Heart failure (HF) is a growing public health problem. This study estimates the current and future costs of HF in mainland Portugal.
MethodsCosts were estimated based on prevalence and from a societal perspective. The annual costs of HF included direct costs (resource consumption) and indirect costs (productivity losses). Estimates were mostly based on data from the Diagnosis-Related Groups database, real-world data from primary care, and the opinions of an expert panel. Costs were estimated for 2014 and, taking population aging into account, changes were forecast up to 2036.
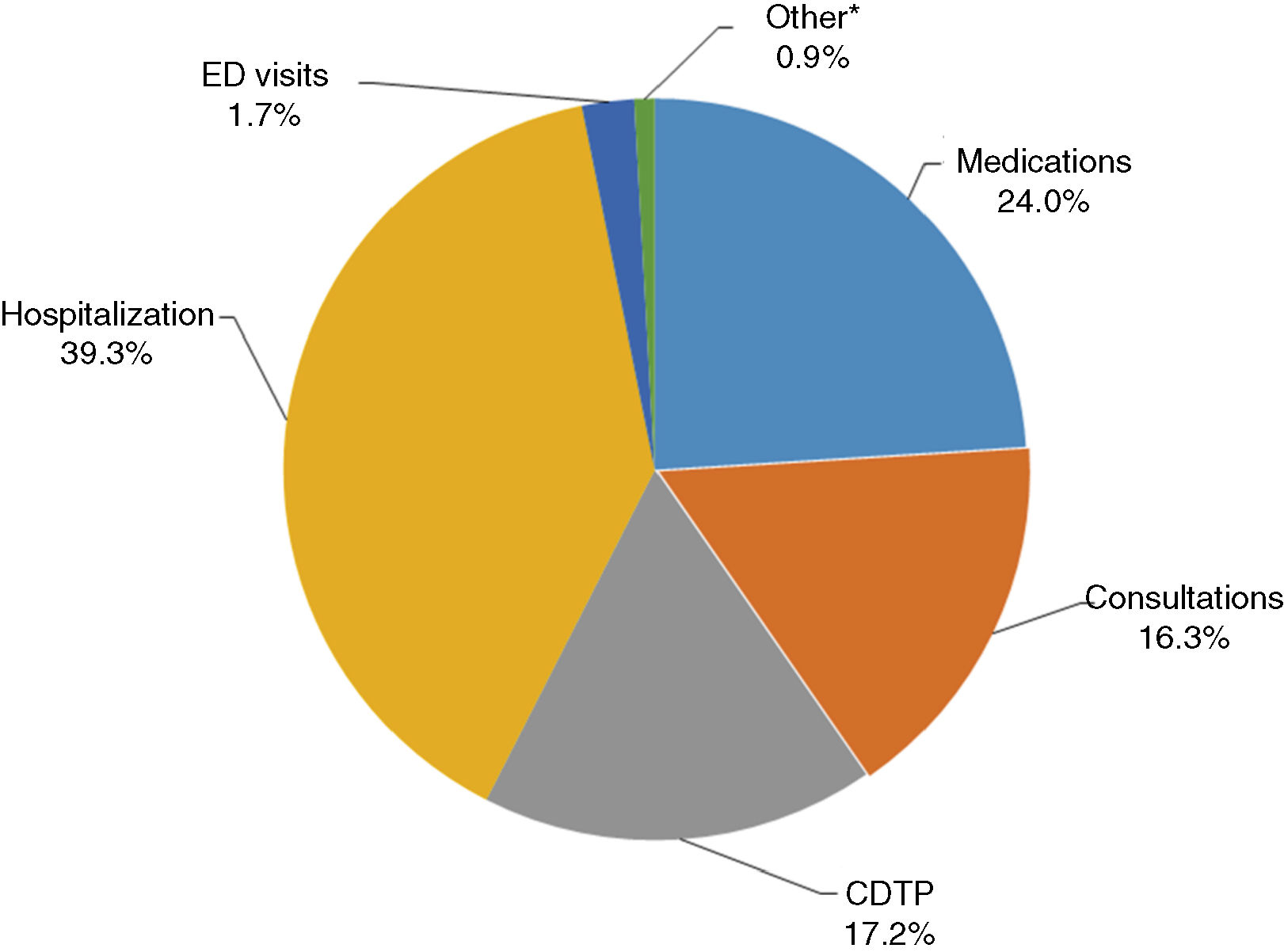
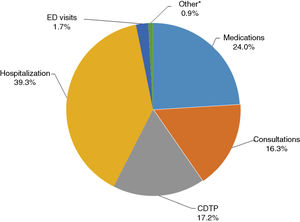
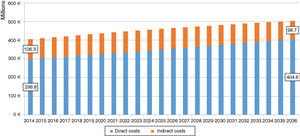
ResultsDirect costs in 2014 were є299 million (39% for hospitalizations, 24% for medicines, 17% for exams and tests, 16% for consultations, and the rest for other needs, including emergencies and long-term care). Indirect costs were є106 million (16% for absenteeism and 84% for reduced employment). Between 2014 and 2036, due to demographic dynamics, total costs will increase from є405 to є503 million. Per capita costs are estimated to rise by 34%, which is higher than the increase in total costs (+24%), due to the expected reduction in the resident population.
ConclusionsHF currently has a significant economic impact, representing around 2.6% of total public health expenditure, and this is expected to increase in the future. This should be taken into account by health policy makers, alerting them to the need for resource management in order to mitigate the impact of this disease.
A Insuficiência Cardíaca (IC) é um problema crescente de saúde pública. Este estudo estima os custos atuais e futuros da IC em Portugal Continental.
MétodosA estimativa dos custos foi realizada na ótica da prevalência e na perspetiva da sociedade. Os custos anuais da IC incluíram os custos diretos (consumos de recursos) e indiretos (impacto na produtividade da população). Utilizaram-se maioritariamente dados da Base de Dados de Morbilidade Hospitalar, dados da prática clínica real relativamente aos consumos nos cuidados primários e opiniões de peritos. Estimaram-se os custos para 2014 e, tendo em conta o envelhecimento da população, a evolução dos mesmos até 2036.
ResultadosOs custos diretos em 2014 totalizaram є299 milhões (39% por internamentos, 24% por medicamentos, 17% por meios complementares de diagnóstico e terapêutica, 16% por consultas, e o restante por outras rubricas como urgências e cuidados continuados). Os custos indiretos totalizaram є106 milhões (16% por absenteísmo e 84% por redução de emprego). Entre 2014 e 2036, por efeitos demográficos, os custos totais passarão de є405 para є503 milhões. O aumento nos custos por habitante será de 34%, um aumento superior ao dos custos totais (+24%) dada a redução prevista da população residente.
ConclusõesA IC tem um importante impacto económico atual (cerca de 2,6% do total das despesas públicas em Saúde) e previsivelmente maior no futuro, o qual deve ser tido em consideração pelos responsáveis pelas políticas de saúde por forma a adequar a gestão de recursos atual e futura e minimizar o impacto desta doença.
Heart failure (HF) is a clinical syndrome characterized by typical symptoms that may be accompanied by signs (such as elevated jugular venous pressure, pulmonary crackles and peripheral edema), caused by a structural and/or functional cardiac abnormality, resulting in reduced cardiac output and/or elevated intracardiac pressures at rest or during stress.1
The most common symptoms in HF (dyspnea and fatigue) have a significant negative impact on functional capacity and quality of life.2–4 Worsening symptoms and signs are reflected in episodes of decompensated HF, which frequently result in hospitalization.5
HF is a growing public health problem worldwide, with higher rates of prevalence among the elderly.6 It is estimated that over 37 million people throughout the world have HF,6 and its prevalence has increased in recent decades.7–9 This may reflect an increase in standardized incidence, aging of populations, increased survival of patients due to improved treatment of cardiovascular disease in general and of HF in particular (including risk factors such as hypertension and diabetes, and complications), or a combination of these factors.10
Despite the importance of HF for the individual patient and for society, the costs associated with the disease in Portugal are unknown. The aim of the present study was to estimate HF costs in mainland Portugal based on data for 2014 and to forecast changes in these costs up to 2036, in order to quantify the current and future economic impact of HF in Portugal.
MethodsCosts over the course of one year were estimated based on HF prevalence and from a societal perspective, including direct costs (resource consumption) and indirect costs (productivity losses) associated with the disease.
The study was divided into two stages. The first estimated costs for the base year (2014), and the second forecast changes up to 2036 taking into account the impact of predicted demographic changes (aging of populations).
The population analyzed was that resident in mainland Portugal aged 25 years or over.
Estimates of current costsPrevalenceHF prevalence in mainland Portugal in 2014, stratified by gender, age group and New York Heart Association (NYHA) functional class, was estimated based on microdata from the Portuguese EPICA study.11 EPICA was a community-based epidemiological survey conducted in 1998-2000 that involved 5434 primary health care users aged 25 years or over. There have been no more recent field studies, so we updated the EPICA data by recalculating prevalence rates taking into account changes in the demographic composition of the population. Since there is no information on HF epidemiology in the Portuguese population aged under 25 years, the prevalence assumed for this age group was zero. It was also assumed that patients in NYHA class I would not generate costs since their physical activity is not significantly limited; everyday physical activities do not cause symptoms in these patients1 and thus they tend to consume few health care resources that are attributable to HF.
Direct costsThe direct costs included in the analysis were those related to: (1) hospitalization; (2) outpatient consultations generating diagnosis-related group (DRG) episodes; (3) other hospital outpatient services; (4) emergency department (ED) services; (5) day hospital care; (6) primary health care (PHC); (7) medications; (8) urgent and non-urgent transport; and (9) use of the National Network of Long-term Care (RNCCI).
Estimates of resource consumptionWe used microdata from the national DRG database for 2014 to estimate resource consumption for HF in hospitalizations and hospital outpatient consultations.12
Hospitalizations for HF were identified based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. Patients who presented the following were included in the study:
- a)
HF as primary diagnosis13–15;
- b)
diagnosis of HF with a primary diagnosis of circulatory system disease;
- c)
heart transplantation or placement of cardiac resynchronization therapy (CRT) or ventricular assist devices, irrespective of associated diagnoses.
It should be noted that using the above criteria to identify hospitalizations for HF, all implantations of implantable cardioverter-defibrillators (ICDs) and other surgical procedures performed during episodes identified by criterion (a) or (b) were also counted as contributing to costs of hospitalization for HF.
The ICD-9-CM codes used are shown in Supplementary Table 1.
In cases of hospitalizations for heart transplantation, the additional costs of financial incentives to centers performing transplantations under Legislative Order no. 7215/2015 were also included.
There is no single accessible database that can be used to estimate all other health resource consumption in non-DRG hospital outpatient services. To overcome this lack, consumption patterns of other resources used were estimated based on various information sources, including a geographically representative panel of seven experts.
Assessment of ED use not followed by hospitalization was based on the proportion of patients who come to the ED for HF and are subsequently hospitalized. According to data from the ED of Braga Hospital in 2013, this figure was 36% (unpublished data), which is in line with that estimated by the expert panel. The number of ED episodes without hospitalization was therefore estimated based on this percentage and the number of urgent admissions with a primary diagnosis of HF obtained from the DRG database.
Use of day hospitals was based on the proportion of patients with HF followed in outpatient consultations (cardiology or internal medicine) at Centro Hospitalar de Lisboa Ocidental (1.5%), which was adjusted down to 1% in view of the fact, pointed out by the expert panel, that some hospitals do not provide day hospital services for HF patients.
A cross-sectional study was carried out of the Regional Health Authority (RHA) information system (SIARS) of the Lisbon and Tagus Valley region (LVT)16 in order to estimate resource consumption by HF patients followed in PHC. All patients meeting the following criteria were included in the analysis: (1) aged 25 years or over; (2) at least one consultation in 2014; and (3) HF code recorded (K77 in the International Classification of Primary Care, second edition). Of the 1.8 million users registered with the LVT RHA, 25316 patients met the above criteria. Analysis of the SIARS enabled the cost of patients followed in PHC to be estimated, including medication invoiced to the LVT RHA irrespective of the place of prescription. The cost of medication for patients followed in PHC within the LVT RHA was considered to be representative of all patients with HF nationwide followed as outpatients including hospital outpatient consultations.
Direct non-medical costs of transport, mainly to the ED or to PHC or hospital outpatient consultations, were included in the present study.
To calculate resource consumption for long-term care, data from the LVT RHA in 2013 were analyzed, together with data from a 2014 report on monitoring of the RNCCI.17 Two types of costs were estimated: those for patients receiving care at home and those for patients admitted to RNCCI facilities (Supplementary Table 2).
For this study, it was decided to adopt a conservative approach to costs associated with cardiac rehabilitation programs. According to a survey of cardiac rehabilitation in Portugal,18 in 2013-2014 there were only 245 HF patients included in phase II (early outpatient) programs in public and private centers.i Furthermore, there are no published estimates of the cost of such interventions. This item was therefore not included.
Finally, it was assumed conservatively that patients followed in PHC are not followed in hospital outpatient consultations and vice-versa. The proportion of patients with HF in cardiology and internal medicine outpatient consultations in 2014, as well as the mean annual number of consultations per HF patient, was estimated by the expert panel. This information was correlated with data on the total number of cardiology and internal medicine consultations in 2014,19 in order to estimate the number of HF patients in NYHA classes II-IV being followed in hospital outpatient consultations. It was assumed that the other patients in NYHA class II-IV HF were followed in PHC.
Unit costsUnit costs for hospitalizations, ED visits without admission, consultations, and complementary diagnostic and therapeutic procedures were estimated based on the prices published in Implementing Order no. 234/2015. The cost of ED visits was estimated as the weighted mean of the cost of a general ED visit (є112.07) and a medical/surgical ED visit (є85.9). The weighting is based on the relative frequency of episodes by type of emergency (medical/surgical or general), according to the 2014 Annual Report from the Central Administration of the National Health System (ACSS) on use of health care services in National Health System establishments and associated entities.20
The unit cost of urgent and non-urgent transport was taken as the weighted mean of the unit cost of the various types of transport available. Supplementary Table 3 shows the unit costs used in the analysis.
Indirect costsThe indirect costs included in the analysis corresponded to productivity losses through lower employment rates caused by early retirement due to long-term disability or higher unemployment compared to the general population, as well as those arising from absenteeism due to the disease (consultations, exams, ED visits, hospitalizations and convalescence). It was conservatively assumed that only patients aged under 65 years would generate such indirect costs.
We also assumed that the impact of disease on the ability to work was different depending on NYHA functional class. As stated above, overall prevalence was estimated by age group and by NYHA class based on microdata from the EPICA study.11 No patients aged under 65 years were found in NYHA class IV, and so it was assumed that this class does not generate indirect costs. In the case of HF patients in NYHA class III, it was assumed that their participation in the labor market would be similar to that of patients with previous myocardial infarction (MI). Unemployment rates, by age group and gender, of individuals aged between 25 and 64 years, with and without previous MI, were estimated from microdata from the 2014 National Health Survey.21 The gender difference in these rates (-48.4% in women and -34.3% in men) was taken as a proxy of reduced employment rates due to HF. Employment rates of patients in NYHA class II were assumed to be similar to that of the general population (64.5% for women and 73.5% for men, according to the 2014 National Health Survey). Such patients only generate indirect costs through absenteeism.
It was also assumed that for each consultation (irrespective of specialty), diagnostic exam or ED visit (without admission), a patient would lose half a day, a quarter or a whole working day, respectively. With regard to working time lost due to hospitalization and convalescence, the duration of convalescence was considered to be equal to the length of hospital stay.
Mean productivity losses were estimated based on the charges to employers of their workers according to the theory of human capital.22 The mean monthly salary was estimated at є1246.20 for men and є977.60 for women based on official sources,23 paid 14 times a year, to which was added employers’ social security contributions at a rate of 23.75%. The information used to calculate indirect costs is summarized in Supplementary Table 4.
Estimates of future costsA mean cost was estimated for each type of direct and indirect cost included in the analysis, by gender and age group. In the case of cost estimates for the average patient based on the opinion of the expert panel, the distribution of resource consumption by gender and age group was assumed to be similar to the distribution of resource consumption due to hospitalizations. The proportion of total costs that could be attributed to long-term care in 2014 was estimated and it was assumed that this proportion would be constant over time. In order to estimate expected increases in costs, it was assumed that all variables and parameters affecting them would be constant except for the demographic composition of the population. The mean costs per patient and HF prevalence rates by gender and age group were thus not considered to vary over the period under analysis.
The demographic projections for the population used in the analysis, by gender and age group, are those published by Statistics Portugal (INE).24
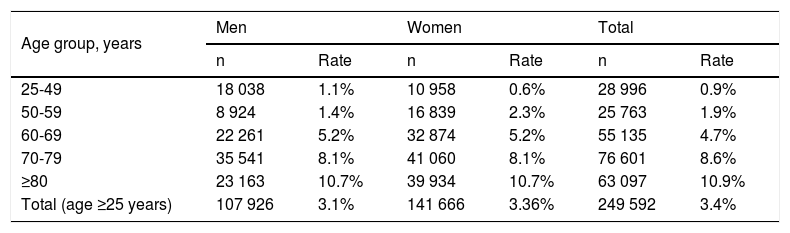
ResultsCurrent estimatesPrevalenceThe estimated overall prevalence of HF in the population aged 25 years or over in mainland Portugal in 2014 was 5.2% (95% confidence interval [CI]: 4.5-5.8), corresponding to 383043 patients (Supplementary Table 5). The prevalence of HF that generates costs (NYHA classes II-IV) was estimated at 3.4% (95% CI: 2.9-4.0), corresponding to 249592 patients (Table 1).
Prevalence of heart failure (New York Heart Association functional class II-IV), by gender and age group, in mainland Portugal in 2014.
| Age group, years | Men | Women | Total | |||
|---|---|---|---|---|---|---|
| n | Rate | n | Rate | n | Rate | |
| 25-49 | 18 038 | 1.1% | 10 958 | 0.6% | 28 996 | 0.9% |
| 50-59 | 8 924 | 1.4% | 16 839 | 2.3% | 25 763 | 1.9% |
| 60-69 | 22 261 | 5.2% | 32 874 | 5.2% | 55 135 | 4.7% |
| 70-79 | 35 541 | 8.1% | 41 060 | 8.1% | 76 601 | 8.6% |
| ≥80 | 23 163 | 10.7% | 39 934 | 10.7% | 63 097 | 10.9% |
| Total (age ≥25 years) | 107 926 | 3.1% | 141 666 | 3.36% | 249 592 | 3.4% |
The distribution of prevalence by age group and NYHA class is shown in Supplementary Table 6.
Direct costsThe DRG database identified 35924 admissions for HF, of which 39 were for heart transplantation. On average, patients admitted had 1.44 hospitalizations for HF per year.
In mainland Portugal in 2014, the total cost of hospitalizations for HF (including funding to public and private hospitals authorized to harvest and transplant organs) was estimated at є117489267.
The same source identified 628 hospital outpatient episodes in 2014, at a total cost of є853354.
The mean annual cost of hospital outpatient services associated with complementary diagnostic and therapeutic procedures, consultations and day hospital care was estimated at є534.30 per patient based on the consumption patterns determined by the expert panel and on unit costs.
The number of ED visits without admission for HF in 2014 was estimated at 53075, generating a direct medical cost of є5117997. The number of day hospital episodes was estimated at 3701, generating a total cost of є114734.
The mean annual costs of complementary diagnostic and therapeutic procedures and consultations for patients followed in PHC were estimated on the basis of SIARS data at є249.94 per patient. Using the same database, the annual mean cost of medication per HF patient was estimated at є287.49 (whether followed as hospital outpatients or in PHC). The cost of medications does not include value-added tax, since the study adopts a societal perspective.
The total costs of HF associated with transport (urgent and non-urgent) and with long-term care (home or residential) were estimated at є7362882 and є1786786, respectively.
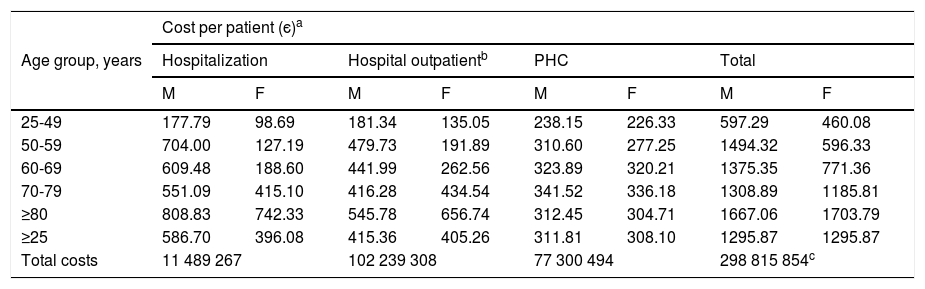
The mean costs per patient shown in Table 2 were estimated assuming that 55% of patients are followed in hospital outpatient consultations and 45% in PHC. The direct costs of HF in mainland Portugal in 2014 were around є299 million.
Direct costs per patient with heart failure (New York Heart Association classes II-IV) in mainland Portugal in 2014.
| Age group, years | Cost per patient (є)a | |||||||
|---|---|---|---|---|---|---|---|---|
| Hospitalization | Hospital outpatientb | PHC | Total | |||||
| M | F | M | F | M | F | M | F | |
| 25-49 | 177.79 | 98.69 | 181.34 | 135.05 | 238.15 | 226.33 | 597.29 | 460.08 |
| 50-59 | 704.00 | 127.19 | 479.73 | 191.89 | 310.60 | 277.25 | 1494.32 | 596.33 |
| 60-69 | 609.48 | 188.60 | 441.99 | 262.56 | 323.89 | 320.21 | 1375.35 | 771.36 |
| 70-79 | 551.09 | 415.10 | 416.28 | 434.54 | 341.52 | 336.18 | 1308.89 | 1185.81 |
| ≥80 | 808.83 | 742.33 | 545.78 | 656.74 | 312.45 | 304.71 | 1667.06 | 1703.79 |
| ≥25 | 586.70 | 396.08 | 415.36 | 405.26 | 311.81 | 308.10 | 1295.87 | 1295.87 |
| Total costs | 11 489 267 | 102 239 308 | 77 300 494 | 298 815 854c | ||||
F: female; M: male; PHC: primary health care.
Figure 1 summarizes total direct costs by item. It can be seen that the largest proportion of costs was for hospitalization (39.3%), followed by medication (24.0%).
Distribution of total direct costs due to New York Heart Association class II-IV heart failure in mainland Portugal in 2014. * Includes National Network of Long-term Care and outpatient episodes. CDTP: complementary diagnostic and therapeutic procedures; ED visits: emergency department visits without admission.
Indirect costs for HF in mainland Portugal in 2014 totaled around є106 million, 83.9% of which was due to reduced employment and the remainder to absenteeism arising from consultations, complementary diagnostic and therapeutic procedures, ED visits without admission, hospitalization and convalescence. Supplementary Tables 7 and 8 show the breakdown of the indirect costs analyzed.
Total costsEstimated total annual costs (direct and indirect) of HF in mainland Portugal in 2014 amounted to around є405 million, most of which (74%) was direct costs. Around 39% of total direct costs (29% of total costs) were attributable to hospitalizations. The mean annual total cost per patient in NYHA classes II-IV was around є1623.
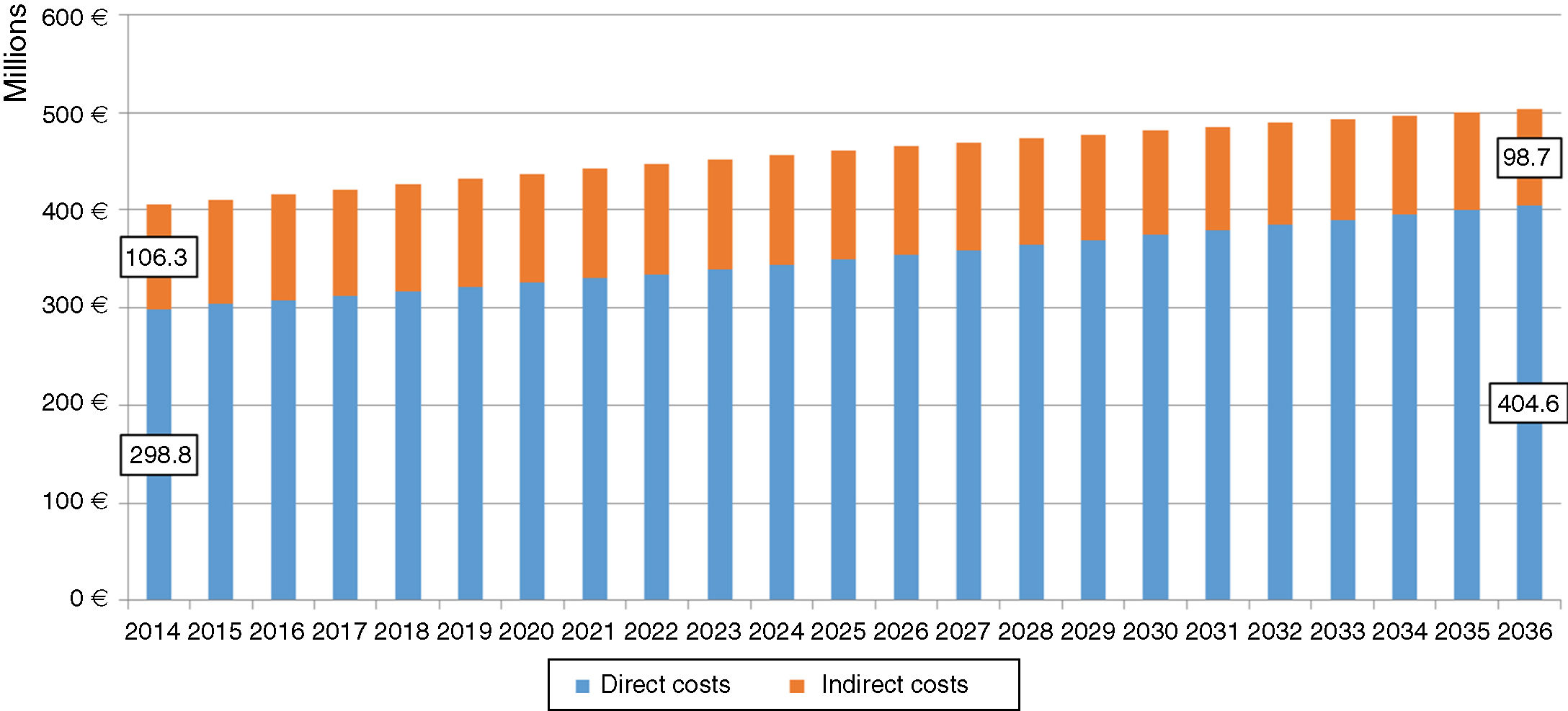
Future estimatesWe estimate that there will be 318071 patients with NYHA class II-IV HF in mainland Portugal in 2036, 27% more than in 2014 (249592 patients). The total costs (direct and indirect costs) for these patients in 2036 are estimated at around є503 million (Figure 2).
Our analysis shows that direct costs will increase constantly over the period studied, while indirect costs may increase up to 2023 (5.4% compared to 2014) and then decrease until 2036 (-7.2% compared to 2014) (Figure 2).
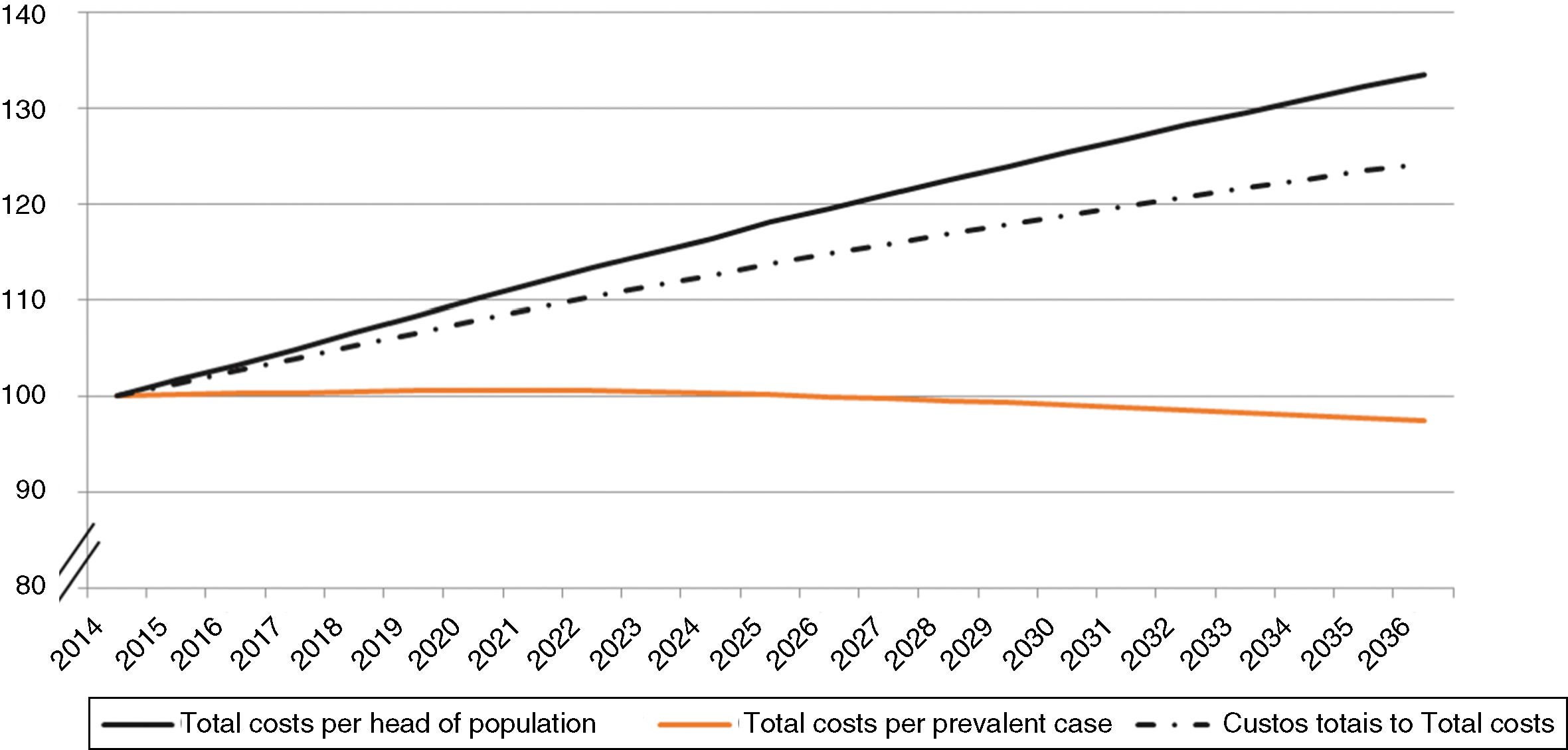
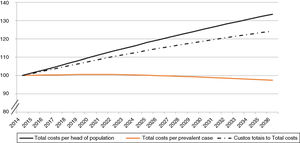
The annual costs per patient with NYHA class II-IV HF rise slightly until 2021 (from є1623 in 2014 to є1633 in 2021), and then decrease somewhat (to є1582 in 2036). On the other hand, the cost per head of population is estimated to rise by around 34% between 2014 and 2036 (Figure 3), as there will be a more rapid increase in cost per head of population, from є41 to є55.
DiscussionHF is a clinical syndrome caused by a structural and/or functional cardiac abnormality1 and it is the final presentation of a wide range of disorders. Improved treatment of these disorders, such as MI, may in itself have contributed to the increased prevalence of HF observed in recent decades.10 In addition, the number of patients with HF is expected to continue to rise as a result of aging populations and its higher prevalence at older ages.6 These trends may well have important implications for the costs of HF over the coming decades.
This study presents an initial estimate of current costs of HF in mainland Portugal (based on 2014 data) and predicted changes up to 2036. The estimates presented for the future do not take into account any cause for variation other than demographic changes, as prevalence patterns by gender and age group were assumed to be constant over the period analyzed. In particular, the estimates do not consider the effects that scientific and technological innovations may have on the costs associated with the disease, since these are impossible to predict. For instance, if a new technology were developed that cures HF, it would be associated with increased short-term costs but would reduce costs in the long term.
The total costs attributable to NYHA class II-IV HF in mainland Portugal in 2014 were about є405 million, which corresponds to around 0.2% of gross domestic product and 2.6% of health expenditure.25,26 Projected total annual costs for NYHA class II-IV HF suggest an increase of around 24% between 2014 (є405 million) and 2036 (є503 million). Since the projections assume a decrease in the resident population, the above estimate implies a 34% increase in annual costs per head of population between 2014 and 2036.
According to our projections, indirect costs will rise until 2023 and then fall in the later years of the period under analysis. This is due to the lower proportion of active individuals (aged 65 years or under) in the population who contribute to the indirect costs included in the analysis. However, the higher number of older patients, resulting in constant growth in direct costs over the study period, underlies the increase in the overall costs of HF. The reduction in indirect costs also explains why the rate of growth in overall costs is lower than the rate of growth in the number of patients with HF (24% vs. 27%).
This study has the advantage of using real-world data to estimate resource consumption patterns in hospitalizations and PHC, but various assumptions had to be made to estimate other types of resource consumption, particularly in hospital outpatient care, long-term care and transport. Even though these assumptions constitute limitations in our study, we opted to take a conservative approach in the following ways: (1) the costs of cardiac rehabilitation programs were not included; (2) it was assumed that patients were followed in either PHC or in hospital, when in fact some patients will be followed in both; (3) costs associated with patients in NYHA class I were not included in the analysis, even though some patients with no functional limitations may be under pharmacological therapy that incurs direct costs; and (4) indirect costs associated with carers of HF patients were not included, even though older patients in particular may require support for attending consultations and undergoing diagnostic exams and treatment, as well as home care. This means that overall costs are probably underestimated. Furthermore, the present study used the DRG database to estimate resource consumption due to HF in terms of hospitalizations and hospital outpatient services, but there are known limitations in the recording of clinical information in hospital administration databases in general and in the DRG database in particular, including the coding of HF.27,28
Overall, the results of this study are in line with those reported in the international literature, in which HF is described as a public health issue of increasing importance.6 A recently published systematic review of studies estimating the costs associated with HF29 included 16 studies published between 2004 and 2016, four of which are of particular interest when discussing our results, since they are more recent (after 2010), they estimate costs from the standpoint of prevalence (as in our study), and they estimate HF costs in other European countries (Poland,30 Spain,31 Greece32 and Ireland33). None of these four studies30–34 included costs due to productivity losses. In order to compare cost estimates per patient among different countries, the authors of the systematic review converted the reported values to US dollars using exchange rates adjusted for purchasing power parity.34
Applying the same methodology to the results of the present study, we estimate the annual mean direct cost in mainland Portugal per patient with HF to be US $2043. This is lower than that reported by the four more recent European studies30–34 with a prevalence-based analysis, which ranged between US $4755 in Poland30 and US $16330 in Ireland.32 In these four studies, direct costs were mainly related to hospitalizations, which accounted for 58-92% of total direct costs. The corresponding estimate in the present study was 39%, which may indicate that the populations assessed in the other studies were substantially different from ours, and mainly included hospitalized patients. In our study, we also had data on PHC, and so we were able to provide a broader picture, which probably resulted in less severe disease on average and lower mean costs per patient.
In addition, compared to the rest of Europe, southern European countries have a lower rate of cardiac device implantation (such as CRT devices, ICDs, prosthetic aortic valves and left ventricular assist devices), which could also contribute to lower HF costs in Portugal, particularly for hospitalizations.35
Overall, the results reported here give further backing to the warning in a recently published consensus document36 that pointed to the pressing need to prioritize HF in the national health agenda, given the current and expected future prevalence of HF and the associated socioeconomic burden for patients, their families and society in general.
ConclusionHF in mainland Portugal has a considerable economic impact, accounting for around 2.6% of total public health expenditure, and this burden is expected to grow significantly over the next twenty years. Most costs correspond to direct costs, particularly those related to hospitalization. The structure of these costs and their predicted growth should be taken into account by all those involved in health administration, including the development and implementation of health policies, in order to optimize current and future management of resources and to minimize the impact of this disease.
Conflicts of interestC.F. received consulting and speaker fees from AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Orion, Servier Portugal, Sanofi, and Vifor. RA, JC and MB are members of the Evidence Based Medicine (EBM) Center at Lisbon School of Medicine, Portugal. This research center is devoted to pre‐ and postgraduate medical education. Since 2002 the Lisbon EBM Center has undertaken several clinical, epidemiological and phamacoeconomic research projects, which had unrestricted funding from over 20 different pharmaceutical companies. One of these was Novartis Farma, Produtos Farmacêuticos SA. FF was a member of the Lisbon EBM Center at the time of paper submission. MG and PB declare no conflicts of interests.
We would like to thank Aurora Andrade, Irene Marques, Susana Costa, Dulce Brito, Daniel Caldeira and Cláudio David for their expert advice, without whom this study could not have been performed. We also thank José Mariz for providing information on ED visits and HF at Braga Hospital.
We are also grateful to the Central Administration of the National Health System for granting access to the DRG database, as well as to the LVT RHA for access to their PHC database. Lastly, we express our gratitude to the EPICA study investigators for providing access to their microdata.
This work received financial support from Novartis Farma, Produtos Farmacêuticos SA, in the form of an unrestricted grant to the Research and Development Association of the Medical School of Lisbon University. Novartis Farma played no role in any stage of the project.
Please cite this article as: Gouveia MRdA, Ascenção RMSS, Fiorentino F, Costa JNMPGd, Broeiro-Gonçalves PM, Fonseca MCFGd, et al. Os custos da insuficiência cardíaca em Portugal e a sua evolução previsível com o envelhecimento da população. Rev Port Cardiol. 2020;39:3–11.
The publication in question does not show the distribution by disease of the 967 individuals in phase III (long-term outpatient) cardiac rehabilitation programs. However, if the same percentage is assumed for these programs as for phase II programs (12.7%), the number of HF patients in phase III programs would be 123 individuals. Phase I programs are in-hospital and so it was assumed that their cost would be included in the costs of hospitalization determined through analysis of the DRG database.