Ventricular wall rupture has become an infrequent complication of myocardial infarction due to widespread use of prompt reperfusion strategies. Patients suffering myocardial infarction with normal coronary arteries seldom develop severe mechanical complications.
We present the case of a patient who developed a ventricular septal rupture following an anteroseptal myocardial infarction and who presented normal coronary arteries at the time of coronary angiography.
A rutura da parede ventricular tornou-se uma complicação pouco frequente em casos de enfarte do miocárdio devido às estratégias de reperfusão urgente. Os pacientes que sofrem enfarte do miocárdio com coronárias normais raramente desenvolvem complicações mecânicas graves.
Apresentamos o caso de um paciente que evoluiu para rutura do septo interventricular na sequência de um enfarte do miocárdio ântero-septal, em que a angiografia coronária mostrou artérias coronárias normais.
We present the case of a patient with anteroseptal myocardial infarction (MI) of unknown duration who presented with post-MI angina and persistent ST elevation and in whom normal coronary arteries and a ventricular septal defect (VSD) were identified on coronary angiography and ventriculography.
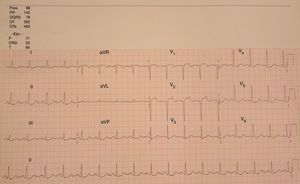
Case reportA 76-year-old woman with no previous history of cardiac disease, dyslipidemia as a cardiovascular risk factor and no other medical conditions presented with intermittent chest pain for four hours compatible with angina. She denied previous symptoms of similar characteristics. On admission, her blood pressure was 105/60 mmHg and heart rate was 90 bpm, and she reported mild persistent pain. The ECG showed complete absence of R waves and ST-segment elevation in leads V1–V2 (Figure 1). Physical examination revealed no abnormalities except for a systolic murmur (III/VI) on the left sternal border and mesocardium. Hand-held echocardiography showed no significant pathologic flows, although the patient's clinical situation made it difficult to carry out a complete assessment. She was immediately referred to the catheterization laboratory for percutaneous coronary intervention (PCI).
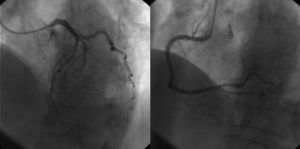
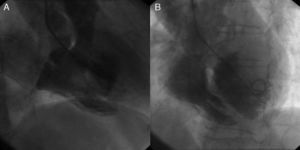
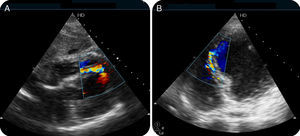
Coronary angiography showed no coronary lesions or signs of partially dissolved thrombus, and coronary flow velocity was normal (Figure 2). The septal branches from the left anterior descending and posterior descending arteries were reviewed carefully, but missing branches, significant atherosclerotic plaques or signs of ostial occlusion were ruled out. Ventriculography, performed to assess wall motion abnormalities, showed a VSD (Figure 3A and B and Online Video 1). Intravascular ultrasound was not performed given the progressive worsening in the patient's clinical situation and evidence of septal rupture after ventriculography. She was transferred to the coronary care unit for clinical stabilization before surgical repair. Transthoracic echocardiography (TTE) confirmed the presence of a 7 mm dissection involving the apical third of the septum (Figure 4A and B). Initially, a direct through-and-through defect resembling a simple rupture was observed (Online Video 2). However, additional images suggested a possible complex rupture with dissection tracts opening to the right ventricle in its mid segment (Online Videos 3 and 4). Initial measurements of cardiac troponin I and creatine kinase were 6.3 ng/ml and 267 IU/l, respectively, slowly decreasing in subsequent analyses. The patient's clinical condition progressively worsened, requiring inotropic support and intra-aortic balloon counterpulsation before emergency surgical patch repair.
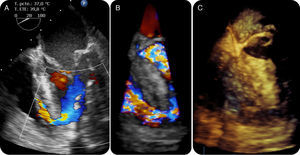
Three hours after successful conclusion of surgery, the patient's condition suddenly worsened. TEE showed complete suture dehiscence (Figure 5A, B and C and Online Videos 5–8) and the patient died before she could be transferred to the operating room to resuture the patch. Consent for autopsy was not granted by the family.
DiscussionSeveral different conditions can lead to myocardial rupture. Acute or subacute MI is the most frequent, but others such as trauma, endocarditis, tumors, and infiltrative diseases have been described.1,2 Although autopsy was not performed in this patient, the absence of previous trauma, diagnosis of cardiac tumor, symptoms of active infection or bacteremia, or prior history of heart failure or other cardiac anomalies makes these other causes less likely. Additionally, echocardiographic examination found no signs suggestive of these alternative diagnoses. Ventricular septal rupture (VSR) complicating acute MI is associated with an increase in post-MI mortality and usually appears either in the first 24 hours after the onset of MI, or 3–5 days after onset.3 The former is related to the development of intramyocardial hematoma, while the latter typically appears in patients in whom reperfusion therapy has failed, and therefore the establishment of emergency PCI programs has dramatically reduced its incidence in recent decades.4 The most common angiographic finding in patients with VSR is complete coronary artery occlusion with few or no collaterals.4
MI with normal coronary arteries (MINCA) can occur as a result of severe vasospasm (related to smoking, cocaine consumption or abnormal increase in vasomotor tone) or of rapid lysis of thrombosis (related to hypercoagulable states and endothelial dysfunction, either primary or as a consequence of drugs, radiation exposure, etc.). However, the full scope of its possible causes and the severity of the associated complications remain to be completely elucidated. MINCA has been described in the past as a relatively benign entity compared to MI due to identifiable coronary artery disease (CAD), with 30-day and one-year mortality rates comparable to patients with low-risk CAD and significantly lower than those with high-risk CAD.3 However, more recent registries have questioned these data, with new findings suggesting that patients with MINCA have similar outcomes and prognosis compared with patients with one- or two-vessel disease presenting with MI.5
Although the incidence of mechanical complications in patients suffering MINCA is unknown, this combination of findings has occasionally been reported.6–10 The pathogenesis of VSR or free ventricular wall rupture in patients who have suffered MINCA has been associated with the sudden onset of ischemia and subsequent abrupt reperfusion, which may be linked to increased neutrophil activity in the damaged area resulting in the release of lytic enzymes following apoptosis.3,5 These typically appear in relation to spontaneous thrombus recanalization, coronary spasm, and myocardial bridging.
In our case, several factors point to the possibility of a prior silent MI, with post-MI angina as the symptom that constituted the patient's chief complaint at the time of admission to the emergency department. The initial elevation of cardiac enzymes was followed by a decrease within hours prior to surgery. Additionally, the ECG showed signs of established necrosis in leads V1 and V2. With this in mind, the possibility of severe coronary spasm or a thrombus that had completely dissolved by the time coronary angiography was performed appear to be the main diagnostic options, with spasm as the first option given the absence of significant atherosclerotic lesions. The septal rupture presented a simple through-and-through component as well as a dissection through the septum toward the mid segment, where it presented a second opening to the right ventricle. This may be due to the progression of the initially established rupture, which seems more likely than a combined etiology. This hypothesis is supported by the low likelihood of ruptures involving the mid and apical portions of the septum being complex (27%) compared to those of the inferobasal portion of the septum, which are complex in up to 94% of cases.11 However, other series have not found significant differences in this distribution.12
ConclusionMechanical complications such as ventricular rupture are a rare but possible complication of MI with normal coronary arteries. Although these are generally believed to have a more benign prognosis, the need for intensive care and observation may not differ significantly from cases of MI with coronary lesions.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.