Stress cardiomyopathy and myocardial infarction are generally regarded as mutually exclusive diagnoses. We report the case of a 54-year-old woman who presented with acute chest pain. Her echocardiogram and ventriculography were typical of stress cardiomyopathy, but she had one subocclusive coronary lesion, a highly significant rise in troponin and a subendocardial myocardial infarction scar documented on cardiac magnetic resonance. This is a rare case of concomitant myocardial infarction and stress cardiomyopathy, in which the acute coronary syndrome itself may have been the stressor, given the absence of other identifiable causes.
A cardiomiopatia de stress e o enfarte agudo do miocárdio são geralmente considerados diagnósticos mutuamente exclusivos. Neste artigo reportamos o caso de uma doente de 54 anos com um quadro clínico de angor inaugural em repouso, cujo ecocardiograma e ventriculografia eram típicos de cardiomiopatia de stress. Não obstante, a coronariografia revelou uma lesão coronária suboclusiva, verificou-se elevação muito significativa de troponina e documentou-se uma cicatriz de enfarte subendocárdico por ressonância magnética cardíaca. Este é um caso raro em que um enfarte agudo do miocárdio e uma cardiomiopatia de stress ocorreram simultaneamente, em que o primeiro poderá ter sido o stressor que despoletou o segundo, dada a ausência de outras causas identificáveis.
Stress cardiomyopathy is generally an exclusion diagnosis after myocardial infarction (MI), myocarditis and pheochromocytoma have been ruled out. We report a rare case of concomitant stress cardiomyopathy and MI, which represented a challenge to current diagnostic criteria.
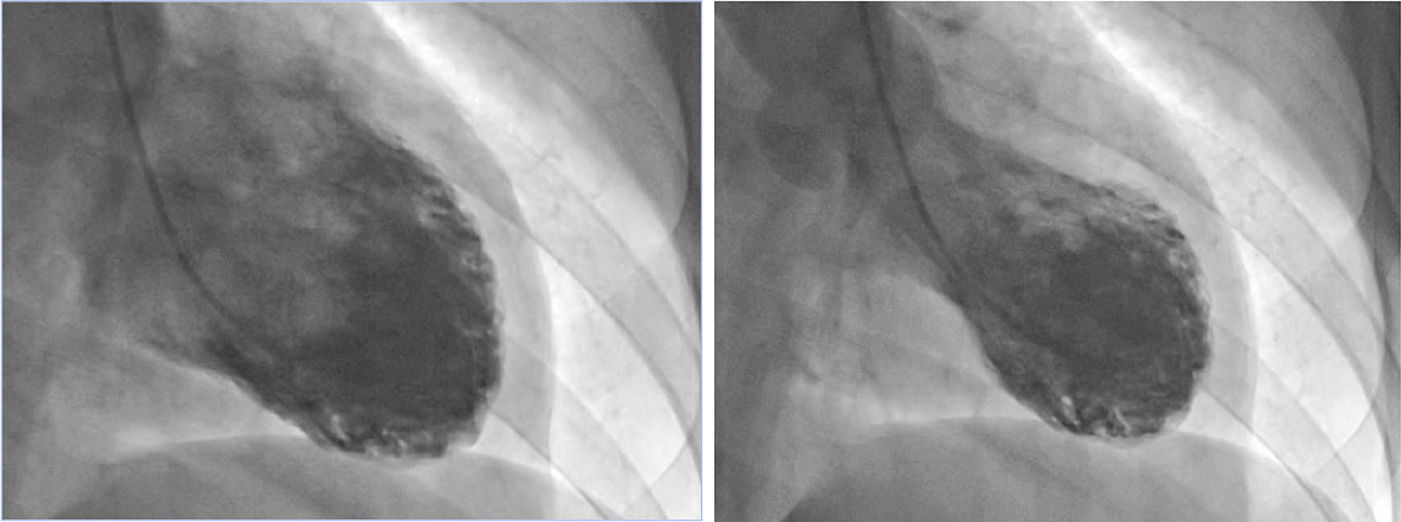
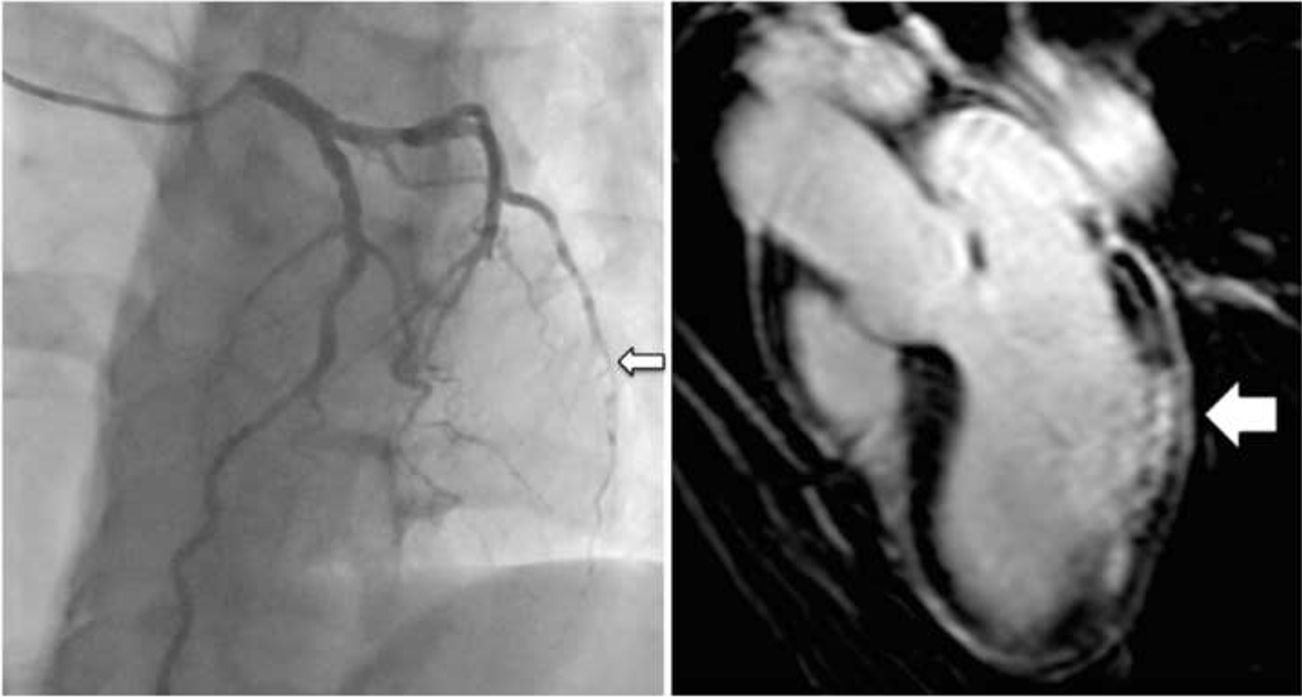
Case reportA 54-year-old woman with a history of dyslipidemia and smoking went to the emergency department (ED) due to crushing chest pain, radiating to the back, with sudden onset at rest 16 hours previously. She had no other symptoms and had not suffered any stressful events that day or in the recent past. On arrival in the ED she was febrile (38°C), but other vital signs and physical examination were normal. The electrocardiogram (ECG) presented an rS pattern in DIII and aVF only. The initial echocardiogram performed in the ED revealed left ventricular dilatation with mid-apical akinesis of all walls and hyperkinesis of all basal segments, producing an image of ventricular ballooning. The patient was immediately sent for emergency catheterization. Ventriculography showed the same findings as the initial echocardiogram (Figure 1); coronary angiography revealed a subocclusive mid-distal lesion of the obtuse marginal coronary artery (Figure 2) and irregularities in the right coronary artery.
The pain was found to have spontaneously resolved on admission to the cardiology ward, and hospital stay was uneventful. Peak troponin I was 42 ng/ml and serum catecholamines were normal. Serial ECGs during hospitalization were comparable to those at admission. Serial echocardiograms were also performed, which showed progressive regression of the findings observed at admission, except for the persistence of posterior wall hypokinesis. The clinical presentation, together with significant troponin I elevation and persisting wall motion abnormalities in a single territory, led us to consider the possibility that, besides stress cardiomyopathy, the patient may have suffered an MI or acute myocarditis. Cardiac magnetic resonance (CMR) was accordingly performed, which revealed subendocardial late enhancement of the posteroinferior wall consistent with an infarction scar in the territory of the circumflex artery.
The discharge diagnoses were MI and stress cardiomyopathy. Six months later, echocardiography and CMR were repeated, which were comparable. The patient has remained asymptomatic.
DiscussionStress cardiomyopathy is not fully understood, but among the possible pathophysiological mechanisms are toxicity arising from catecholamine surge, microvascular dysfunction and multivessel spasm.1 At present there are no definitively established diagnostic criteria; the most commonly used are those of the Mayo Clinic,2 which require the presence of: (1) wall-motion abnormalities typical of the syndrome; (2) absence of obstructive coronary disease or evidence of acute plaque rupture; (3) new ECG abnormalities or modest elevation of cardiac troponin; and (4) absence of pheochromocytoma or myocarditis. There is frequently a physical or emotional stressor, but this is not necessary for the diagnosis.
CMR is useful for differential diagnosis. Typically, patients with stress cardiomyopathy do not present significant late enhancement,3 while subendocardial late enhancement is common in MI and focal or subepicardial late enhancement is frequent in myocarditis.4
In the present case, a marked rise in troponin, typical infarction scar, persistent hypokinesis restricted to a single coronary territory after resolution of other wall motion abnormalities, subendocardial late enhancement documented by CMR and a subocclusive lesion in the vessel irrigating the affected territory, made it clear that the patient had suffered an MI. However, the acute ischemic lesion does not explain the transient ballooning observed in this patient, a typical feature of stress cardiomyopathy. We thus concluded that the patient had suffered an MI and concomitantly developed stress cardiomyopathy, the acute coronary syndrome itself possibly being the stressor.
Although stress cardiomyopathy can occur in patients with obstructive coronary disease, it is exceptionally rare, as pointed out by the authors of the Mayo Clinic criteria.2 We found only one case report of concomitant acute coronary syndrome and stress cardiomyopathy in the same patient.5
However, as this case illustrates, MI does not completely rule out the possibility of stress cardiomyopathy, and may itself be the stressor.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Nobre Menezes M, Silva D, Almeida AG, et al. Um caso raro de cardiomiopatia de stress (Takotsubo) e enfarte agudo do miocárdio concomitantes. Rev Port Cardiol. 2015;34:499.e1–499.e3.