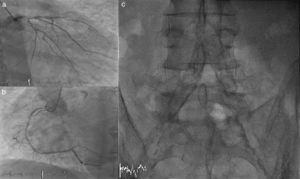
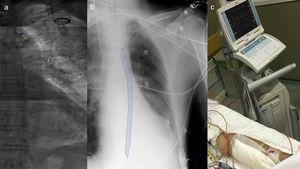
A 76-year-old man, a current smoker with a long-standing history of diabetes, was admitted to our institution due to non-ST segment elevation acute coronary syndrome. He was haemodynamically unstable, with signs of pulmonary oedema and hypotension, so intravenous inotropes were initiated. A transradial angiogram showed severe three-vessel coronary artery disease involving the distal left main coronary artery (Figure 1a and b). A bedside echocardiogram displayed severe left ventricular dysfunction and grade IV mitral regurgitation. The patient presented severely calcified peripheral arteriopathy (Figure 1c) and both inferior limbs were pulseless. A left transbrachial approach was used under fluoroscopy guidance to implant an intra-aortic balloon pump (size 40 ml) through a 7.5 F catheter and counterpulsation was performed successfully (Figure 2). Forearm perfusion was monitored continuously by means of distal pulse oximetry and heparin IV infusion was initiated (bolus of 5000 IU and an activated partial thromboplastin time ratio of 2 times control value as a target). The patient was referred for emergency open-heart surgery a few hours later and multivessel coronary artery bypass graft and mitral valve replacement were carried out uneventfully. Haemodynamic support was maintained for the following 48 hours and the balloon pump could then be removed without thrombotic or ischaemic complications.
(a) Fluoroscopy reconstruction showing antegrade placement of an intra-aortic balloon pump at the descending aorta with the proximal radiopaque marker distal to the emergence of the subclavian artery (blue arrow). (b) Bedside chest X-ray on postoperative day 1 (balloon pump position is highlighted in blue). (c) Effective 1:2 counterpulsation through 7 Fr transbrachial access.
The intra-aortic balloon pump offers limited circulatory support and did not show prognostic benefit in recent clinical trials. For this reason, its use is not routinely recommended in patients with cardiogenic shock according to the latest guidelines. Nevertheless, it is still widely available in most centres and provides an increase in diastolic coronary flow that might be beneficial in patients with high risk coronary anatomy and left ventricular impaired systolic function until revascularisation is performed. Therefore, its use as a bridge to coronary artery bypass surgery is still largely recommended.
The need for less-aggressive vascular access, using an introducer of much smaller size compared to other peripheral circulatory assist devices, may be of interest for elderly patients or patients with severe systemic arteriosclerosis. A left transbrachial percutaneous approach may be a safe and effective alternative if femoral artery access cannot be achieved. Adequate selection of the sheath size according to pre-implantation brachial angiography (7 to 8F), continuous distal perfusion monitoring and early anticoagulation infusion are key points in avoiding potential vascular complications.
Conflicts of interestThe authors have no conflicts of interest to declare.