Atrial fibrillation (AF) is the most common sustained arrhythmia, with significant burden for patients. Catheter ablation is safe and superior for symptom improvement. The purpose of this work was to assess how clinical practice compares with current scientific evidence and quality indicators for AF ablation.
MethodsThe Portuguese Association of Arrhythmology, Pacing and Electrophysiology conducted a prospective registry among Portuguese centers to assess clinical practice regarding management of patients referred for ablation and the methodology used in the procedures and related outcomes.
ResultsA total of 337 patients were referred for ablation, 102 (37.91%) female, age 65 (56–70.8) years. The median CHADS2-VaSC2 thromboembolic risk score was 2 (1–3), and 308 (92.49%) were on anticoagulants. AF was mainly paroxysmal (224, 66.97%) and symptomatic (mEHRA score 3; 2–3). Before ablation most patients (273, 81.49%) underwent cardiac computed tomography and only 24 (7.36%) procedures were performed with uninterrupted anticoagulation. For ablation, Carto® (194; 59.15%) and Ensite® (55; 16.77%) were mainly used, and the preferential strategy was pulmonary vein isolation (316; 94.61%). Acute complications occurred in five (1.49%) patients, while most had symptom improvement at one month (200; 86.21%), sustained at one year. There were 40 (12.6%) relapses within 30 days and 19 (26.39%) at one year.
ConclusionsIn a population of patients with AF referred for ablation in Portuguese centers, patient management is provided according to the best scientific evidence and there is a high standard of practice with respect to the quality of AF ablation practice.
A fibrilhação auricular (FA) é a arritmia mantida mais comum, com ónus significativo sobre os doentes. A ablação por cateter é segura e superior para a melhoria sintomática. O objetivo deste trabalho é comparar a prática clínica com a evidência científica atual e indicadores de qualidade estabelecidos.
MétodosRegisto prospetivo conduzido pela Associação Portuguesa de Arritmologia, Pacing e Eletrofisiologia, em centros portugueses, avaliando a prática clínica na abordagem de doentes referenciados para ablação, metodologia utilizada e respetivos resultados.
ResultadosForam referenciados 337 doentes, 102 (37,91%) do sexo feminino e idade 65 (56-70,8) anos. O risco tromboembólico era 2 (1-3), encontrando-se 308 (92,49%) sob hipocoagulação oral. Maioritariamente paroxística (224, 66,87%) e sintomática (mEHRA score 3; 2-3), previamente à ablação, a maioria (273, 81,49%) realizou TC cardíaca, com apenas 24 (7,36%) procedimentos realizados sem interrupção de hipocoagulação. Com uso predominante de sistema mapeamento Carto® (194; 59,15%) e Ensite® (55; 16,77%), a estratégia preferencial foi o isolamento das veias pulmonares (316; 94,61%). Ocorreram cinco complicações agudas (1,49%), tendo a maioria dos doentes melhoria sintomática no primeiro mês (200; 86,21%), mantida no primeiro ano. Aos 30 dias houve 40 (12,6%) recidivas, 19 após um ano (26,39%).
ConclusõesNuma população de doentes com fibrilhação auricular referenciados para ablação em centros portugueses, a abordagem dos doentes está enquadrada na melhor evidência científica recomendada e existe um elevado padrão de qualidade no que concerne à prática do procedimento de ablação de FA.
Atrial fibrillation (AF) is the most common sustained arrhythmia worldwide, with an estimated prevalence of 2–4% in adulthood. With increased life expectancy, together with more accurate and intensive diagnostic methods, an estimated 2.3-fold rise is expected, with a lifetime risk of developing AF of one in three Europeans at the age of 55 years.1
AF is a complex disease in terms of management, with important morbidity and mortality, and has a significant impact on patients’ quality of life as well as a considerable socioeconomic burden. The techniques of AF ablation have evolved in the last three decades, and are currently dominated by percutaneous catheter ablation, which is available in the majority of hospitals, with a low periprocedural complication rate. As stated in the most recent (2020) European Society of Cardiology (ESC) guidelines,1 catheter ablation is a safe and superior treatment for symptom improvement and maintenance of sinus rhythm and a well validated treatment for the prevention of AF recurrence.
According to the latest data published by the European Heart Rhythm Association (EHRA)2,3 with information from 2016, AF ablation is one of the commonest electrophysiological procedures (reflecting a paradigm shift in the treatment of this arrhythmia), with substantial growth since 2007. Portugal is one of the top three southern European countries in AF ablation, with 478% growth and 82 ablations per million population (mean of 110 ablations per million population in ESC members). Unpublished official data presented by the Portuguese Association of Arrhythmology, Pacing and Electrophysiology (APAPE) show that 1633 AF ablations were performed in 2021 – a 35.2% increase from the previous year and corresponding to 157.86 ablations per million population.
A consensus statement on AF ablation published in 20174 laid out the periprocedural strategies, techniques, and endpoints for improving outcomes and safety with the use of ablation for AF treatment. However, there is little published information regarding the standards of practice for AF catheter ablation in the real world.
ObjectivesThe purpose of this work was to collect continuous data on national activity regarding AF ablation, analyzing characteristics and indications among patients undergoing ablation and describing procedural characteristics and the frequency of associated complications. We aimed thereby to determine how clinical practice in Portuguese centers that perform AF ablation compares with the current scientific evidence and quality indicators for AF ablation as stated in the 2017 HRA/EHRA/ECAS/APHRS/SOLACE international consensus document4 and the 2015 Atrial Fibrillation Network/EHRA consensus conference.5
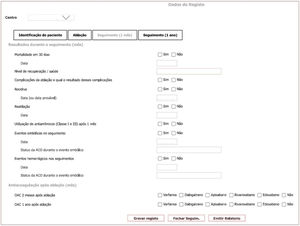
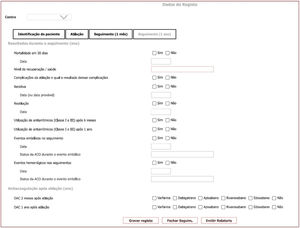
MethodsStudy populationAPAPE conducted a prospective registry between February 1, 2020 and January 31, 2022 among Portuguese electrophysiology laboratories that perform AF ablation, to assess clinical practice regarding the management of patients referred for ablation, the methodology used in the procedures, and their respective outcomes. All participating centers were asked to include consecutive patients who underwent AF ablation during the study period, by completing an online questionnaire (Figures 1–4) with prespecified questions. There were no inclusion criteria to enter the study besides the need for AF ablation being performed. It was not mandatory to respond to all the questions in the survey, and so whenever there is missing information regarding specific parameters in the analysis, the total number of patients for whom complete information is available is given.
Baseline patient characteristicsRegarding patient characteristics, we sought to assess risk factors for AF incidence and recurrence, including body mass index, smoking, and the presence of hypertension, dyslipidemia, and obstructive sleep apnea.
Patient thromboembolic risk (based on the CHADS2-VaSC2 score) was also assessed, as was the presence of significant structural cardiac disease (left atrial [LA] dilatation, moderate/severe mitral regurgitation, and impaired left ventricular ejection fraction [LVEF]).
The type of AF (paroxysmal, persistent, or long-standing persistent) was documented in all patients along with previous attempts to control rhythm with AF ablation.
Indication for atrial fibrillation ablation and anticoagulation therapyThe reporting hospitals that agreed to participate in the study stated the indication of patients for performing AF ablation, including patient symptoms (based on the modified European Heart Rhythm Association [mEHRA] score) and previous attempts at rhythm control other than ablation (pharmacologic or electrical cardioversion). The use of anticoagulation was assessed in all patients, as were types of drugs used and respective dosages.
Atrial fibrillation ablation procedureWith respect to AF ablation procedures, data were collected to appraise the strategies used, safety measures and guideline adherence. The authors aimed to assess the quality of AF practice as per the 2017 HRA/EHRA/ECAS/APHRS/SOLACE international consensus document.4 The data requested for quality assessment were decided based on the recommendations made in this document, which states that each recommendation was accepted if at least 80% of the writing committee was in agreement, and the authors accordingly used this cutpoint for each recommendation, to determine whether the procedure was performed in accordance with the suggested standard of care.
Regarding periprocedural anticoagulation, we determined whether procedures were performed with or without interruption of anticoagulation, whether unfractionated heparin (UFH) was used to maintain therapeutic anticoagulation during ablation, and the respective monitoring strategy (using activated clotting time [ACT]). We assessed the time to reintroduction of oral anticoagulation (if interrupted) and whether parenteral anticoagulation was used after the procedure, and the status of anticoagulation at discharge. The use of transesophageal echocardiography (TEE) and/or cardiac computed tomography (CT) to exclude LA thrombus and to assess LA anatomy was also determined for every patient who underwent ablation.
With respect to ablation, we asked the responding centers to report whether general anesthesia and an esophageal thermometer was used. The use and type of LA mapping and energy for ablation was assessed, as was the method of choice for performing AF ablation (pulmonary vein isolation and/or additional ablation lines) as well as confirmation of acute success (maneuvers to confirm block).
For every ablation procedure, the occurrence of acute complications and their respective outcomes were assessed.
Outcomes of atrial fibrillation ablation at one month and one year post procedureThe outcomes of patients treated by ablation for rhythm management were assessed and complications were defined as detailed in the 2017 HRA/EHRA/ECAS/APHRS/SOLACE international consensus document.4 Reported deaths and ablation-related complications within one month and one year of the procedure were assessed. Likewise, we obtained patient-reported outcomes at one month and one year, the occurrence of AF relapse (after a three-month blanking period) and the need for redo procedures. As this was an observational study intended to reflect real-life practice, the authors did not prespecify monitoring strategies during follow-up and allowed centers to perform their usual institutional follow-up. As stated in the consensus document,4 follow-up should include a minimum of a 12-lead electrocardiogram at each patient visit (for which no time interval was specified), at least one 24-hour Holter monitoring in the first year, and in the event of symptoms, a symptom-driven event recording in paroxysmal AF. Additional 24-hour Holter monitoring at six months was specified in the event of persistent AF. In the ESC AF guidelines,1 follow-up is only recommended at three months after ablation and annually thereafter.
With respect to patient management and outcomes, we also sought to record the use of antiarrhythmic drug therapy one month, six months and one year after ablation and the mainstay of anticoagulation use at two months and one year post procedure. The occurrence of thromboembolic and bleeding events in the first month and first year after ablation was assessed.
Statistical analysisAll analysis were performed using Stata® version 12 (StataCorp LLC, College Station, TX). Data are presented as median and lower and upper quartiles (Q1–Q3) for continuous variables and as absolute number and percentage for categorical variables.
After testing for normality of the population with the Shapiro–Wilk test, continuous variables were compared with the t test and categorical variables with Fisher's exact test. A value of p<0.05 was considered statistically significant and logistic regression analysis using significant variables was performed to determine independent predictors.
Ethics disclosuresIn each center, data were collected prospectively using a standardized data collection form (Figures 1–4) accessed online by all the participating hospitals. Patient identification was recorded in the participating centers but was not transferred to APAPE and so the compiled data remained anonymous. All patients provided written informed consent, and the study was approved by the ethics committee of the participating hospitals.
This study complies with the declaration of Helsinki.
ResultsStudy populationSeven electrophysiology laboratories and the respective hospital centers nationwide participated in the survey, corresponding to 31.82% of the 22 national centers that perform AF ablation. During the study period, 337 patients undergoing AF ablation were included (11.87% of all 2840 AF ablations performed in Portugal throughout the study period between 2020 and 2022). Among the included patients, all underwent the planned ablation procedure, 293 (86.9%) had a complete record at inclusion and 253 (75.07%) completed follow-up. Overall, 127 (37.7%) patients had at least one missing item among the totality of the survey's questions.
Baseline patient characteristicsOf the included patients, 102 (37.91%) were female (68 records, 20.17%, had missing data regarding this question) and their median age was 65 (56–70.8) years (Table 1). A total of 252 (75.68%; n=333) patients were overweight, with a median body mass index of 27.68 kg/m2 (25.06–30.82), and 25 (7.46%; n=335) patients were smokers. Hypertension had been diagnosed in 170 (50.75%; n=335) patients, dyslipidemia in 125 (37.20%; n=336), and 29 (8.81%; n=329) patients had been diagnosed with obstructive sleep apnea.
Baseline patient characteristics.
| na | ||
|---|---|---|
| Female, n (%) | 102 (37.91%) | 269 |
| Age, years, median (Q1–Q3) | 65 (56–70.8) | 337 |
| BMI, median (Q1–Q3) | 27.68 (25.06–30.82) | 333 |
| Smokers, n (%) | 25 (7.46%) | 337 |
| Former smokers, n (%) | 42 (12.53%) | 337 |
| Hypertension, n (%) | 170 (50.75%) | 335 |
| Dyslipidemia, n (%) | 125 (37.20%) | 336 |
| Obstructive sleep apnea, n (%) | 29 (8.81%) | 329 |
| CHADS2-VaSC2 score, median (Q1–Q3) | 2 (1–3) | 337 |
| Severe LV systolic dysfunction, n (%) | 19 (5.74%) | 331 |
| LVEF, %, median (Q1–Q3) | 55 (50–60) | 122 |
| Moderate to severe MR, n (%) | 16 (4.77%) | 335 |
| LA dilatation, n (%) | 202 (73.19%) | 276 |
| LA volume, ml/m2, median (Q1–Q3) | 42 (34–52) | 267 |
| LA diameter, mm, median (Q1–Q3) | 42 (39–48.5) | 75 |
| Paroxysmal AF, n (%) | 224 (16.12%) | 335 |
| Persistent AF, n (%) | 54 (16.12%) | 335 |
| Long-standing persistent AF, n (%) | 57 (17.01%) | 335 |
| Previous AF ablation, n (%) | 50 (16.84%) | 297 |
AF: atrial fibrillation; BMI: body mass index; LA: left atrial; LV: left ventricular; LVEF: left ventricular ejection fraction; MR: mitral regurgitation; Q1–Q3: lower and upper quartiles.
The median thromboembolic risk of this cohort, assessed by their CHADS2-VaSC2 score, was 2 (1–3), found in 87 (29.49%) patients, while 23 patients (7.8%) had a very high risk CHADS2-VaSC2 score (≥4). Regarding the existence of structural cardiac disease, there were 19 (5.74%; n=331) patients with severe left ventricular dysfunction (LVEF <30%); median LVEF was 55% (50%–60%). Moderate to severe mitral regurgitation was present in 16 (4.77%; n=335) patients and LA dilatation in 202 (73.19%; n=276). Measurement of LA volume over diameter was the main method used to assess LA dilatation, median indexed LA volume being 42 (34–52; n=267) ml/m2 (Table 1).
The main type of AF in this cohort was paroxysmal (224, 66.87% patients; n=335), with similar proportions of patients having persistent (54, 16.12%) or long-standing persistent AF (57, 17.01%) (Table 1). There were previous attempts at rhythm control with AF ablation in 50 (16.84%; n=297) patients.
Indication for atrial fibrillation ablation and anticoagulation therapyRegarding indication for AF ablation, this was mainly driven by mild to moderate AF symptoms (Table 2), with a median mEHRA score of 3 (2–3). There were 261 symptomatic patients (92.55%; n=282), of whom 101 (35.82%) were in mEHRA class 2, while most were in class 3 (135, 47.87%).
Indication for atrial fibrillation ablation and anticoagulation therapy.
| na | ||
|---|---|---|
| mEHRA score, median (Q1–Q3) | 3 (2–3) | 337 |
| II, n (%) | 101 (35.82%) | 282 |
| III, n (%) | 135 (47.87%) | 282 |
| IV, n (%) | 25 (8.87%) | 282 |
| Previous rhythm control attempts, n (%) | 285 (85.59%) | 333 |
| Previous electrical cardioversion, n (%) | 65 (24.53%) | 333 |
| VW class I antiarrhythmic therapy, n (%) | 112 (42.44%) | 333 |
| VW class III antiarrhythmic therapy, n (%) | 172 (66.41%) | 333 |
| Anticoagulant therapy, n (%) | 308 (92.49%) | 333 |
| DOAC therapy, n (%) | 303 (98.34%) | 333 |
| Dabigatran, n (%) | 32 (9.61%) | 333 |
| Apixaban, n (%) | 62 (18.62%) | 333 |
| Rivaroxaban, n (%) | 150 (45.05%) | 333 |
| Edoxaban, n (%) | 59 (17.72%) | 333 |
| Warfarin, n (%) | 5 (1.50%) | 333 |
| Dual antithrombotic therapy, n (%) | 3 (1.05%) | 333 |
| No antithrombotic therapy, n (%) | 25 (7.51%) | 333 |
DOAC: direct oral anticoagulant; mEHRA: modified European Heart Rhythm Association; Q1–Q3: lower and upper quartiles; VW: Vaughan Williams.
Previous attempts at rhythm control were made in 285 (85.59%; n=333) patients (Table 2), 65 of whom (24.53%) underwent electrical cardioversion; 112 (42.44%) patients were under treatment with Vaughan Williams class I antiarrhythmics and 172 (66.41%) were under class III therapy.
With respect to anticoagulation, 308 (92.49%; n=333) patients were on anticoagulant therapy. Of these, 303 (98.34%) were taking direct oral anticoagulants (DOACs), of whom 19 (6.27%) were eligible for a lower dose. Overall, 32 (9.61%) patients were taking dabigatran, 62 (18.62%) apixaban, 150 (45.05%) rivaroxaban and 59 (17.72%) edoxaban (Table 2).
Atrial fibrillation ablation procedureConcerning AF ablation, the procedure was performed under general anesthesia in 103 (30.93%; n=333) patients. Regarding procedure planning and LA thrombus exclusion, most patients (273, 81.49%; n=335) underwent cardiac CT, while TEE was performed in 130 (38.81%; n=335) (Table 3).
Periablation management.
| na | ||
|---|---|---|
| General anesthesia, n (%) | 103 (30.93%) | 333 |
| Cardiac CT, n (%) | 273 (81.49%) | 335 |
| TEE, n (%) | 130 (38.81%) | 335 |
| Cardiac CT+TEE, n (%) | 69 (20.6%) | 335 |
| Uninterrupted anticoagulation, n (%) | 24 (7.36%) | 326 |
| Anticoagulation interrupted for 12 h, n (%) | 27 (8.28%) | 326 |
| Anticoagulation interrupted for 24 h, n (%) | 114 (34.97%) | 326 |
| Anticoagulation interrupted for 48 h, n (%) | 161 (49.39%) | 326 |
| UFH before/immediately after TSP, n (%) | 326 (97.6%) | 334 |
| ACT monitoring for anticoagulation, n (%) | 331 (99.7%) | 332 |
| ACT, s, median (Q1–Q3) | 310 (300–320) | 332 |
| Oral anticoagulation restart, h, median (Q1–Q3) | 5 (5–6) | 297 |
| Parenteral anticoagulation bridging, n (%) | 7 (2.36%) | 297 |
| Post-ablation oral anticoagulation, n (%) | 332 (99.10%) | 335 |
| DOAC therapy, n (%) | 330 (99.39%) | 335 |
| Dabigatran, n (%) | 34 (10.15%) | 335 |
| Apixaban, n (%) | 67 (20%) | 335 |
| Rivaroxaban, n (%) | 168 (50.15%) | 335 |
| Edoxaban, n (%) | 58 (17.31%) | 335 |
| Warfarin, n (%) | 5 (1.50%) | 333 |
ACT: activated clotting time; CT: computed tomography; DOAC: direct oral anticoagulation; TEE: transesophageal echocardiography; TSP: transseptal puncture; UFH: unfractionated heparin.
With respect to periablation anticoagulation, 24 (7.36%; n=326) procedures were performed without interrupting anticoagulation, while anticoagulation was interrupted for most ablations, for 24 h (114, 34.97%) or for at least 48 h (161, 49.39%). UFH was used before or immediately after transseptal puncture in 326 (97.60%; n=334) patients. ACT was used to monitor anticoagulation level in 331 (99.7%; n=332) patients, with a median ACT of 310 (300–320) s. After the procedure, the median time before restarting anticoagulation was 5 (5–6) h and seven patients (2.36%; n=297) had parenteral anticoagulation bridging. At discharge, 332 (99.10%; n=335) patients were on anticoagulant therapy, with DOACs in 330 (99.39%) patients and 20 (5.97%) patients eligible for reduced dose. The distribution among DOACs was similar to that before ablation; three patients (0.89%) were not anticoagulated after ablation.
AF ablation procedures were performed with three-dimensional (3D) mapping systems in 251 (76.52%; n=328) patients (Table 4), using Carto® in 194 (59.15%), Ensite® in 55 (16.77%) and Rhythmia® in two (0.61%). Radiofrequency energy was used for ablation in 246 (73.87%; n=333) patients and cryoenergy in 87 (26.13%). The power delivered in the LA posterior wall was lower in 246 (100%; n=329) procedures (a class I recommendation) and an esophageal thermometer was used in only two (0.59%; n=334) patients. The preferential strategy for AF ablation was pulmonary vein isolation (PVI), used in 316 (94.61%; n=334) patients. Successful PVI was reported in 322 (98.17%; n=328) patients, confirmed by entry block in 241 (85.77%; n=281). Additional ablation lines were performed in 40 (12.05%; n=332) patients and pacing maneuvers to confirm block of these lines were performed in 39 (97.5%; n=330) patients (Table 4). Typical atrial flutter was previously diagnosed or occurred during AF ablation in 51 (15.41; n=331) patients and cavotricuspid isthmus ablation lines were created in 43 (84.3%; n=333) patients.
Atrial fibrillation procedure.
| na | ||
|---|---|---|
| 3D mapping system during ablation, n (%) | 251 (76.52%) | 328 |
| Carto®, n (%) | 194 (59.15%) | 328 |
| Ensite®, n (%) | 55 (16.77%) | 328 |
| Rhythmia®, n (%) | 2 (0.61%) | 328 |
| RF energy, n (%) | 246 (73.87%) | 333 |
| Cryoenergy, n (%) | 87 (26.13%) | 333 |
| Lower power delivered to LA posterior wall, n (%) | 246 (100%) | 329 |
| Esophageal thermometer use, n (%) | 2 (0.59%) | 334 |
| Preferential PVI, n (%) | 316 (94,61%) | 334 |
| Successful PVI, n (%) | 322 (98.17%) | 322 |
| Entry block confirmation, n (%) | 241 (85.77%) | 281 |
| Additional ablation lines, n (%) | 40 (12.05%) | 332 |
| Pacing maneuvers to confirm block, n (%) | 39 (97.5%) | 330 |
| Typical atrial flutter, n (%) | 51 (15.41%) | 331 |
| CTI ablation, n (%) | 43 (84.3%) | 333 |
| Acute complication of AF ablation, n (%) | 5 (1.49%) | 334 |
| Major complications, n (%) | 1 (0.29%) | 334 |
3D: three-dimensional; AF: atrial fibrillation; CTI: cavotricuspid isthmus; LA: left atrial; PVI: pulmonary vein isolation; RF: radiofrequency.
Acute complications during AF ablation occurred in five (1.49%; n=334) patients, of which four were minor without additional intervention and one was major, requiring emergency cardiac surgery.
Outcomes of atrial fibrillation ablation at one month and one year post procedureAt the end of the first month post ablation, there were two reported deaths (0.73%; n=275) and six (2.18%) procedure-related complications, with no additional deaths or complications at one year after the procedure (Table 5). Regarding patient recovery and symptoms, at one month there were 200 (86.21%; n=232) patients with symptom improvement, 29 (12.5%) reporting no change in baseline symptoms and three (1.29%) with worsened quality of life. The 30-day median mEHRA score was 2 (1–2) (p<0.000 from baseline). At one year post ablation, the recovery rate was sustained, with no difference from the first month post ablation (p=0.66); the median mEHRA score was 1 (1–2) (p<0.000 from baseline) (Table 5).
Outcomes of atrial fibrillation ablation.
| na | ||
|---|---|---|
| 30-day death, n (%) | 2 (0.73%) | 275 |
| 30-day complications, n (%) | 6 (2.18%) | 275 |
| 30-day embolic events, n (%) | 1 (0.37%) | 275 |
| 30-day bleeding events, n (%) | 2 (0.74%) | 275 |
| 30-day symptom improvement, n (%) | 200 (86.21%) | 275 |
| 30-day worsening of symptoms, n (%) | 3 (1.29%) | 275 |
| 30-day mEHRA score, median (Q1–Q3) | 2 (1–2) | 275 |
| 30-day AF relapse, n (%) | 40 (12.6%) | 274 |
| Redo AF ablation procedure, n (%) | 4 (10%) | 274 |
| 1-year death, n (%) | 0 | 275 |
| 1-year complications, n (%) | 0 | 275 |
| 1-year embolic event, n (%) | 0 | 275 |
| 1-year bleeding event, n (%) | 0 | 275 |
| 1-year symptom improvement, n (%) | 48 (81.36%) | 59 |
| 1-year worsening of symptoms, n (%) | 1 (1.7%) | 59 |
| 1-year mEHRA score, median (Q1–Q3) | 1 (1–2) | 59 |
| 1-year AF relapse, n (%) | 19 (26.39%) | 72 |
| Redo AF ablation procedure, n (%) | 3 (15.8%) | 72 |
AF: atrial fibrillation; mEHRA: modified European Heart Rhythm Association.
In the first 30 days of the post-ablation blanking period, 40 (12.6%; n=274) patients suffered AF relapse, of whom four (10%; n=273) underwent a redo procedure in this period. AF relapse at 30 days was associated with obstructive sleep apnea (p=0.029), greater body mass index (p=0.0078) and previous LA ablation (p=0.0002), and was less likely if PVI was the method for AF ablation. Logistic regression analysis revealed that only previous LA ablation was independently associated with more AF relapses (p=0.000, odds ratio [OR] 3.59; 95% confidence interval [CI] 1.75–7.39), and PVI was associated with fewer relapses (p=0.034, OR 0.28; 95% CI 0.09–0.91) (Table 6).
Predictors of atrial fibrillation relapses.
| 30 days | 1 year | |
|---|---|---|
| Obstructive sleep apnea | p=0.029 | NS |
| BMI | p=0.0078 | NS |
| Previous ablation in the left atrium | p=0.0002 (OR 3.59; 95% CI 1.75–7.39) | NS |
| PVI as preferential method of ablation | p=0.034 (OR 0.28; 95% CI 0.09–0.91) | NS |
| Increased LA diameter | NS | p=0.039 |
| AF type | NS | p=0.019 (OR 19.03) |
| mEHRA score improvement | NS | p=0.0092 |
| AF relapse at 30 days | – | p=0.004 |
AF: atrial fibrillation; BMI: body mass index; CI: confidence interval; LA: left atrial; mEHRA: modified European Heart Rhythm Association; NS: not significant; OR: odds ratio; PVI: pulmonary vein isolation.
At the end of the first-year post ablation, there were AF relapses in 19 (26.39%; n=72) patients and three (15.8%) underwent a redo procedure at a median of 229 (166–268) days after the index procedure. The occurrence of relapses at one year was associated with increased LA diameter (p=0.039), AF type (p=0.0003), lack of improvement in mEHRA score (p=0.01) at 30 days and at one year (p=0.0092), and the occurrence of AF relapse at 30 days (p=0.004) (Table 6). There were no differences in major outcomes regarding AF relapse between volume of procedures performed by center per year (<100, 100–299, or >300).
Regarding antiarrhythmic drug therapy, at 30 days post ablation 212 (77.94%; n=272) patients were taking Vaughan Williams class I or class III antiarrhythmic drugs, and at six months and one year post ablation, 51 (70.83%; n=72) and 45 (62.5%) patients were on antiarrhythmic drug therapy, respectively (Table 7).
Patient management after atrial fibrillation ablation.
| na | ||
|---|---|---|
| Class I or III antiarrhythmic therapy at 30 days, n (%) | 212 (77.94%) | 272 |
| Class I or III antiarrhythmic therapy at 6 months, n (%) | 51 (70.83%) | 72 |
| Class I or III antiarrhythmic therapy at 1 year, n (%) | 45 (62.5%) | 72 |
| Anticoagulation therapy at 2 months, n (%) | 274 (99.64%) | 275 |
| Dabigatran, n (%) | 29 (10.55%) | 275 |
| Apixaban, n (%) | 53 (19.27%) | 275 |
| Rivaroxaban, n (%) | 143 (52%) | 275 |
| Edoxaban, n (%) | 47 (17.09%) | 275 |
| Warfarin, n (%) | 2 (0.73%) | 275 |
Two months after AF ablation, 274 (99.64%; n=275) patients were still on anticoagulant therapy (two [0.73%] on warfarin, 29 [10.55%] on dabigatran, 53 [19.27%] on apixaban, 143 [52%] on rivaroxaban and 47 [17.09%] on edoxaban). By the end of the first year, 73 (93.33%; n=75) patients were still on anticoagulant therapy, with similar rates between DOACs and warfarin (Table 7).
During the first month post ablation, one (0.37%; n=272) patient had an embolic event (under full-dose anticoagulant therapy) and two (0.74%; n=271) patients had a bleeding event (both under anticoagulant therapy). No events occurred after this period or in the first year after ablation (Table 5).
DiscussionIn recent years, AF has been diagnosed with greater frequency, due on one hand to increases in predisposing conditions and on the other hand to heightened awareness and earlier and systematic diagnosis.5 In our study, we analyzed a population of patients with previously diagnosed AF for whom a strategy of rhythm control with ablation was planned. The 337 patients included, reported by a third of all electrophysiological centers that perform AF ablation in Portugal, corresponded to 11.85% of all AF ablations performed in the two-year study period, reflecting a significant increase in the number of patients eligible for this rhythm control strategy in the country (with consistent increases in ablations performed of 15.3%, 37% and 26.8% from 2015 to date) and a surrogate of an increase in AF diagnosis.6,7
As AF is difficult to prevent, interventions for risk factor control to reduce incident AF should be increased, and there are significant measures that should be applied to improve care of patients diagnosed with the condition.8 The 2020 ESC guidelines for the diagnosis and management of AF1 propose a structured characterization of AF and an integrated approach to patient management. We identified a population of predominantly male (62.06%) AF patients with a median age of 65 years to whom ablation was offered, which is representative of the Portuguese population currently referred for ablation.6,7 This was a population with a high prevalence of risk factors for AF, including a significant proportion of overweight patients, with high rates of smoking, dyslipidemia and hypertension, which identifies a population at increased risk for whom an integrated care pathway should be offered with upstream therapy, to reduce recurrence. On the other hand, the proportion of patients with obstructive sleep apnea was low, probably reflecting the choice of medical treatment in this population with increased AF recurrence after ablation and for whom recurrences can be reduced with directed apnea treatment.1,4,8 While patients referred for ablation with moderate to severe structural cardiac disease was low (5.74% patients had LVEF<30% and only 4.77% had moderate to severe mitral regurgitation), the proportion of patients with LA dilatation was high (73.19%). This finding is in agreement with recent guidelines and published studies,9 which indicate that in highly symptomatic patients with structural cardiac disease there is a role for AF ablation, which can improve survival as well as symptoms (there is evidence for more robust efficacy if LVEF >25%). This is a population that on one hand could be more at risk from the procedure, but that on the other hand are likely to have a survival benefit and to whom ablation should be offered. Although LA diameter continues to be used to assess LA dilatation, in our population more robust volumetric measurements are increasingly used to assess LA structure before ablation. This issue should be addressed in further studies, to determine whether more accurate measurements of structural LA disease would help select patients who would benefit more from AF ablation.
With respect to AF characterization, most of the patients referred for ablation had paroxysmal AF (66.87%), while persistent and long-standing persistent AF (16.12% and 16.84%) were less frequent, which we believe reflects the current level of evidence for AF ablation in the different subsets of AF patients to whom the procedure is offered. The median mEHRA score was 3, with 92.55% of patients being symptomatic; additionally, previous failed attempts at rhythm control had been made in 85.59% of patients (24.53% with electrical cardioversion, 42.44% with class I antiarrhythmic therapy, 66.41% with class III antiarrhythmic therapy and 16.84% with previous AF ablation). These findings are in line with the most recent guidelines,1 which provide more robust evidence in symptomatic patients with paroxysmal AF and with failed previous attempts at rhythm control who should be offered AF ablation. However, patients with persistent and long-standing persistent highly symptomatic AF should also be offered a rhythm control strategy and ablation should be considered, and as such, they are also represented in our population (although in a less significant proportion).3,10,11
Integrated management of AF includes assessment of thromboembolic risk in all patients in order to identify those who should be offered oral anticoagulation.12 In the light of recent studies on DOACs,1 these should be the preferential choice in AF patients. In our cohort, the majority of patients were eligible for long-term anticoagulation (median CHADS2-VaSC2 score of 2) and a high proportion were offered anticoagulation (92.49%), of which 98.34% were with DOACs.
According to the AF ablation consensus statement,4 the procedure should be undertaken with sedation or general anesthesia, and in patients under anticoagulation who are in AF at the time of the procedure or in sinus rhythm without previous anticoagulation, performing preprocedural TEE is reasonable. In our cohort, 30.93% of patients underwent the procedure under general anesthesia and the other procedures were performed with conscious sedation. Although in patients under anticoagulation exclusion of LA appendage thrombi with imaging is not mandatory, in our population the majority of patients underwent cardiac CT (81.49%) or TEE (38.81%) before the procedure in order to exclude thrombus and also for procedural planning, as these modalities provide assessment of LA anatomy.
The consensus document recommends that ablation should preferably be performed without interrupting anticoagulation (class I recommendation),4 but regarding this, in our population there was a low proportion of patients (7.36%) with this indication. In fact, most procedures were performed according to a IIa class recommendation, with anticoagulation interrupted for 24 h (34.97%) or more than 48 h (49.39%). This is a quality measure that is unmet and efforts should be made to improve it.13 On the other hand, although anticoagulation was interrupted, these procedures were performed safely with the use of UFH (administered either before or immediately after transseptal puncture) and the use of ACT to monitor anticoagulation levels, which had an adequate median of 310 s during the procedure. Most patients restarted oral anticoagulation at a median of 5 h post procedure, as recommended, and 99.10% were anticoagulated at discharge (99.39% with DOACs). Although these data reflect a tendency to delay adoption of recommendations to perform ablation without interrupting anticoagulation (probably due to fear of complications), there are no concerns regarding the attainment of appropriate anticoagulation levels during all stages of the periablation period or after the procedure and on discharge, in a period with a higher thromboembolic risk due to extensive ablation in the left atrium. Of greater concern, although their number is low, is the fact that three patients (0.89%) were not anticoagulated at discharge, as after ablation and in the first two months it is necessary to maintain anticoagulation in all patients irrespective of their CHADS2-VaSC2 score.
In our study, the use of 3D mapping systems was predominant (76.52% of procedures), mostly using Carto® and Ensite® (59.15% and 16.77%, respectively). Although radiofrequency energy was most often used (73.87%), there was increasing use of single-shot techniques using cryoenergy, which represented a fourth of all procedures.14 This probably reflects a growing preference for techniques that are faster and enable more procedures to be performed, at a time when patient referrals for AF ablation are on the increase.
The aim of AF ablation should always include PVI, and although demonstration of bidirectional block is desirable, the class I recommendation refers only to the demonstration of at least entry block,4,5,15 demonstration of exit block being a class IIb recommendation. Concomitantly, in patients with a history of typical atrial flutter or its induction during ablation, cavotricuspid isthmus ablation is recommended. There is also the possibility of performing linear ablation as well as PVI, with pacing maneuvers to confirm block being recommended. In our study PVI was the strategy adopted in 94.61% of patients. It is important to note that 16.84% of patients were referred for a redo procedure after previous AF ablation, which is probably why PVI was not the main strategy in all patients. There was a high rate (98.17%) of acute PVI success during the procedures but entry block was confirmed in only 85.77%. Additional ablation lines were performed in only 12.05% of patients and pacing maneuvers to confirm block of these lines were performed in 39 of the 40 patients for whom this strategy was used. There were also 51 patients with typical atrial flutter previously diagnosed or occurring during AF ablation and cavotricuspid isthmus ablation was performed in 84.3%. As recommended, in our cohort the power delivered in the LA posterior wall was lower in all RF procedures, with an esophageal thermometer being used in only two patients; this a reasonable (class IIB) recommendation to reduce risk during AF ablation.4
It is recommended that outcomes of AF ablation should be reported to ensure that the most appropriate strategies are being used for patient management.4,16-18 In our study, we identified acute complications during AF ablation in five (1.49%) patients, of which only one was major, requiring intervention (emergency cardiac surgery). At one month post AF ablation, there were two reported deaths (0.73%) and six (2.18%) procedure-related complications. On patient also had an embolic event (under full-dose anticoagulant therapy) and two patients had a bleeding event (both while on anticoagulant therapy). No additional adverse events had occurred at one year after the procedure. This rate of reported complications is in line with previously reports, which may be an indication that adhering to recommendations for AF ablation increases procedure safety.
It is also recommended that patient recovery level and outcomes after a rhythm control strategy with ablation should be reported, along with AF management in the post-ablation period.17 In our study, at the end of the first month there was significant symptomatic improvement in the majority of patients (200; 86.21%) although 12.5% reported no change from baseline symptoms and 1.29% reported worsening of symptoms. The recovery level was sustained with no significant difference at one year post ablation, with a median mEHRA score of 1, a significant improvement compared to baseline (pre-ablation mEHRA score of 3).
Regarding patient management after ablation, at one month, six months and one year post ablation, 77.94%, 70.83% and 62.5%, respectively, of patients were still on Vaughan Williams class I or III antiarrhythmic drugs, reflecting a reduction in the use of this therapy compared to the pre-ablation period (85.29%). This result reflects good adherence to the class IIa recommendation4 for the immediate and short-term use of antiarrhythmic drugs in the post-ablation period and in the medium and long term, a strong preference for a hybrid approach (AF ablation and continued antiarrhythmic therapy), which is also a possibility for the care of patients with AF within the recommendations for rhythm control in the roadmap consensus for improvement of AF patient management.5
With respect to anticoagulation, 99.64% of patients were under anticoagulation therapy at two months post ablation and 93.33% by the end of the first year, which also reflects adherence to quality measures of patient management after ablation, for which maintenance of anticoagulant therapy should be driven by individual thromboembolic risk and not by apparent success of AF ablation.4
Regarding AF relapse, we identified 12.6% of patients who relapsed in the first month post ablation during the blanking period (four patients underwent a redo procedure), and at one year there were relapses in 19 (26.39%) patients (three underwent redo procedures). These findings are in line with reports of AF relapse after ablation,1 and probably reflect the importance of centers following recommended strategies in the selection of patients for ablation and also adhering to recommended strategies during the periablation period. In our study, 30-day AF relapse was independently associated with previous LA ablation and was less likely if PVI was the strategy used for ablation. In the long term (one year post ablation), AF relapse appears to be associated with increased LA diameter, AF type, lack of improvement in mEHRA score and the existence of AF relapse at 30 days. These results are in line with previous AF ablation trials and recommendations, with less evidence of long-term efficacy of ablation in non-paroxysmal forms of AF ablation, and suggest that relapse during the blanking period may predict long-term AF recurrence.1,9,10
More than 80% (86.7%) adherence to 13 of the 15 class I recommendations for AF ablation in the 2017 HRA/EHRA/ECAS/APHRS/SOLACE international consensus document4 was reported in patients in our study, and our results thus reflect good adherence to the consensus regarding patient management and selection of patients for AF ablation. Likewise, with respect to quality indicators specifically for AF ablation procedures and post-ablation management, there is a good standard of practice with respect to procedure planning, performance and management of patients in the post-ablation period.
LimitationsOur study has limitations. First, this was not a mandatory registry, and participation in the survey increased the workload in participating centers. Consequently, although a significant proportion of hospitals responded to the survey, we do not have complete coverage throughout the country and there may be biases associated with differences between centers that did or did not respond to the survey. Second, as in all large-scale surveys, some data were missing, and additionally complete information was not mandatory, which could add bias to the reported results. In particular, one-year follow-up should be interpreted with caution due to the low number of patients for whom data are available, and further studies would be of great value to further address long-term follow-up. Also, the complications and deaths that occurred in the study period are not specified, and this is an important point that should be addressed in further studies.
ConclusionsIn a population of patients with AF referred for ablation in Portuguese centers, we can state that patient management is provided according to the best scientific evidence recommended by European guidelines and that there is a high standard of practice with respect to the quality of AF ablation, with safety measures and reported outcomes achieved as recommended.
Registry collaboratorsPedro Carmo, Hospital de St.ª Cruz, Centro Hospitalar de Lisboa Ocidental E.P.E., Carnaxide, Portugal and Hospital da Luz, Lisbon; Dinis Mesquita, Hospital de S. Bernardo, Centro Hospitalar de Setúbal E.P.E., Setúbal, Portugal; Luis Brandão, Hospital Garcia de Orta E.P.E.; Luis Adão, Centro Hospitalar Universitário de São João, E.P.E.; Nuno Cabanelas, Hospital Prof. Doutor Fernando Fonseca E.P.E., Amadora, Portugal; Pedro Silva Cunha, Hospital de Santa Marta, Centro Hospitalar Universitário de Lisboa Central, E.P.E.; Sofia Almeida, Hospital CUF Tejo.
FundingThis study was sponsored by Boehringer Ingelheim Portugal in the form of an educational grant.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank all the participating centers that collaborated in the registry and Boehringer Ingelheim for their sponsorship of this study.