Aortic stenosis is the most common valvular heart disease. The number of octogenarians proposed for intervention is growing due to increased lifespan. In this manuscript we aim to evaluate perioperative outcome and long-term survival after surgical aortic valve replacement (SAVR) in octogenarians, comparing patients with low surgical risk (EuroscoreII <4%) with intermediate-high risk (EuroscoreII ≥4%).
MethodsA retrospective observational single-center cohort study with 195 patients aged ≥80 years old, who underwent SAVR between 2017 and 2021, was conducted. Patients were divided into two groups according to EuroscoreII: (1) Low risk (EuroscoreII <4%) with intermediate-high risk (EuroscoreII ≥4%). Continuous variables are presented in median (IQR), analyzed using Wilcoxon rank sum test; categorical variables in percentages, analyzed using chi-squared test; and survival was analyzed by Kaplan–Meier, open cohort, and the log-rank test was performed.
ResultsThe overall median age was 82 (IQR 81–83), with 4.6% of the patients ≥85 years old. 23.6% of the patients presented EuroscoreII ≥4%. No complications were observed in 26.2%, with a significantly higher rate in intermediate-high risk patients. Postoperative need for hemodynamic support was the most frequent complication, followed by postoperative acute kidney injury and the use of blood products. Overall median ICU stay was three days (2–4) and hospital length of stay (LOS) six days (5–8). Patients with intermediate-high risk and those with complications had longer ICU LOS. At 12 months, overall survival was 96.4%, at three years 94.1% and 5 years 75.4%. Patients with low surgical risk had higher survival proportions up to 5 years.
ConclusionSAVR in patients ≥80 years is associated with low in-hospital mortality, although a significant proportion of patients develop complications. Long-term follow-up up to five years after surgery is acceptable in octogenarians with low surgical risk.
A estenose aórtica é a doença valvular mais frequente. O número de octogenários propostos para intervenção está a aumentar devido ao aumento da esperança média de vida. Neste artigo pretendemos avaliar os resultados cirúrgicos e sobrevida a longo prazo da cirurgia de substituição de válvula aórtica (SVA) em octogenários, comparando pacientes com baixo risco cirúrgico (EuroscoreII <4%) com risco intermédio-alto (EuroscoreII ≥4%).
MétodosEstudo observacional retrospetivo, centro único, incluindo 195 doentes ≥80 anos, submetidos a SVA entre 2017-2021. Os pacientes foram divididos em dois grupos de acordo com EuroscoreII: baixo risco cirúrgico (EuroscoreII <4%) ou risco intermédio-alto (EuroscoreII ≥4%). Variáveis contínua; variáveis categóricas em percentagens, analisadas com teste chi-quadrado. A sobrevivência foi analisada com modelo de Kaplan-Meier, coorte aberto, usando o teste log-rank.
ResultadosA mediana de idades foi de 82 (IQR 81-83), com 4,6% dos doentes ≥85 anos; 23,6% apresentavam EuroscoreII ≥4%; 26,2% dos doentes não apresentaram complicações, com uma proporção mais alta de complicações nos doentes com risco intermédio-alto. A complicação mais frequente foi a necessidade de suporte hemodinâmico pós-operatório, seguida de lesão renal aguda e de transfusão de produtos hemáticos. O tempo mediano de internamento na UCI foi de três dias (2-4) e hospitalar de seis dias (5-8). Doentes com risco intermédio-alto e com complicações apresentaram internamentos na UCI mais prolongados. A sobrevida global foi de 96,4% aos 12 meses, 94,1% aos três anos e 75,4% aos cinco anos.
ConclusãoA SVA em doentes ≥80 anos apresenta mortalidade intra-hospitalar baixa, apesar de uma proporção significativa de pacientes desenvolver complicações. A sobrevida é mais elevada após cinco anos nos pacientes com baixo risco.
.
Aortic valve stenosis (AS) is the most common heart valve disease in developed countries,1 with an estimated prevalence of around 3% in patients aged 65 years or more, but gradually increases with age, reaching 4.3% between 76 and 85 years and 7.4% over 85.2
Mortality significantly increases with the onset of symptoms, with approximately a 50% risk of death in the first two years.3,4 Besides the higher risk of death, patients also present a considerably impaired quality of life.5 Prognosis can be modified with an aortic valve intervention, such as surgical aortic valve replacement (SAVR) or transcatheter aortic valve implantation (TAVI). Subsequently, more than 65000 and 67500 AVR are performed each year in Europe and the United States of America, respectively.6 Although AS already represents a considerable burden that requires intervention, the number of patients with AS will increase in the next decades due to an aging population.7,8 Moreover, both the proportion and absolute number of older patients being offered interventions will increase.
Elderly patients have a higher incidence of comorbidities and have been classically associated with a substantial increase in morbidity and mortality, with up to 78% of major complications and death after cardiac surgery occurring in patients over 75 years.9 Yet, improvements in patient selection, extracorporeal circulation, perioperative management and surgical techniques have significantly reduced morbidity and mortality over the past years, enabling safe aortic valve interventions in older patients. Mortality in octogenarians was reported to be as high as 24% in 1988, decreasing to 15.7% in 1991 and approaching 4% in 2015.10–12
In 2021, life expectancy in Portugal at the age of 65 was 19.6 years (17.8 years for males and 21 for females), and in the same year, approximately 23.8% of the Portuguese population were aged 65 or over.13 The percentage of elderly patients in Portugal will increase in the next decades, and the number of octogenarians being offered interventions will probably also rise, as predicted in other developed countries.11,12
ObjectivesThe aim of this study was to assess the safety of SAVR in octogenarians, evaluating perioperative outcomes and in-hospital and long-term mortality, comparing patients with low surgical risk (EuroscoreII <4%) with patients with intermediate and high risk (EurosoreII ≥4%).
MethodsStudy populationThis is a retrospective single-center study, including 195 consecutive patients aged 80 years or more, who underwent surgery at the Cardiothoracic Surgery Department at Hospital de Santa Maria, Lisbon, Portugal, between January 2017 and January 2021. We included only patients who underwent isolated SAVR, excluding patients with (1) previous cardiac surgery; (2) active endocarditis; (3) combined procedures, and (4) missing clinical data on the electronic process (Figure 1). Patients who are aged over 80 are discussed by the heart team for an optimal intervention decision. Low surgical risk patients are usually referred to surgery, while patients at intermediate and high surgical risk are referred to surgery only when they are not suitable for a percutaneous interventional due to anatomical or clinical features.
Patients were divided into two groups according to preoperative EuroscoreII risk score: (1) low surgical risk (EuroscoreII <4%), n=149 and (2) intermediate and high surgical risk (EuroscoreII ≥4%) n=46.
The study was approved by the local Ethics Committee (Comissão Ética Centro Hospitalar Lisboa Norte – Ref. No, 23/18), and the need for a signed informed consent form from patients was waived due to the retrospective and anonymous nature of the data. The study followed the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” guidelines.
Surgical procedure and data collectionWe performed SAVR as previously reported by our group.14 Total intravenous anesthesia was used, maintained with propofol during cardiopulmonary bypass (CPB). CPB circuit included Inspire 6® (Sorin Group, Italy) or Quadrox-i® (Getinge, Sweden) oxygenators, without mannitol or corticoids in the priming solution. Heparin (300 mg/kg) was administered to achieve an activated clotting time superior to 480 seconds. A non-pulsatile roller pump was used with blood flow indexed to 2.4 L/min/m2. Surgery was performed with normothermia, with standard aortic cross-clamp, central cannulation in the ascending aorta and central venous cannulation in the right atrium. Intermittent antegrade cold blood cardioplegia was used for cardioplegic arrest induction, and reperfusion warm blood hot-shot solution was administered before aortic cross-clamp release.
Demographics, clinical characteristics and perioperative data were collected electronically from the clinical files from our department and from registries from the national electronic healthcare database.
Statistical analysisContinuous variables are presented as median with interquartile range (IQR) and were analyzed using Wilcoxon rank sum test for non-paired samples. Categorical varia- bles are presented in frequencies or percentages and were analyzed using chi-squared test. All reported p-values are two-sided tests, considering a significance level of 5%. We have considered ns as non-significant, *:P<0.05; **:P<0.01; ***:P<0.001; and ***:P<0.0001.
Survival curves were drawn using the Kaplan-Meier method and analyzed by the log-rank test. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) (New York, USA) and GraphPad Prism 9 (Boston, USA).
ResultsPatientsBaseline characteristics are detailed in Table 1. Median EuroscoreII was 2.69 (1.76–3.8), with 76.4% (149 patients) presenting low surgical risk with EuroscoreII lower than 4% and 23.6% (46 patients) of the patients presenting an EuroscoreII of 4% or higher (intermediate-high risk). Patients’ mean age was 82±1.94, with 63.6% (124 patients) between 80 and 82, 31.8% (62 patients) between 83 and 85 and 4.6% (9 patients) over 85 years old. Patients at a low surgical risk were statistically significantly younger. Considering all patients, nearly half (50.8%) were male, and hypertension was the most common comorbidity (94.4%). A significant proportion of dyslipidemia (71.8%), diabetes mellitus (28.7%), chronic kidney disease (49.2%) and ischemic cardiopathy (23.6%) was also present. The majority (62.6%) presented preserved left ventricular (LV) function, with 34.9% presenting moderate LV function and 2.5% poor LV function. Patients with intermediate-high risk had higher proportion of risk factors for cardiac surgery, as female sex, peripheral vascular disease, chronic lung disease and left ventricle dysfunction (Table 1). Almost all patients were symptomatic, according to the New York Heart Association (NYHA) functional classification, with only 1% in NYHA Class I. Low-risk patients had a higher proportion of NYHA Class I and II patients. The procedure was performed electively in 163 patients (83.6%) and urgently in the other 32 patients (16.4%), in all patients. The proportion of patients who required urgent surgery was significantly higher in the intermediate-high risk patients.
Demographic data.
| Variable | All patients | Low risk | Intermediate-high risk | p-Value |
|---|---|---|---|---|
| n | 195 (%) | 149 (%) | 46 (%) | |
| Age, years, mean±SD | 82±1.9 | 82±1.8 | 82.9±2.3 | 0.01* |
| Male sex | 99 (50.8) | 82 (55) | 17 (37) | 0.04* |
| BMI, kg/m2, mean±SD | 27.3±3.9 | 27.3±4.1 | 27.4±3.2 | 0.95 |
| Hypertension | 184 (94.4) | 138 (92.6) | 46 (100) | 0.07 |
| Diabetes mellitus | 56 (28.7) | 42 (29.2) | 14 (30.4) | 0.85 |
| Dyslipidemia | 140 (71.8) | 110 (73.8) | 30 (65.2) | 0.27 |
| Chronic kidney disease | 96 (49.2) | 77 (51.7) | 19 (41.3) | 0.24 |
| Peripheral vascular disease | 17 (8.7) | 7 (4.7) | 10 (21.7) | 0.001** |
| Cerebrovascular disease | 18 (9.2) | 16 (10.7) | 2 (4.4) | 0.25 |
| Chronic lung disease | 25 (12.8) | 14 (9.4) | 11 (23.9) | 0.02* |
| Ischemic cardiopathy | 46 (23.6) | 32 (21.5) | 14 (30.4) | 0.24 |
| Atrial fibrillation | 29 (19.5) | 17 (37) | 0.02* | |
| LV function | ||||
| Preserved | 122 (62.6) | 101 (67.8) | 21 (31.8) | <0.0001**** |
| Moderate 31–50 | 68 (34.9) | 47 (31.5) | 23 (50) | 0.03* |
| Poor LV function (21–30%) | 5 (2.5) | 1 (0.7) | 2 (4.4) | 0.14 |
| Very poor LV function (<20%) | 0 (0) | 0 (0) | 0 (0) | |
| NYHA | ||||
| I | 2 (1) | 2 (1.3) | 0 (0) | >0.99 |
| II | 92 (47.2) | 78 (52.4) | 14 (30.4) | 0.01* |
| III | 98 (50.3) | 69 (46.3) | 29 (63) | 0.06 |
| IV | 3 (1.5) | 0 (0) | 3 (6.5) | 0.01* |
| Timing | ||||
| Elective | 163 (83.6) | 136 (91.3) | 27 (58.7) | **** |
| Urgent | 32 (16.4) | 13 (8.7) | 19 (41.3) | <0.0001 |
| EuroscoreII (IQR) | 2.7 (1.8–3.8) | 2.4 (1.7–2.8) | 5.2 (4.5–6.4) | <0.0001**** |
BMI: body mass index; IQR: interquartile range; LV: left ventricular; standard deviation. NYHA: New York Heart Association Functional Classification; SD: standard deviation. Ns: non-significant; *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
All patients underwent surgery with a diagnosis of severe aortic stenosis, and all received a bioprosthetic valve (Table 2). Up to 17% of the patients had a concomitant procedure, including morrow myectomy (13.8%), left atrial appendage resection (LAAR) (3.1%) or both combined (1%). Morrow myectomy was more frequent in the low-risk group, while LAAR was more frequent in the intermediate-high risk patients. Rapid deployment valves were used in 69.7% of the patients, which significantly contributed to the overall reduced CPB and aortic cross-clamp times of 39 min (IQR 32–58) and 29 min (23–48), respectively. Curiously, rapid deployment valves were used more frequently in the low surgical risk group, which explains the significantly lower CPB and aortic cross-clamp times (Table 2).
Surgical details.
| Variable | All patients | Low risk | Intermediate-high risk | p-Value |
|---|---|---|---|---|
| N | 195 (%) | 149 (%) | 46 (%) | |
| Aortic stenosis | 195 (100) | 149 (100) | 46 (100) | – |
| Surgery | ||||
| AVR | 160 (82.1) | 121 (81.2) | 39 (84.8) | 0.58 |
| AVR+morrow myectomy | 27 (13.8) | 25 (16.8) | 2 (4.3) | 0.03* |
| AVR+LAAR | 6 (3.1) | 2 (1.3) | 4 (8.7) | 0.009** |
| AVR+morrow myectomy+LAAR | 2 (1) | 1 (0.7) | 1 (2.2) | 0.36 |
| Prosthesis | ||||
| Edwards Perimout Magna Ease® | 41 (21) | 27 (18.1) | 14 (30.4) | 0.18 |
| Sorin Crown® | 6 (3.1) | 3 (2) | 3 (6.5) | 0.11 |
| Abbot Trifecta GT® | 12 (6.2) | 8 (5.4) | 4 (8.7) | 0.37 |
| Edwards IntuityElite® | 62 (31.8) | 46 (30.9) | 16 (34.8) | 0.62 |
| LivaNova Perceval/Perceval Plus® | 74 (37.9) | 65 (43.6) | 9 (19.6) | 0.003** |
| Prosthesis size | ||||
| S, 19, 21 | 69 (35.4) | 48 (32.2) | 21 (45.7) | 0.09 |
| M, 23 | 67 (34.3) | 52 (35.9) | 15 (32.6) | 0.77 |
| L, 25 | 39 (20) | 32 (21.5) | 7 (15.2) | 0.84 |
| XL, 27 | 20 (10.3) | 17 (11.4) | 3 (6.5) | 0.38 |
| CPB time, min; median (IQR) | 39 (32–58) | 37 (31–57) | 50 (37–71.5) | 0.002** |
| Aortic cross-clamp time, min; median (IQR) | 29 (23–48) | 27 (22–45.5) | 36 (27–56.5) | 0.002** |
AVR: aortic valve replacement; CPB: cardiopulmonary bypass time; LAAR: left atrial appendage resection. Ns: non-significant; *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
Postoperative complications are described in Table 3. Considering all patients, nearly a quarter of the patients (26.2%) had an uneventful postoperative course, without any complication. The rate of complications was significantly higher in patients with intermediate-high surgical risk, with only 6% presenting without any postoperative adverse event (compared to 30.2% in low-risk group, *p=0.02). The most common complication in both groups was the need for hemodynamic (vasopressor/inotropic) support (at least 6 h after surgery), which occurred in 54.4% and 73.9% (*p=0.03) of the patients with low and intermediate-high risk, respectively. Median mechanical ventilation time was 8 h (IQR 6–10) in all patients, with 82% of the patients being weaned in the first 12 h after surgery. No significant differences were observed between both groups. Most patients did not present significant postoperative bleeding (68.2%), with a median 400 mL (IQR 300–600). Only one patient in each group was re-examined due to severe postoperative bleeding and 39% of all patients received at least one blood product transfusion.
Postoperative complications.
| Mechanical ventilation, h, median (IQR) | 8 (6–10) | 8 (6–9.8) | 7 (6–11) | 0.29 |
| <6 h | 45 (23) | 34 (22.8) | 8 (17.4) | 0.54 |
| 6–12 h | 115 (59) | 90 (60.4) | 25 (54.3) | 0.49 |
| 12–18 h | 26 (13.3) | 19 (12.8) | 6 (13) | >0.99 |
| >18 h | 9 (4.7) | 6 (4) | 4 (8.7) | 0.25 |
| Postoperative bleeding (first 24 h), mL, median (IQR) | 400 (300–600) | 400 (300–700) | 400 (300–525) | 0.11 |
| Group 0 <600 mL | 133 (68.2) | 98 (65.8) | 35 (76.1) | 0.21 |
| Group I 601–800 mL | 34 (17.4) | 29 (19.5) | 5 (10.9) | 0.27 |
| Group II 801–1000 mL | 7 (3.6) | 5 (3.4) | 2 (4.3) | 0.67 |
| Group III 1001–2000 mL | 20 (10.3) | 16 (10.7) | 4 (8.7) | 0.79 |
| Group IV >2000 mL | 1 (0.5) | 1 (0.7 | 0 (0) | >0.99 |
| Re-exploration due to bleeding | 2 (1) | 1 (0.7) | 1 (2.2) | 0.42 |
| Use of blood products transfusions | 76 (39) | 55 (36.9) | 21 (45.7) | 0.30 |
| AKI | 96 (47.7) | 60 (40.3) | 29 (63) | 0.01* |
| Renal replacement therapy | 3 (1.5) | 1 (0.7) | 2 (4.3) | 0.14 |
| Delirium | 14 (7.2) | 10 (6.7) | 4 (8.7) | 0.74 |
| Implantation of permanent PMK | 15 (7.7) | 13 (8.7) | 2 (4.3) | 0.33 |
| De novo AF | 28 (14.4) | 25 (16.8) | 7 (15.2) | >0.99 |
| Infection | 18 (9.2) | 10 (6.7) | 6 (13) | 0.22 |
| Stroke | 1 (0.5) | 1 (0.7) | 0 (0) | >0.99 |
| Death | 1 (0.5) | 1 (0.7) | 0 (0) | >0.99 |
| ICU LOS, days, median (IQR) | 3 (2–4) | 3 (2–4) | 3.5 (2–5) | 0.02* |
| Hospital LOS, days, median (IQR) | 6 (5–8) | 6 (5–8) | 7 (5–11.3) | 0.11 |
AF: atrial fibrillation; AKI: acute kidney injury; ICU: intensive care unit; IQR: interquartile range; LOS: length of stay; PMK: pacemaker. Ns: non-significant; *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
Acute kidney injury (AKI) was the second most common complication, affecting 47.7% of the patients, although only 1.5% required renal replacement therapy and all patients completely recovered during hospital stay. The proportion of patients with AKI was higher in the intermediate-high risk group (*p=0.01), although the need for renal replacement therapy was similar between both groups. Other complications included delirium (7.2%), implantation of permanent pacemaker (7.7%), de novo atrial fibrillation (14.4%), infection (9.2%) and stroke (1%), all without significant differences between both groups. In-hospital death occurred in one patient (0.5%).
Overall, median intensive care unit (ICU) length of stay (LOS) was three days (IQR 2–4) and hospital LOS was six days (IQR 5–8). Patients at higher surgical risk had an increased ICU LOS (*p=0.02), although no statistically significant differences were observed in-hospital LOS (Table 3). Considering all the patients included in this study, a considerable proportion of patients (44.1%) were discharged from the ICU in the first 48 h after surgery, with 35.4% being discharged between the third and fourth postoperative days and only 20.5% had an ICU LOS of 4 or more days. Hospital LOS was inferior to eight days in 67.4% of the patients.
However, we observed a statistically significant difference between patients with and without postoperative complications. Patients with any postoperative complication had an increased ICU LOS [3 days (IQR 2–5) vs 1 day (IQR 1–2), ****p<0.0001] and hospital LOS [7 days (IQR 6–9) vs 5 days (IQR 5–7), ***p=0.0002].
SurvivalIn-hospital mortality rate was 0.5% (1 patient). Death occurred in an 81 year old male with no significant preoperative comorbidities, who developed unexpected refractory postoperative cardiogenic shock.
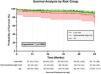
Overall survival at 12 months was 96.4% (Figure 2). Survival rates were 95.3% at two years, 94.1% at three years, 93.4% at four years and 75.4% at five years. None of the patients were re-operated, neither were referred to our department due to prosthetic valve dysfunction or significant periprosthetic leak.
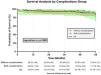
Patients at low surgical risk had slightly higher survival proportions up to 60 months (Figure 2), with a survival of 81.7% compared to 57.3% in the intermediate-high risk group (**p=0.0024). Considering that our group has previously showed that postoperative organ dysfunction in the ICU is associated with higher mortality rates after 12 and 24 months,15 we analyzed survival according to the occurrence of complications (Figure 3). The survival proportion for patients without postoperative complications was similar to those who experience any complication (ns, p=0.5992).
DiscussionOur study shows that SAVR in octogenarians is associated with low mortality rate, with satisfactory perioperative morbidity and in-hospital mortality. Moreover, patients with low surgical risk have very acceptable five-year survival rates, similar to what is expected in general population.13 Surgery in octogenarians is associated with a considerable proportion of postoperative complications, which were significantly higher in patients with intermediate-high surgical risk.
Age is an important and established predictor of perioperative morbidity and mortality in cardiac surgery. It is one of the greatest contributors to postoperative mortality, at the level of urgent or emergent presentation.16 The risk increases with age, and Hannan et al. have demonstrated that the adjusted hazard ratio for 30-month survival in patients with aortic stenosis undergoing SAVR increases from 1.57 in 65–74 years to 3.96 in patients over 84 years.17 It is well known that the strong and clear association between age and surgical outcomes has a considerable impact on the decision to operate. In fact, age is one of the main reasons to decide against surgery and was one of the preponderant factors to deny intervention in 33% of elderly patients with severe symptomatic aortic stenosis in the Euro Heart Survey.18
However, even in elderly patients with severe symptomatic aortic stenosis, the negative impact of conservative treatment remains unacceptable. It has been shown that SAVR confers significant survival benefits in patients aged 80 and over, with patients denied surgery having up to 12-fold increased mortality risk.19 Thus, the decision to operate should not rely solely on preoperative risk estimation and should consider the risk-benefit ratio, potential improvement in quality of life, current life expectancy and patient decision. Thereby, current recommendations for SAVR in octogenarians should consider the available data for three factors we will explore further: (1) recent improvements in cardiac surgery that lead to low morbidity and mortality rates; (2) postoperative improvement in quality of life; and (3) cost-effectiveness.
First, recent advances in cardiac surgery have substantially reduced perioperative morbidity and mortality in all patients. Despite the increase in patient risk profile and comorbidities, mortality in cardiac surgery has been consistently reduced,20,21 enabling older patients to undergo surgery with acceptable risk. Mortality rates after SAVR in octogenarians are now low, ranging from 1.9% to 4.5%.22–25
Second, while survival is clearly important to measure the success of surgery, it may not be the major factor in clinical decision to operate older patients, since improvements in quality of life can be much more impactful. Current evidence shows that surgery in elderly patients clearly reduces cardiac symptoms, equals or increases quality of life (compared to age-matched general population and to younger patients submitted to SAVR) and significantly increases patients’ functional status.26 Quality of life in the elderly can be assessed by diverse questionnaires, with the Short-form 36 Health Status questionnaire (SF-36) being the most frequently used.27 It includes 36 health-related multiple-choice questions covering eight domains (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health) to measure both physical and mental components. Using the SF-36, Bento et al. reported significant improvements in all domains at three, six and 12 months after SAVR in 163 octogenarians in Portugal, identical to other reports in several other developed countries.24,28,29
Finally, even from an economic perspective, SAVR has advantages in octogenarians. One way to evaluate the economic impact of an intervention is the cost-effectiveness ratio (CER), which provides the cost for gaining one additional quality-adjusted life year (QALY). It is commonly used to compare treatments and/or interventions. Wu et al. reported that the overall CER for a SAVR is $13528 per QALY and increases with age, up to $19826 in octogenarians.30 Commonly accepted thresholds establish less than $20000 per QALY as very cost-effective,31 so SAVR is very cost-effective in all patients, including patients aged between 80 and 89 years old.30 Moreover, Wu et al. have also shown that the return on the investment for SAVR is enormous for patients of all ages, even in very elderly patients.30,32
Currently, it is essential to consider TAVI when analyzing surgical results in this particular population. The NOTION trial, the only low-risk randomized controlled trial involving an elderly population, did not reveal a statistically significant difference between TAVI and SAVR concerning the composite endpoint of death, stroke, or myocardial infarction.33 Subgroup analyses of elderly patients in two major low-risk randomized controlled trials did not demonstrate statistically significant differences compared to the overall population. In the analysis of the PARTNER-3 trial,34 which compared TAVI using a balloon-expandable bioprosthesis (Sapien 3) with SAVR at five years, there was no significant difference in the risk of death, stroke, or rehospitalizations. Although mortality curves crossed beyond three years, the difference in all-cause mortality was not statistically significant, with a higher incidence of non-cardiovascular deaths in the TAVI group. The Evolut Low-Risk trial illustrated TAVI's noninferiority to surgery at the four-year mark.35 Generally, lower evidence studies support these findings.
In October 2023, Thourani et al. presented the initial report linking the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database to the National Death Index (NDI).36 The long-term mortality of 42586 low-risk patients undergoing isolated SAVR is detailed. The patients had baseline characteristics similar to those in both the Evolut and PARTNER-3 low-risk trials. In the analysis of the subgroup aged 75–84 years, mortality at one, three, five, and eight years was 2.5%, 4.3%, 6.7%, and 12%, respectively, with survival rates of 97.5%, 95.7%, 93.3%, and 88%, respectively.34 These remarkable results, frankly better than those published in well-known trials, should establish a new gold standard for SAVR, underscoring the excellence in care provided through these well-established surgical procedures.
Overall, the data support TAVI as a meaningful alternative for low-risk patients with severe aortic stenosis. However, careful consideration of individual patient factors and longer-term outcomes is paramount. There is insufficient evidence to prioritize older age as the exclusive criterion for choosing between TAVI and SAVR in otherwise low-risk patients. The superiority of either technique in this specific subgroup remains uncertain, with each method presenting its advantages and drawbacks. Given the limited four- to five-year follow-up in the two largest low-risk trials, decisions should be guided by life expectancy rather than age. Considerations of risk scores and procedural risks, which may or may not be associated with age itself, play a critical role in the decision-making process. This perspective underscores the significance of heart team discussions in selecting the most appropriate approach for each patient.
Our results show that elderly patients can undergo surgery with low mortality rates and acceptable morbidity rates. The in-hospital mortality rate was low (0.5%), similar to that observed in younger patients. Long-term survival was similar to that expected in patients in this range, and similar to other studies with slightly younger populations, such as in the PARTNER-3 sub analysis. Although PARTNER-3 showed survival rates of 93.3% at five years in patients between 75 and 84 years, our group of low surgical risk patients were significantly older and presented a survival rate of 81.7% at five years. One important consideration in the survival analysis between low and intermediate-high risk groups is that there are no differences in the confidence intervals (CI) between both groups, with an important overlap of both CI. One may conclude that with 95% of confidence there are no differences up to 60 months. One possibility to explain the statistically significant difference at 60 months between the two groups is the unbalanced proportion of patients (149 vs. 46 patients). Moreover, patients at an intermediate-high surgical risk have more comorbidities that may significantly impact long-term survival. In terms of morbidity, our patients had a significantly high rate of AKI (47.7%), although the majority had a mild postoperative AKI with complete in-hospital recovery and only 1.5% had necessity of renal replacement therapy. Other complications had similar or lower rates compared to what is currently published.12,19,24 Although the occurrence of complications may not directly impact survival, since there were no survival differences comparing patients with and without any complication up to five years after surgery, patients with higher preoperative risk had a significantly increased proportion of complications. The impact of postoperative complications in this subset of patients warrants further investigation.
We have no doubt that the number of older patients undergoing cardiac surgery will increase in the following years and this type of retrospective analysis is the starting point to design more accurate programs to continue reducing postoperative morbidity in older patients. New surgical approaches, with minimally invasive surgeries and/or the use of rapid deployment valves, will certainly contribute to new surgical strategies in this specific but absolutely substantial surgical population.
It is important to highlight that our study has several limitations, many of them associated with the retrospective nature of its design. It is a single-center analysis and the results may not be translated to other populations. Moreover, patients who underwent surgery are discussed in the heart team, but are pre-operatively evaluated by our Department, evaluating comorbidities and frailty. Thereby, there is a selection bias and only patients fit for surgery and with good functional status were included. Other patients with indication for intervention are referred for percutaneous aortic valve replacement.
ConclusionSAVR in octogenarians is associated with low in-hospital mortality, with a considerable proportion of patients developing postoperative complications, although the proportion is significantly lower in patients with EuroscoreII below 4%. The most frequent postoperative complication was the need for hemodynamic support, followed by AKI. However, most of the patients quickly recovered, with ICU and hospital LOS similar to younger patients. Furthermore, long-term follow-up to five years is acceptable in patients at a low risk, showing that the survival of these patients is closer to the average life expectancy of the general population. Octogenarians with low surgical risk can undergo surgery safely, with favorable results up to five years. Nevertheless, the survival proportion is lower in intermediate-high risk patients aged at least 80 years old, and the type of intervention in this subgroup should be discussed case by case by the heart team.
Conflict of interestsThe authors state that they have no conflict of interests.