Trichosporon beigelii is a non-pathogenic fungus that can however become an opportunist agent of disseminating and potentially fatal infections, especially in immunocompromised patients. In the literature, there are only 11 published cases of infective endocarditis due to T. beigelii. Most of these cases involved immunocompetent individuals and the main risk factor was the presence of a prosthetic valve. The longest interval between surgery and endocarditis was eight years. In the present study, a case of prosthetic valve endocarditis due to T. beigelii is reported in an immunocompetent patient 11 years after mitral valve replacement. As with similar cases, low clinical suspicion and negative blood cultures delayed the beginning of antifungal therapy and cardiac surgery. Considering the high mortality and severity of T. beigelii endocarditis, it should be considered when there is a prosthetic valve infection with negative blood cultures, irrespective of the time elapsed since the previous surgery.
Trichosporon beigelii é um fungo não patogênico, que, entretanto, pode se tornar um agente oportunista de infecções disseminadas e potencialmente fatais, especialmente em pacientes imunossuprimidos. Na literatura, foram relatados apenas onze casos de endocardite infecciosa (EI) por T. beigelii, sendo a maioria dos indivíduos imunocompetentes, cujo único fator de risco era a presença de prótese valvar. O maior intervalo registrado entre a cirurgia e a endocardite foi de oito anos. No presente estudo, será relatado um caso de endocardite de valva protética por Trichosporon beigelii em paciente imunocompetente, onze anos após troca valvar mitral. Como nos demais relatos, a baixa suspeição clínica e hemoculturas negativas levaram ao atraso no início da terapia antifúngica e cirurgia cardíaca. Devido à alta gravidade e mortalidade da endocardite por Trichosporon beigelii, este relato de caso sugere que a mesma deve ser considerada nos casos de infecção de valva protética, mesmo com hemoculturas negativas, independentemente do tempo da intervenção.
Trichosporon beigelii is a non-pathogenic fungus that causes superficial infections such as white piedra.1 Systemic infection is rare but is much more serious, with mortality approaching 80%.2
Eleven cases of infective endocarditis (IE) due to T. beigelii have been reported.1–11 Most were in immunocompetent patients whose only risk factor was the presence of a prosthetic heart valve. Of these 11 cases, nine presented endocarditis on a prosthetic valve,1,3,5–11 in five of which the prosthetic mitral valve was affected.1,7–11
The longest interval between surgery and IE of a prosthetic valve reported in the literature was eight years. In the present study, a case of prosthetic valve IE due to T. beigelii is reported in an immunocompetent patient 11 years after valve replacement.
Case reportA 57-year-old man with a bioprosthetic mitral valve implanted 11 years previously was admitted with a history of high fever and chills in the previous 15 days. He denied intravenous drug abuse, diabetes, malignancy or other immunosuppressive conditions. On physical examination he was febrile (axillary temperature 38.4°C), with blood pressure of 125/78mmHg and heart rate of 118bpm. Cardiovascular assessment showed regular heart rhythm, normal heart sounds and a significant systolic murmur in the mitral focus. The rest of the examination was normal.
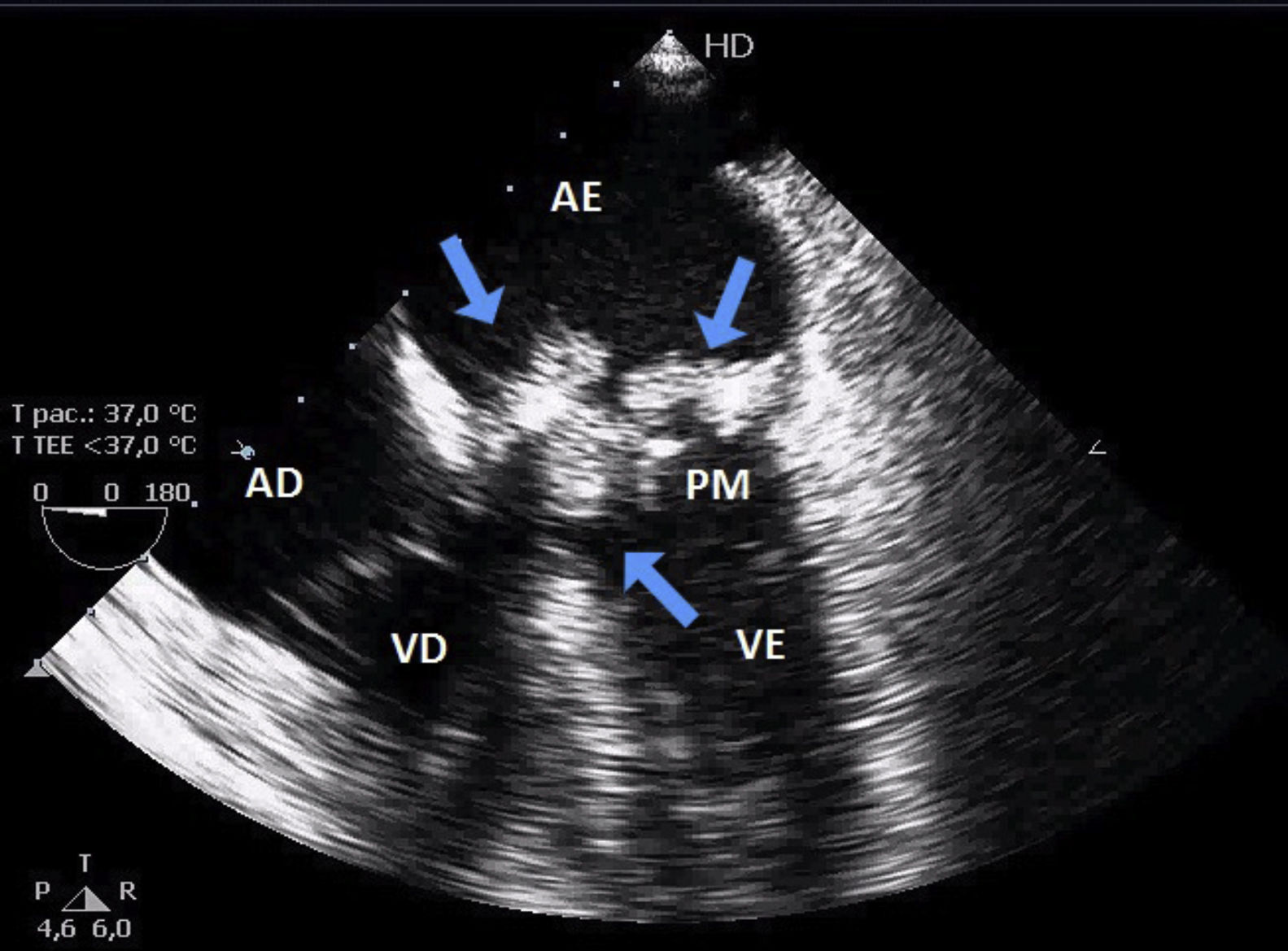
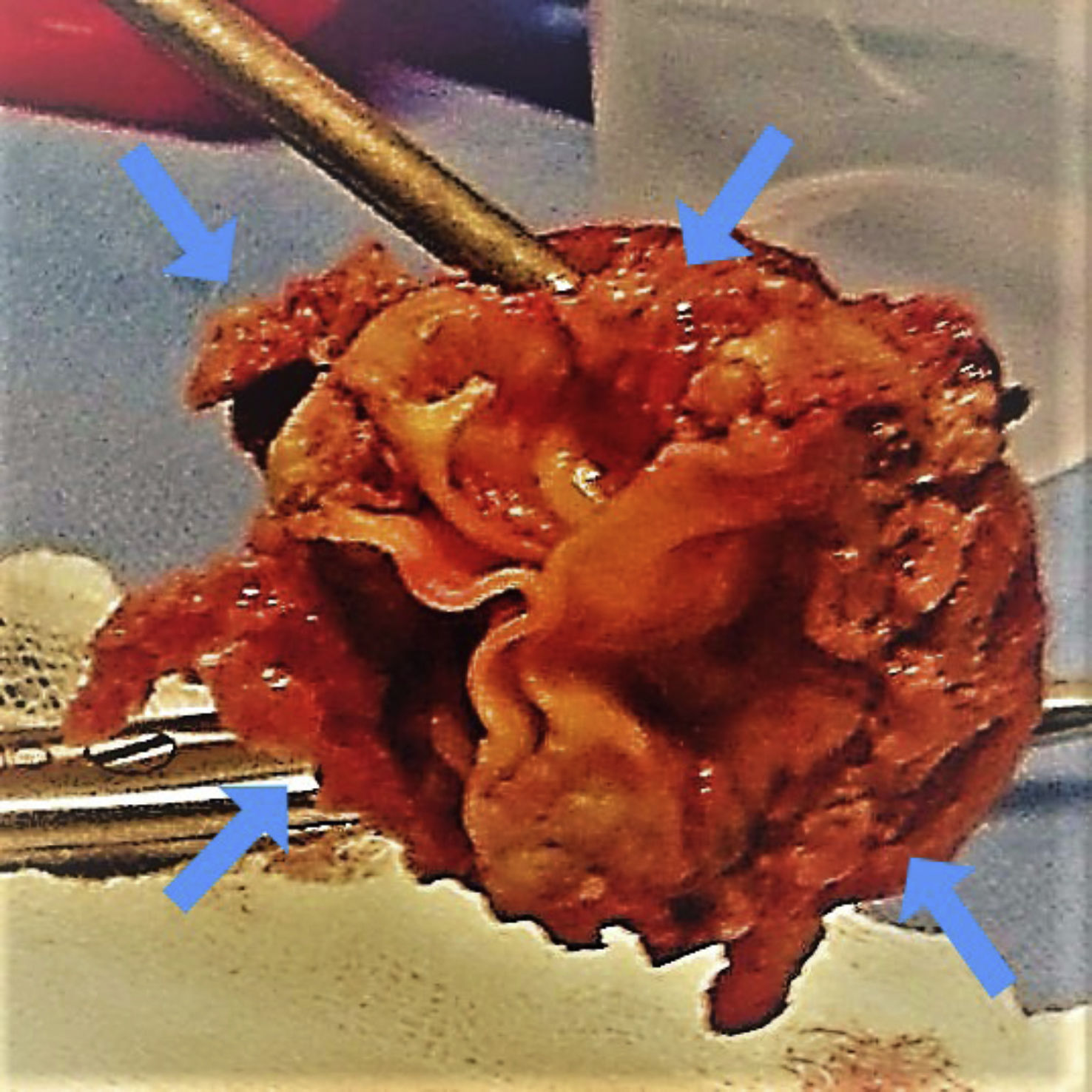
Laboratory tests showed slight leukocytosis without eosinophilia. Transthoracic echocardiography revealed an image suggesting vegetations on the biological valve, which was confirmed by transesophageal echocardiography (Figure 1). Blood cultures were taken and empirical antimicrobial therapy was begun, but the patient’s infection worsened and he developed hemodynamic instability. The mitral bioprosthesis was accordingly replaced by a metal valve. The vegetation adhering to the bioprosthesis was cultured and following macroscopic examination (Figure 2) amphotericin B was added. On the sixth postoperative day growth of T. beigelii was observed in the culture from the bioprosthesis and, in view of clinical deterioration, the antifungal was replaced by voriconazole. However, the patient developed multiorgan failure and died on the 13th day after surgical intervention.
In the literature, there are only 11 published cases of IE due to T. beigelii.1–11 In the nine reports of cases affecting prosthetic valves,1,3,5–11 the mean interval between cardiac surgery and the diagnosis of IE was four years, ranging between three months and eight years. The present case is unusual in that 11 years had passed after valve replacement, making this the longest period so far recorded.
There are no laboratory findings characteristic of trichosporonemia,1,3 which often delays diagnosis of this serious condition. Eosinophilia was observed in only four3,5,6,8 of the 11 reported cases and was not seen in the present case.
Blood cultures are frequently negative in systemic trichosporonosis,2 although they revealed the presence of Trichosporon spp. in seven of the reported cases,2,3,5,7,9–11 and in those with negative blood cultures, cultures from other sites confirmed the infection.1,4,6,8 This was also the case in our patient, in whom the organism was only isolated from a culture of the valve vegetation.
The current first-line treatment of IE due to Trichosporon spp. is valve replacement associated with antifungal therapy.11 The antifungal used in most of the reported cases was amphotericin B,2–8,10,11 although some authors suggest others, including voriconazole. Analysis of the effectiveness of antifungal therapy is hindered by the severity of patients suffering from T. beigelii fungemia, in whom mortality can reach 80%.1 Only four of the 11 reported cases were considered cured during hospital stay,4,7,9,11 while eight patients died during four years of medical follow-up.2–7,9,10
ConclusionOf the few cases of IE of prosthetic valves due to T. beigelii, the current case presents the longest interval between valve replacement surgery and diagnosis of infection by this pathogen.
As in all the cases in the literature, low clinical suspicion led to a delay in beginning appropriate therapy. Considering the high mortality and severity of T. beigelii endocarditis, it should be considered when there is a prosthetic valve infection with negative blood cultures, irrespective of the time elapsed since the previous surgery.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Couto R, Couto G, Abrahão I, Compagnoni I, Carnio T, Tolentino J, Endocardite por Trichosporon beigelii 11 anos após cirurgia de troca valvar mitral. Rev Port Cardiol. 2021;40:305.