With improvements in respiratory care, patients with Duchenne muscular dystrophy (DMD) are surviving longer, with cardiac morbidity becoming an increasingly common problem. Routine assessment of cardiac function is therefore of increasing importance in this group. We illustrate an unusual case in which marked herniation of the left hemidiaphragm prevented assessment of left ventricular (LV) function, even with the aid of contrast-enhanced echocardiography, highlighting the potential value of cardiac CT imaging in this patient group.
DMD is an X-linked cardiac and skeletal muscle disorder affecting approximately 1 in 6000 boys. The disease process begins in childhood and boys affected with DMD are typically wheelchair-bound before 12 years of age.1 Over 90% of patients with DMD present cardiac involvement with arrhythmias, hypertrophic or dilated cardiomyopathy by the age of 20, accounting for significant morbidity.2
Despite extensive cardiac involvement, initiation and up-titration of appropriate therapy has demonstrated prognostic value, and the routine and regular assessment of LV function is therefore of paramount importance. However, echocardiography is not always feasible due to the neuromuscular scoliosis affecting the body and chest wall positioning, and multimodality imaging may be useful in providing accurate cardiac assessment and guiding further management.3
A 32-year-old DMD patient with severe respiratory failure requiring continuous non-invasive ventilation and a background of diabetes mellitus and hypertension attended our multidisciplinary cardiorespiratory clinic for assessment. It was not possible to visualize any cardiac structures with 2D echocardiography and a contrast-enhanced study was arranged. Unfortunately, even with continuous infusion of microsphere contrast, it was not possible to adequately visualize the left ventricle. Appearances suggested possibly significantly reduced LV systolic function, but the study was deemed non-diagnostic.
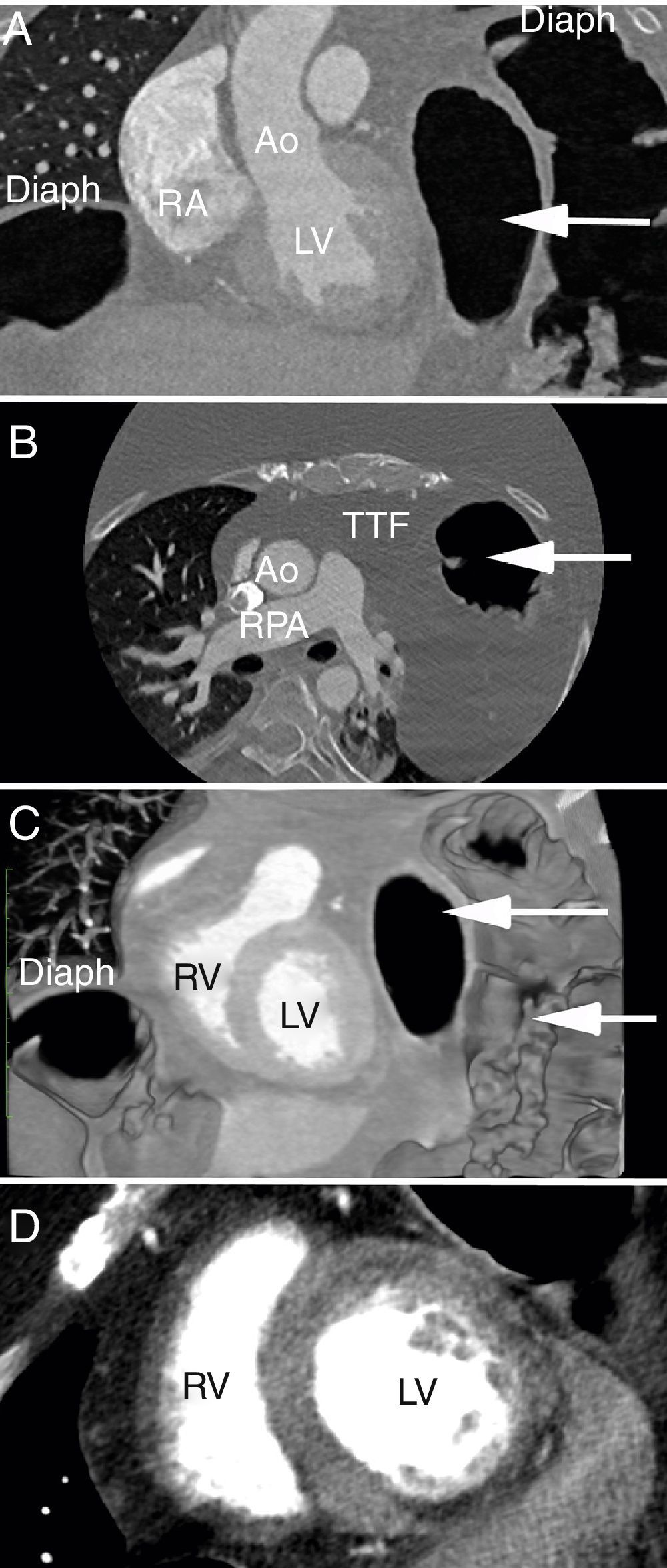
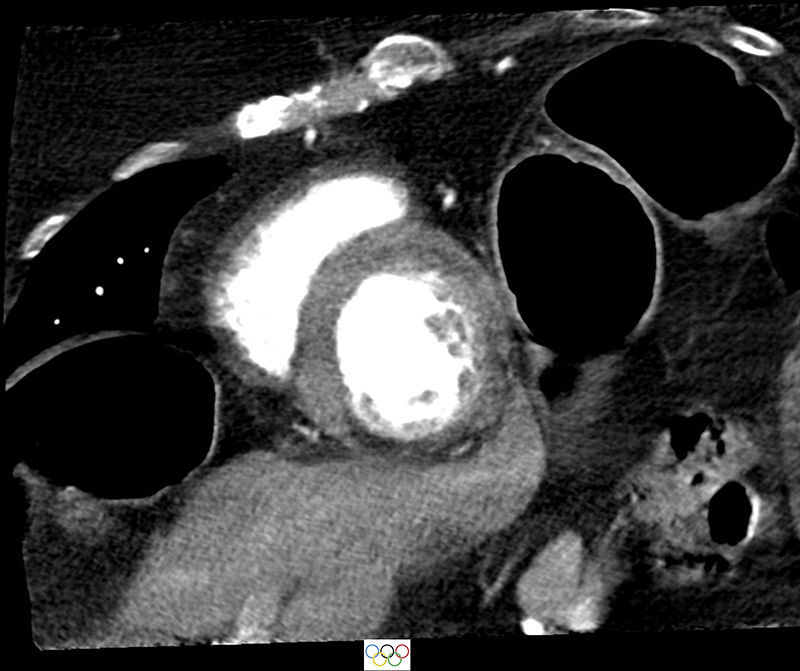
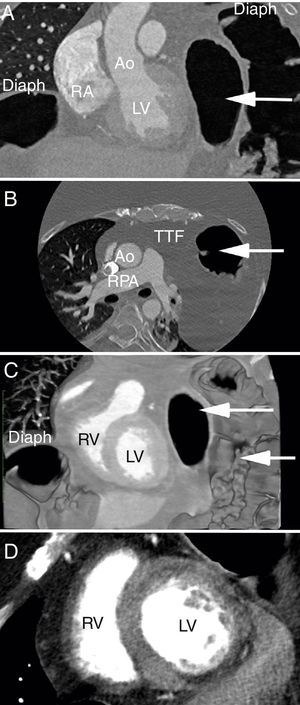
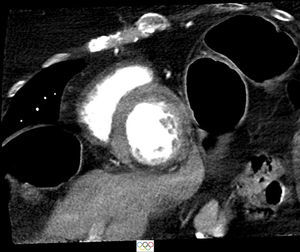
For further investigation, alternative imaging was sought. Cardiac magnetic resonance imaging was not feasible owing to body habitus, orthopnea and requirement for continuous non-invasive ventilation. Therefore, a retrospective ECG-gated cardiac computed tomography (CT) scan was performed for functional imaging. This showed mildly reduced LV systolic function with left ventricular ejection fraction of 47%, end-diastolic volume of 147 ml and end-systolic volume of 77 ml. The basal and mid inferior wall appeared thin and hypokinetic with a corresponding hypoperfusion pattern seen on first-pass perfusion imaging typical of Xp21 dystrophies (Figure 1).4 Note was also made of severe herniation of the abdominal contents into the left hemithorax (Figure 1), accounting for the non-diagnostic echocardiogram and contrast echocardiogram studies. The left lung was almost completely collapsed with a minimally aerated left lower lobe and a small amount of aerated left upper lobe as a result of marked elevation of the left hemidiaphragm. There was herniation of the stomach and small and large bowel as well as the tail of the pancreas into the left thoracic cavity. In short-axis view of the left ventricle, the herniated bowel loops gave the appearance of the Olympic rings (hitherto termed the “Kapetanakis-Rajani” sign) (Figure 2).
Cardiac computed tomography. (A) Coronal plane with marked herniation of the abdominal contents into the left hemithorax (white arrow); (B) the corresponding axial plane with bowel loops extending up into the thorax to the level of the main pulmonary artery; (C) coronal volume-rendered image of the bilateral diaphragmatic elevation and bowel loops within the thoracic cavity; (D) contrast-filled cardiac chambers with a thin and hypoperfused inferior wall, as typically seen in Duchenne muscular dystrophy. Ao: aorta; Diaph: diaphragm; LV: left ventricle; RA: right atrium; RPA: right pulmonary artery; RV: right ventricle; TTF: transthoracic fat.
The incidence of dilated cardiomyopathy in patients with DMD has been reported as 25% by six years of age and up to 60% by 10 years of age. For these patients, echocardiography with or without the use of contrast agents remains the mainstay of cardiac assessment. This technique however is susceptible to suboptimal image quality as a consequence of body habitus, structural diaphragmatic changes and resultant abdominal herniation into the thoracic cavity. In such instances alternative imaging techniques such as multiple gated acquisition scanning and cardiac magnetic resonance imaging have been proposed.
In the case presented, we firstly show an advanced case of DMD in which significant diaphragmatic paralysis and resultant abdominal visceral herniation restricted the use of echocardiography. Secondly we show the clinical utility of gated cardiac computed tomography to assess cardiac size, function and perfusion when other techniques were not possible.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.