Heart failure (HF) is a progressive and multifactorial clinical syndrome that can be viewed as the final path of heart disease. It affects more than 15 million people living in Europe and this number is expected to increase significantly as the population ages.1 As the final common pathway of heart disease, HF is associated with high mortality, at least 50% at 5 years. HF contributes to more than two million hospital stays per year in Europe, and is the most common cause of hospitalizations over the age of 65 years and is associated with low quality of life.1
Notwithstanding these facts, the awareness of the syndrome among the general population, health professionals, and decision-makers is poor. This is reflected in suboptimal prevention and clinical management, inappropriate adherence to therapy, low treatment reimbursements and scarce research funding.2,3
In this issue of the Journal, Silva-Cardoso et al.4 describe 16 statements belonging to four major HF domains, defined by a group of Portuguese HF experts and designed to improve HF care in Portugal (Figure 1). These statements were validated by a large Delphi-like panel encompassing cardiologists, internists, general practitioners, and nurses interested in or dedicated to HF.
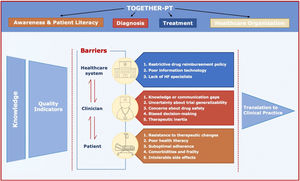
Barriers and facilitators of knowledge translation in heart failure.4,12
The authors establish four critical statements to raise HF patient literacy and awareness of the syndrome. Most HF features including morbidity and impact on survival are unknown to the general population and even among patients.2 The prognostic impact of HF is similar to more common forms of cancer concerning hospitalizations and five-year case mortality, which supports the concept that HF is as malignant as cancer.5,6 Moreover, a large proportion of patients with cancer will die of cardiovascular disease including HF. However, public perception and investment are still mainly focused on oncology, with HF still falling behind when it comes to the true perception of the associated prognosis and funding invested in research.3 Despite all therapeutic developments, HF should be perceived as the malignant phase of heart disease deserving at least a similar investment to cancer in evidence-based treatments and research.
Due to the progressive nature of HF, early diagnosis is crucial to start pharmacologic and device interventions that reverse or slow the progression of cardiac dysfunction and change the natural history of HF.1 The importance of early diagnosis of HF is underscored by the authors through four dedicated statements. Since the diagnosis of HF requires the presence of symptoms and/or signs of HF and objective evidence of structural and/or functional abnormality of the heart, echocardiography, and measurement of natriuretic peptides (NP) are essential for this purpose.1 Furthermore, the detection of structural heart disease, abnormal cardiac function, or elevated NP levels enables the identification of patients with pre-HF (ACC/AHA stage B), in the absence of current or prior symptoms and/or signs of HF.7 This population with subclinical heart disease calls for the development of effective treatment strategies for the prevention of HF. The PORTuguese Heart failure Observational Study (PORTHOS)8 designed to determine the HF prevalence in the Portuguese population will also identify the burden of pre-HF.
Combined pharmacologic therapy including beta-blocker, angiotensin receptor-neprilysin inhibitor, mineralocorticoid receptor antagonist and newer sodium-glucose cotransporter-2 (SGLT-2) inhibitor can reduce the relative risk of all-cause death by 70% and HF hospitalization by 80% in patients with HF with reduced ejection fraction (EF).9 The benefit of these four fantastic drugs in reducing cardiovascular death or HF hospitalization and improving quality of life can be extended to patients with mildly reduced EF and even for those with preserved EF receiving SGLT-2 inhibitor. Although this impressive impact on the natural history of HF, contemporary real-world studies demonstrate a clear underuse of these guideline-directed medical therapies (GDMT).10,11 The authors describe four statements highlighting the need for adherence to guideline treatment recommendations. Barriers to the implementation of HF clinical guidelines have been described at the healthcare system, clinician, and patient level that must be addressed comprehensively12 (Figure 1).
Finally, the authors proposed four statements to improve the organization of the HF healthcare system. In addition to the hierarchy of three levels of care, primary care, regional hospitals, and central hospitals, they propose the development of a single, integrated, shared electronic health record (EHR) combined with quality of care indicators (QI).13 The European Society of Cardiology recognizes the need for reporting QI and outcomes of cardiovascular care through continuous clinical registries to assess adherence to clinical guidelines and develop quality improvement programs designated by the EuroHeart project.14,15 A single shared EHR with encoded demographic and clinical data can be the platform for launching a high-quality continuous clinical registry harmonized with the EuroHeart. Furthermore, EHR can be used to alert the clinician to prescribe dose targeted GDMT, a strategy that led to significantly higher rates of GDMT at 30 days when compared with usual care.16
Conflicts of interestThe authors have no conflicts of interest to declare.