Severe periprosthetic regurgitation is a rare but potentially serious complication of valve surgery. It can present clinically as heart failure, hemolytic anemia or infective endocarditis. The diagnosis is normally suspected following transthoracic echocardiography.
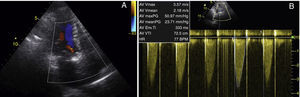
A 78-year-old woman with paroxysmal atrial fibrillation had undergone aortic valve replacement with a mechanical prosthesis 10 years previously and was under oral anticoagulation. She had recently been hospitalized for chest pain with anterior ST elevation. Coronary angiography revealed no epicardial coronary disease but showed what appeared to be a thrombus in the distal anterior descending artery; aortography showed moderate aortic regurgitation. Echocardiography revealed elevated transvalvular gradients, suggestive of mismatch and/or increased flow, and mild regurgitation (Figure 1). The setting was interpreted as embolic infarction. The patient was discharged with indication for close monitoring of INR, and transesophageal echocardiography was scheduled to assess valve function.
Transthoracic echocardiography showing: (A) mechanical aortic valve (21-mm Medtronic® with mild regurgitation, possibly periprosthetic; (B) elevated transvalvular gradients (maximum 51 mmHg and mean 24 mmHg); acceleration time 89 ms, left ventricular outflow tract velocity time integral/aortic velocity time integral 0.29 and area index 0.83 cm2/m2, suggestive of mismatch and/or increased flow.
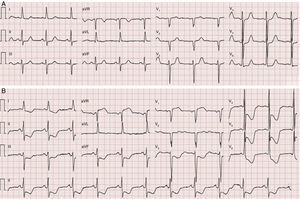
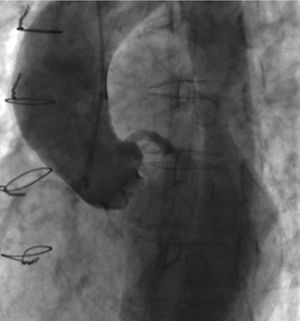
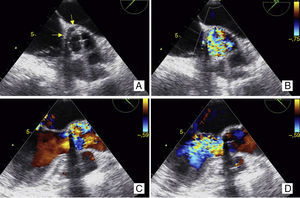
She was re-admitted two weeks later for recurrence of intense chest pain, together with autonomic symptoms and marked ST depression (Figure 2), which did not respond to medical therapy. Repeat cardiac catheterization excluded coronary artery disease and showed good disc opening of the prosthetic valve and severe aortic regurgitation (Figure 3). Thoracic computed tomography angiography excluded acute aortic syndrome. Transesophageal echocardiography showed severe periprosthetic regurgitation (Figure 4). The patient was referred for cardiac surgery.
Transesophageal echocardiography: (A and B) short-axis view (40°), showing valve dehiscence in the region of the non-coronary cusp, affecting 25–30% of the perimeter of the prosthesis (yellow arrows); (C) (in systole) and (D) (in diastole), long-axis view (120°), showing turbulent regurgitant jet, wide at its source, filling the entire left ventricular outflow tract.
Diagnosing periprosthetic regurgitation can be a challenge when the clinical presentation is atypical and transthoracic echocardiography fails to clarify the situation. The resulting decrease in diastolic coronary perfusion pressure can lead to severe subendocardial ischemia. In the case presented, due consideration of the symptoms and use of various imaging techniques confirmed the diagnosis and enabled appropriate treatment to be planned.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Almeida I, Madeira M, Caetano F, et al. Uma causa rara de isquemia subendocárdica. Rev Port Cardiol. 2015;34:429–431.