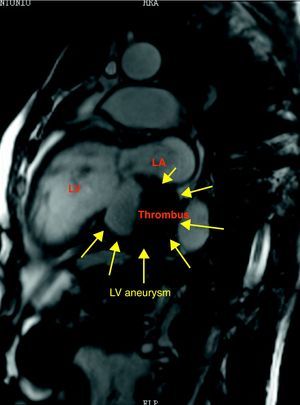
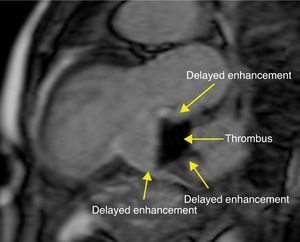
In view of the patient's dyspnea and recurrent chest pain, without new electrocardiographic alterations or elevation of myocardial necrosis markers, thoracic CT was performed, which showed a hypodense mass, apparently extracardiac, next to the left atrium. A second echocardiogram showed a mass (39mm×40mm) adjacent to the left atrium, but continuity with the cardiac chambers was not conclusively demonstrated (Figures 1 and 2). Subsequent cardiac magnetic resonance imaging revealed a large left ventricular inferobasal aneurysm, partly filled by a large thrombus (52mm×48mm×32mm). Given the thinness of the aneurysm wall, it was impossible to distinguish different layers, and so pseudoaneurysm with late presentation could not be definitively excluded. There was some flow between the thrombus and the aneurysmal sac, but the former appeared to be adhering to the upper and lower walls of the aneurysm (Figures 3 and 4). The exam also confirmed severe left ventricular dysfunction and mitral regurgitation due to changes in left ventricular geometry, with marked posterior leaflet tethering.
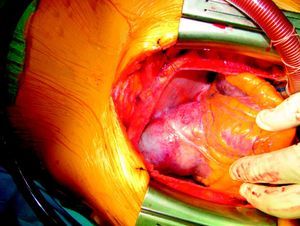
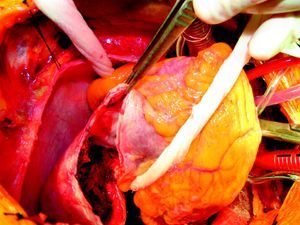
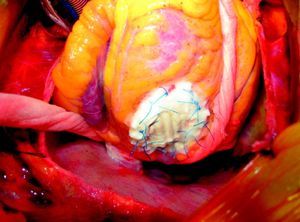
The patient was accordingly transferred to a surgical center, where coronary angiography revealed no significant new lesions. Intraoperative examination confirmed the presence of a true aneurysm of the left ventricular posterior wall. Thrombus resection and endocardectomy were performed, followed by closure with a Vascutek® tube graft (Figures 5–8). After three days in intensive care, the patient was discharged fifteen days later, clinically improved.
DiscussionDistinguishing between left ventricular aneurysm and pseudoaneurysm is difficult, particularly in the case of posterior aneurysms (3%).2,3 True aneurysms are defined as areas of thinner myocardium that are dyskinetic but contain all wall layers. By contrast, pseudoaneurysms result from free wall rupture, often contained by thrombus and adherent pericardium. The latter thus present a greater risk than true aneurysms, spontaneous rupture being the most serious complication since this generally results in sudden death. Differential diagnosis between the two entities is difficult since they have many characteristics in common, the diagnosis often being made during surgery.4 Thinned or ruptured myocardium moves dyskinetically or is non-contractile, leading to heart failure and malignant ventricular arrhythmias, which can occur with both entities.5 In the case presented, the detection of a mass adjacent to the left atrium by CT and echocardiography was a diagnostic challenge. Magnetic resonance imaging confirmed the presence of a thrombus associated with an aneurysm or pseudoaneurysm, but this technique also was unable to detect continuity in the myocardium. In true aneurysms, surgical intervention is aimed at improving left ventricular function through reverse remodeling, thus reducing the risk of malignant arrhythmias and embolic events, and improving survival for patients with this complication.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Aguiar, J; Aneurisma do ventrículo esquerdo e diagnóstico diferencial com pseudoaneurisma. Rev Port Cardiol 2012. doi:10.1016/j.repc.2012.04.001.