Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia in the developed world and is associated with impaired quality of life, a five-fold higher risk of stroke, a three-fold increased incidence of heart failure, and a nearly two-fold higher risk of hospitalization and overall mortality.1 AF is known to be exponentially more prevalent among the elderly, but is frequently asymptomatic and therefore undiagnosed. This results in suboptimal rates of anticoagulation and effective control of other cardiovascular risk factors. The clinical and economic burden posed by AF is therefore substantial, and this scenario is set to worsen in the coming years,1 mainly driven by population aging2,3 and its association with various comorbidities.
In FAMA, a large-scale epidemiological study conducted in 2009 in Portugal, the prevalence of AF among individuals aged over 40 years was estimated to be 2.5%.3 The SAFIRA study estimated a 9.0% prevalence in patients aged over 65 years,4 as did another Portuguese study.5
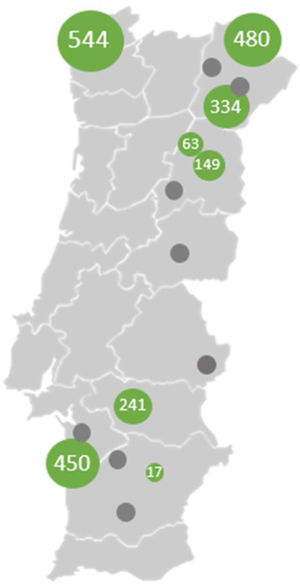
The Screening of Atrial Fibrillation among Elderly in Primary Care with MyDiagnoSTick (SAFEST) study uses a device (MyDiagnostick®, MyDiagnostick Medical B.V. Maastricht, The Netherlands) (Figure 1) for opportunistic screening of AF in an elderly population. SAFEST is a cross-sectional, multicenter registry conducted in 18 primary care units (PCUs) throughout Portugal. Currently, eight units have concluded recruitment, with 2278 participants included (Figure 2). The mean age is 74.90 years (standard deviation 7.40) and 57.12% are female.
Geographic distribution of recruitment. Primary care units that have concluded recruitment, in ascending order of number of participants (in green): UCSP (Unidade de Cuidados Saúde Personalizados) Beja, UCSP Trancoso, UCSP Celourico da Beira, USF Salus, UCSP Torre de Moncorvo, UCSP Sines, UCSP Bragança I – Sé, USF (Unidade de Saúde Familiar) Lethes. Study sites not yet activated (in gray): UCSP Mirandela II, UCSP Alfândega da Fé, UCSP Seia, USF Beira Saúde, UCSP Ferreira do Alentejo, UCSP Ourique, UCSP Alcácer do Sal, USF Uadiana.
The main goals are to determine the diagnostic yield of an opportunistic AF screening strategy with the device in the elderly population, as well as to assess the impact of a screening-based diagnosis on six-month anticoagulation adherence rate. Secondary objectives include creating risk factor profiles to guide screening strategies for detection of silent AF, exploring potential clinical and echocardiographic predictors, and assessing regional disparities. Patients without a previous diagnosis of AF, coming in for a general practice appointment, are invited to enter the study and, after informed consent is obtained, a non-invasive, one-minute diagnostic test with the MyDiagnostick is performed to screen for AF. For positive results, a 12-lead ECG is performed to confirm the AF diagnosis, and the exam is ultimately validated by a cardiologist.
To avoid burdening clinical practice at the included PCUs, a cardiac physiology technician is added to the team and allocated to whichever center is active. This person is responsible for collecting patient information on demographics, clinical history and current medication, and performs the test using the MyDiagnostick device and the 12-lead ECG if indicated.
Managing a multicenter study in a primary care setting is a massive challenge, as it involves multiple ethics committee submissions and approvals, complex logistics, and geographic dispersion. Additionally, communication with the study sites is demanding, as these units have no associated entities or professionals dedicated to clinical research. Once the study site is activated and the cardiac technician allocated, they become the main point of communication with each site.
Although this study model is replete with operational obstacles, it is of considerable value for collecting data from an under-represented population that is distant from large healthcare facilities. This also highlights the merits of involving PCUs in clinical research.
This study constitutes the first large-scale analysis of an opportunistic screening strategy for AF in elderly individuals in a primary care setting, focusing predominantly on rural areas, using a rhythm monitoring device.
We believe that this registry may have important implications for clinical practice in the future, contributing to the implementation of public health measures aimed at increasing the population's awareness of AF, leading to a reduction in the incidence of ischemic stroke in populations at risk through the early institution of anticoagulation when indicated, and attenuating regional asymmetries in the detection and management of this clinical condition.
Conflicts of interestThe authors have no conflicts of interest to declare.