Kounis syndrome is an acute coronary syndrome in the context of a hypersensitivity reaction. The main pathophysiological mechanism appears to be coronary vasospasm.
We report the case of a patient with a history of allergy to quinolones, who was given ciprofloxacin before an elective surgical procedure and during drug administration developed symptoms and electrocardiographic changes suggestive of ST-segment elevation acute coronary syndrome. The drug was suspended and coronary angiography excluded epicardial coronary disease. Two hours after withdrawal of the drug the symptoms and ST elevation had resolved completely.
A síndrome de Kounis corresponde a uma síndrome coronária aguda em contexto de reação de hipersensibilidade. O mecanismo fisiopatológico principal parece estar relacionado com vasospasmo coronário. Apresentamos o caso de um doente com história de alergia a quinolonas, ao qual foi administrado ciprofloxacina antes de um procedimento cirúrgico eletivo e que, durante a administração do fármaco, desenvolve quadro sugestivo de síndrome coronária aguda com supradesnivelamento de ST. O fármaco foi suspenso e a realização de cateterismo cardíaco emergente revelou ausência doença coronária epicárdica. Duas horas após a interrupção do fármaco, o quadro clínico resolveu completamente.
In acute coronary syndrome (ACS), coronary angiography excludes significant coronary disease in 5-20% of cases.1 We report the case of a patient admitted to our department for ST-segment elevation ACS but with no epicardial coronary disease on coronary angiography. The ACS was probably due to a hypersensitivity reaction. Myocardial infarction or angina secondary to an allergic reaction is known as Kounis syndrome.2
Case reportAn 85-year-old man, white, a former smoker, had a history of hypertension, stage 4 chronic kidney disease, bladder cancer under follow-up, and allergy to quinolones. He was being medicated with hydroxyzine 25 mg daily and alprazolam 0.25 mg daily.
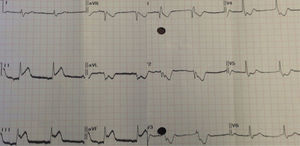
He was admitted electively to the hospital for surgical circumcision and meatoplasty. During administration of ciprofloxacin in the operating theater he developed constricting chest discomfort associated with dyspnea, sweating and hypotension. Electrocardiographic monitoring showed apparent ST elevation, so ciprofloxacin was suspended and the patient was transferred to the hospital's emergency department. The electrocardiogram (ECG) revealed ST elevation (>3 mm) in DII, DIII and aVF, with ST depression and T-wave inversion in aVL and V1-V3 (Figure 1).
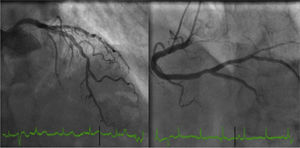
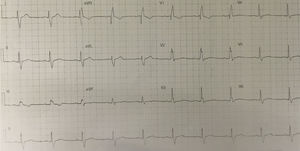
Given the suspicion of inferoposterior ST elevation ACS, he was medicated with a loading dose of ticagrelor (180 mg), aspirin 250 mg and morphine 8 mg and referred to our hospital for emergent catheterization. Coronary angiography, performed two hours after symptom onset, excluded coronary disease (Figure 2) and he was admitted to the cardiac intensive care unit. On admission he was asymptomatic and hemodynamically stable (blood pressure 112/67 mmHg) and the ECG showed sinus rhythm, right bundle branch block, and no ST-segment alterations (Figure 3). Transthoracic echocardiography revealed no wall motion abnormalities or other relevant changes. Laboratory tests showed leukocytosis (11.72×103/μl, reference value 3.8-10.6×103/μl), neutrophilia (86.8%) and elevated C-reactive protein (5.24 mg/dl, reference value 0-0.5 mg/dl). These inflammatory parameters normalized within 24 hours. Assessment of cardiac biomarkers showed slight changes in high-sensitivity troponin T (falling from 0.051 to 0.035 ng/ml at 12 hours, reference value 0.003-0.014 ng/ml) and normal pro-B-type natriuretic peptide (102 pg/ml, reference value 0-450 pg/ml).
Given the absence of coronary disease, together with the patient's history of allergy to quinolones and the temporal association with ciprofloxacin administration, a diagnosis of allergic ACS (Kounis syndrome) was made. The patient was discharged after 24 hours of surveillance, medicated with long-acting oral nitrates, and there were no further events in two-month follow-up.
DiscussionKounis syndrome, also known as allergic angina and allergic myocardial infarction, is an ACS in the context of a hypersensitivity reaction.3 First described by Kounis in 1991,2 it appears to be related to the release of inflammatory mediators by mast cells in the course of an allergic reaction.4 Among these mediators is histamine, which as well as inducing tissue factor expression and activating platelets, can trigger coronary vasospasm.5 The condition has been reported in the context of hypersensitivity to drugs, particularly antibiotics, non-steroidal anti-inflammatories and chemotherapy agents, and environmental exposure, such as to foods or insect bites.4
Three subtypes of Kounis syndrome have been described6: type I, due to coronary artery spasm in individuals without significant coronary disease; type II, in patients with pre-existing coronary disease, in whom the release of pro-inflammatory mediators causes vasospasm or atherosclerotic plaque instability; and type III, stent thrombosis due to a hypersensitivity reaction.7
In the case presented, the patient had a history of allergy to quinolones, and so previous sensitization may explain the speed with which the clinical setting developed. The absence of significant coronary disease led to this episode being classified as type I.
The clinical spectrum of Kounis syndrome is highly variable, and depends on the initial allergic response, the patient's comorbidities and susceptibilities (particularly history of atopia or autoimmune disease8), and level of exposure to the allergen. It can affect children,9 and its severity ranges from transient episodes such as reported here to cases of cardiogenic shock.10
There is no consensus on treatment for Kounis syndrome, and most of the data on it are from case reports. At all events, the therapeutic strategy depends on the subtype.11 In type I, treating the allergic reaction should resolve the ACS if this has not occurred spontaneously on withdrawal of the allergen, as in the case presented, in which the only action was immediate suspension of the drug, without any anti-allergic treatment. In types II and III, it is also necessary to treat the ACS.12 In addition to standard ACS treatment,13 the vasospasm should be treated with vasodilators (nitrates and non-dihydropyridine calcium channel blockers). Treatment of the allergic reaction includes anti-histamines and epinephrine,14 although the latter should be considered on a case-by-case basis depending on the severity of the anaphylactic reaction, given the simultaneous presence of an ACS.
ConclusionKounis syndrome is a diagnosis to be borne in mind in cases of suspected ACS in the context of an allergic reaction. The mechanisms of this condition are not fully understood, but treatment should be directed at the hypersensitivity reaction and the coronary event, in accordance with the results of coronary angiography.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Almeida J, Ferreira S, Malheiro J, Fonseca P, Caeiro D, Dias A, et al. Causa rara de síndrome coronária aguda: síndrome de Kounis. Rev Port Cardiol. 2016;35:699.