We report a case of severe fulminant myocarditis that closely mimicked acute inferior ST-segment elevation myocardial infarction (STEMI) and presented with refractory cardiogenic shock, multiple life-threatening arrhythmias and rapidly progressive liver failure. This case was successfully differentiated from STEMI by emergency coronary angiography. Recurrent cardiogenic shock was reversed by intra-aortic balloon pumping (IABP). Life-threatening arrhythmias including ventricular tachycardia, ventricular fibrillation, and high-degree atrioventricular block (AVB) were terminated by immediate cardioversion and temporary pacemaker. High-dose hydrocortisone effectively attenuated the inflammatory injury to the myocardium. The patient recovered and was well at the follow-up visit four months after discharge.
Relatamos um caso real de miocardite fulminante grave simulando enfarte agudo do miocárdio agudo inferior com supra desnivelamento ST (STEMI) com choque cardiogénico refratário, arritmias fatais múltiplas e lesão hepática funcional progressiva. Detetou-se com eficácia que não se tratava de STEMI através de angiografia coronária de urgência. O choque cardiogénico recorrente foi resolvido com eficiência através de balão intra-aórtico. Arritmias fatais incluindo a taquicardia ventricular, a fibrilhação ventricular e o bloqueio auriculoventricular de alto grau foram ultrapassadas por cardioversão imediata e pacemaker temporário. Uma dose elevada de hidrocortisona atenuou eficazmente lesões inflamatórias no miocárdio. O doente ultrapassou esta situação e estava totalmente recuperado na consulta de follow-up quatro meses após a alta.
Acute myocarditis is an inflammatory myocardial disease usually caused by viral infection and subsequent inflammatory response in cardiac myocytes. Fulminant myocarditis is the most severe subtype of myocarditis, characterized by a rapidly progressive course, severe clinical symptoms and a high mortality rate.1,2 Diagnosis and treatment of fulminant myocarditis remain challenging in clinical practice,3 especially when its manifestation closely mimics acute ST-segment elevation myocardial infarction (STEMI).4,5 Medical treatment is still the main therapy for fulminant myocarditis. Intra-aortic balloon pump (IABP) and ventricular assist devices have been increasingly used as mechanical circulatory support in cases of cardiogenic shock, but their effectiveness in fulminant myocarditis requires further confirmation.6–8 Moreover, since life-threatening arrhythmias such as ventricular tachycardia and atrioventricular block can cause cardiac arrest in fulminant myocarditis, optimization of anti-arrhythmia therapy is critically important in preventing sudden death.9
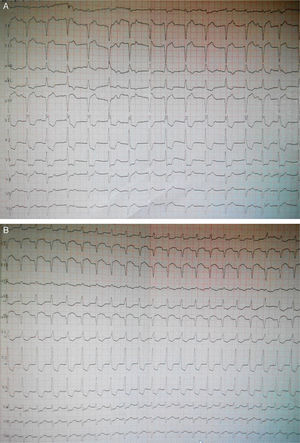
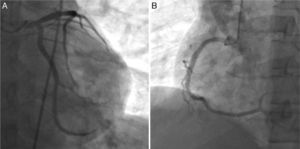
Case reportA man in his 40s was admitted to our department for recurrent chest pain, cough and expectoration during the previous three days. The patient had no relevant previous history. The admission electrocardiogram (ECG) showed 1–2 mm ST-segment elevation and QS waves in leads II, III and aVF (Figure 1A); the myocardial injury marker troponin I was elevated to 13.02 ng/ml. The patient was initially diagnosed with suspected acute inferior STEMI. However, seven hours after admission, he complained of severe chest pain, dyspnea and sweating. Immediate blood pressure determination was 54/33 mmHg and immediate 12-lead ECG showed 4–5 mm ST-segment elevation in leads II, III and aVF, exhibiting dynamic changes from the admission ECG (Figure 1B). A diagnosis of acute inferior STEMI was established. Blood pressure was maintained at normal levels by dopamine. An urgent coronary angiography was also performed. However, all the major coronary arteries were demonstrated to be normal except for a myocardial bridge in the left anterior descending artery (Figure 2). The diagnosis was subsequently corrected to fulminant myocarditis. Two hours after angiography, the patient experienced cardiogenic shock again, and his blood pressure fell to 67/35 mmHg, resistant to cardiotonic or vasopressor drugs, including dopamine, dobutamine and aramine. The shock was not effectively reversed until emergent IABP implantation. Four hours after IABP implantation, the patient suffered Adams-Stokes syndrome three times; the ECG monitor showed that one attack was due to ventricular tachycardia (Figure 3A), while the other two were due to ventricular fibrillation (Figure 3B). Synchronized cardioversion was performed three times with an energy setting of 200 J. The patient was successfully resuscitated and continuous amiodarone was administered. However, about 10 hours later, he again suffered a syncopal episode, with blood pressure of 72/37 mmHg. The ECG monitor recorded high-degree atrioventricular block (AVB), with a longest R-R interval of 7.0 s (Figure 3C). A temporary pacemaker was emergently implanted and the bradycardia was effectively resolved (Figure 3D). A dose of 450 mg hydrocortisone was subsequently administered and maintained continuously for one week.
12-lead ECGs on admission and showing dynamic changes during hospitalization. (A) ECG on admission showing complete right bundle branch block, QS waves and 1–2 mm ST-segment elevation in leads II, III and aVF; (B) ECG seven hours after admission showing sinus tachycardia, complete right bundle branch block, QS waves and 4–5 mm elevation of ST-segment in leads II, III and aVF, and 0.5–3 mm ST-segment depression in leads I and V1–V5.
Two days after admission, viral serology showed a significantly increased cytomegalovirus IgG level (60.3 U/ml). During hospitalization, relevant serum parameters including troponin I, pro-BNP, and liver injury markers including alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were also measured repeatedly. Troponin I and pro-BNP increased significantly and then reduced slowly. ALT and AST also rose to extremely high levels (3475 U/l and 5670 U/l, respectively) and declined with improvement of heart failure.
The patient recovered, and after being hospitalized for 23 days was discharged with a left ventricular ejection fraction (LVEF) of 72%. He underwent a follow-up visit four months after discharge, which demonstrated fully recovered heart function and normal cardiac structure on cardiac ultrasound. Coronary arteries and heart rhythm were also normal on coronary computed tomography (CT) angiography and Holter ECG monitoring, respectively.
DiscussionWe report a case of severe fulminant myocarditis and share our experience in diagnosing and treating this patient. Several points deserve consideration. Firstly, this case was initially misdiagnosed as acute inferior STEMI. In clinical practice, it is unusual for myocarditis to manifest with a STEMI-like ECG.10 However, in this case, the ECG demonstrated features seen in myocardial infarction as well as dynamic changes typical of STEMI. Under such circumstances, coronary angiography is still the most reliable approach for differential diagnosis. We performed emergency angiography and effectively differentiated the patient's condition from STEMI. The results of IgG serology and coronary CT angiography further supported the diagnosis of myocarditis.
Another feature of the case was rapidly progressive heart failure, refractory cardiogenic shock and resistance to pharmaceutical therapy. Fortunately, emergent IABP implantation effectively reversed the heart failure and shock. This is further evidence for using IABP under these circumstances. Besides pro-BNP, the significantly increased ALT and AST levels might also have resulted from severe heart failure and cardiogenic shock.
Malignant arrhythmias are usually the leading causes of death in the setting of fulminant myocarditis.9 In this case, three life-threatening arrhythmias occurred simultaneously and were terminated by immediate cardioversion or pacemaker implantation. We therefore suggest timely and aggressive interventions to prevent sudden death in fulminant myocarditis.
The efficacy and safety of immunosuppressive agents in acute myocarditis remain controversial,11–13 but they are empirically recommended in fulminant myocarditis.14 In this case, hydrocortisone at a dose of 450 mg as steroid pulse therapy convincingly demonstrated efficacy and excellent safety. An LVEF of 72% indicated fully recovered heart function. This is further confirmation of the efficacy of immunosuppressive therapy in fulminant myocarditis.
One shortcoming of our case was a lack of evidence from endomyocardial biopsy or cardiac magnetic resonance imaging, due to the patient's extremely emergent condition and the limited availability of these two techniques in China.
Overall, we conclude that coronary angiography is still the most effective approach to differentiating fulminant myocarditis from acute myocardial infarction. Timely and aggressive interventional measures may significantly reduce the risk of sudden death from cardiogenic shock or life-threatening arrhythmias in fulminant myocarditis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThis work was supported by the National Natural Science Foundation of China (No. 81200603). The authors have no conflict of interest to declare.