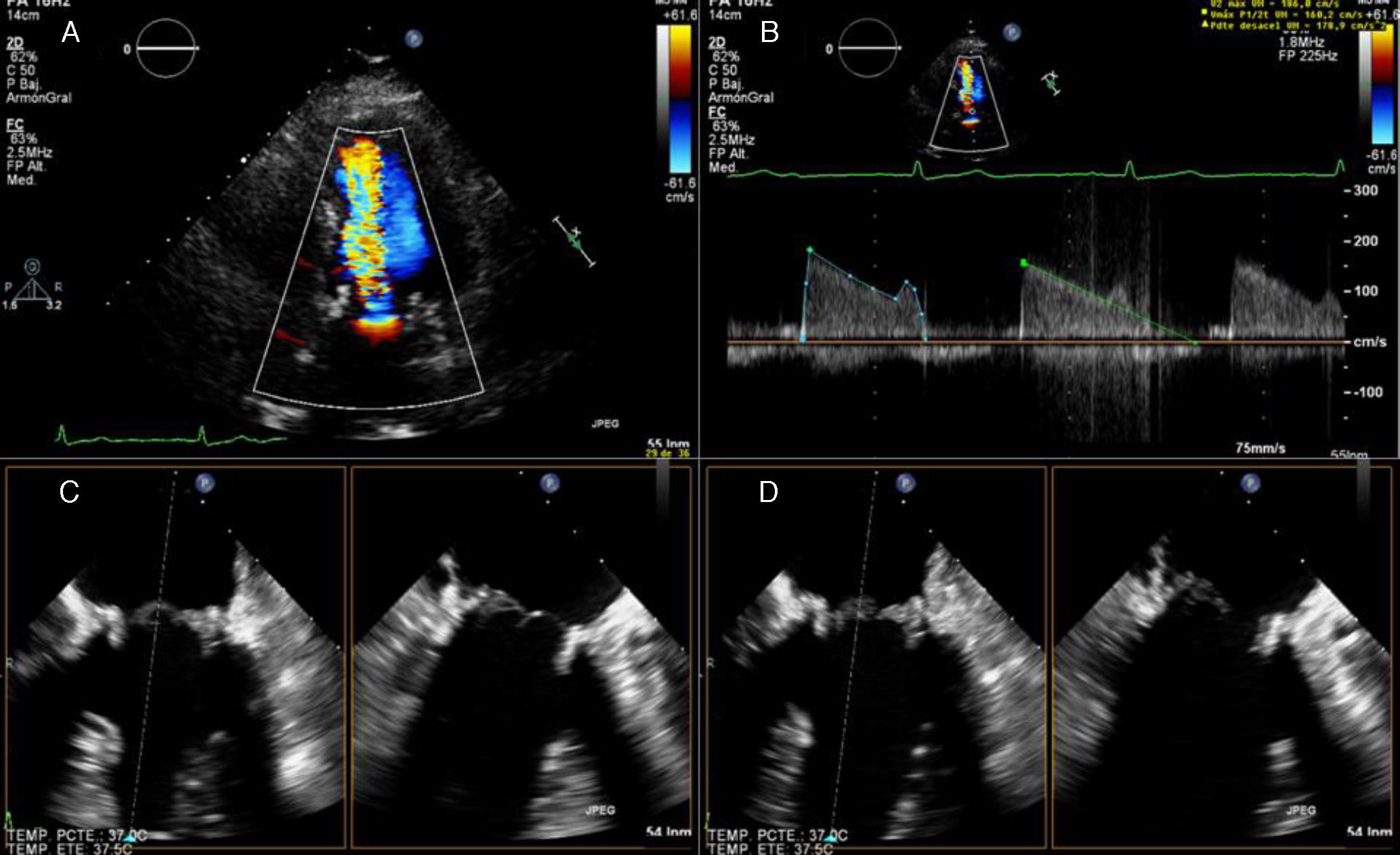
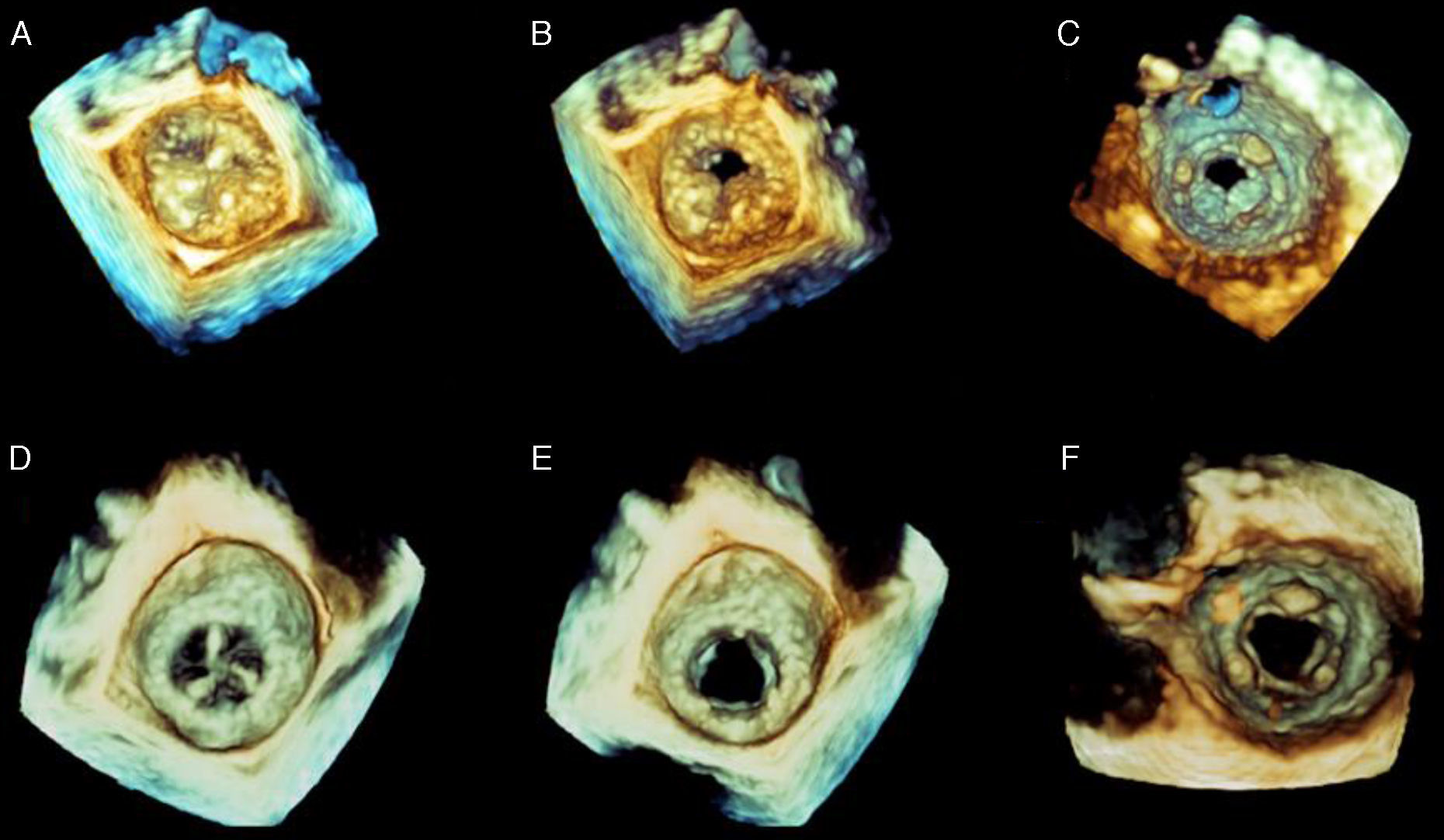
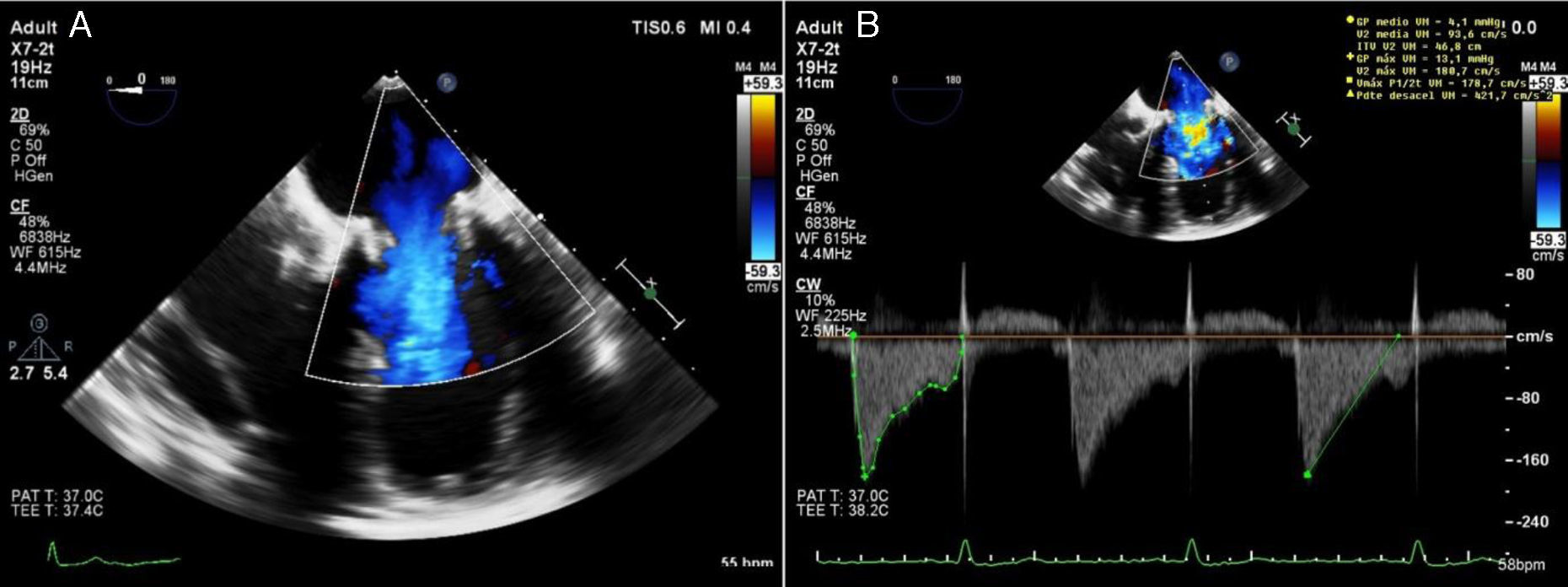
A 73-year-old woman presented to the emergency department with a two-month history of progressive dyspnea on exertion. Fifteen months earlier she had undergone mitral valve replacement with a bioprosthesis due to severe mitral regurgitation. Her postoperative treatment included antiplatelet therapy with aspirin and oral anticoagulation, but both medications were discontinued six months after the surgery. Transthoracic echocardiography showed prolongation of mitral pressure half-time suggestive of prosthesis dysfunction (Figure 1A and B, Video 1). Transesophageal echocardiography (TEE) revealed thickening of two of the three prosthetic mitral leaflets, with restricted mobility. The anterior leaflet opened normally, resulting in severe stenosis with a total effective area of 0.81 cm2 calculated by three-dimensional (3D) planimetry (Figure 1C and D, Figure 2A–C, Videos 2–4). Diuretics, aspirin and anticoagulation were initiated and the patient was discharged home on day 3 with a presumptive diagnosis of prosthetic valve thrombosis. Follow-up TEE performed two months later showed normal thickness of the three leaflets with normal opening and an effective area of 1.7 cm2 assessed by 3D echocardiography (Figure 2D–F, Figure 3, Videos 5 and 6). This case demonstrates the utility of 3D TEE to define the anatomy of the obstructed prosthesis and how the thrombus impairs leaflet function. In addition, it illustrates the potential benefit of maintaining antiplatelet therapy in patients with a bioprosthetic mitral valve and no other risk factors for thromboembolism, as recommended in the 2014 AHA/ACC guideline for the management of patients with valvular heart disease.
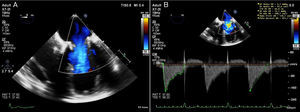
Transthoracic echocardiography demonstrating increased flow velocity across the mitral bioprosthesis (A), with prolongation of pressure half-time and elevated mean pressure gradient (B); two-dimensional transesophageal echocardiography showing marked thickening of two of the three mitral leaflets (C systolic frame, D diastolic frame).
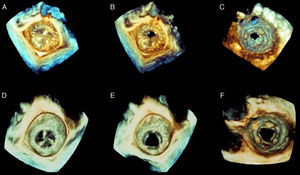
(A–C) Baseline three-dimensional transesophageal echocardiography (3D TEE) images of the prosthesis as viewed from the left atrium (A, systole; B, diastole) and the left ventricle (C, diastole); 3D TEE confirms two-dimensional findings and improves anatomical characterization of the thrombosed bioprosthesis; (D–F) control 3D TEE after two months of antithrombotic treatment demonstrating normal prosthetic function, with normal opening of the three leaflets.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.