As short-term mortality continues to decrease after myocardial infarction (MI), secondary prevention strategies attain increasing relevance. This study aimed at assessing the control of cardiovascular (CV) risk factors, including dyslipidemia, hypertension and diabetes, in a contemporary cohort of MI survivors who completed an exercise-based cardiac rehabilitation (EBCR) program.
MethodsObservational, retrospective cohort study including patients admitted to a tertiary center with acute MI between November 2012 and April 2017, who completed a phase II EBCR program after discharge. Achievement of low-density lipoprotein (LD) cholesterol, blood pressure and HbA1c guideline recommended targets was assessed. Lipid profile parameters were assessed and compared at three time points (hospitalization, beginning and end of the program).
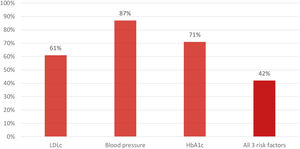
ResultsA total of 379 patients were included. Mean age was 58.8±10.6 years; 81% were male. Considering the European Society of Cardiology's guidelines on contemporary data collection, 61%, 87% and 71% achieved the recommended LDL cholesterol, blood pressure and HbA1c targets, respectively, at the end of the program. Combining all three risk factors, 42% achieved the recommended targets. High-sensitivity C-reactive protein decreased between the beginning and the end of the program [0.14 (0.08-0.29) mg/L to 0.12 (0.06-0.26) mg/L; p<0.001].
ConclusionDespite contemporary management strategies, including enrollment in a structured EBCR program, a substantial number of patients presented suboptimal control of CV risk factors. Considering the dyslipidemia, hypertension and diabetes results, less than half of the enrolled individuals achieved the recommended targets. These findings highlight a pivotal unmet need which could be particularly relevant in improving CV outcomes by enhancing secondary prevention profiles.
À medida que a mortalidade após enfarte agudo do miocárdio (EAM) diminui, as estratégias de prevenção secundária adquirem uma relevância crescente. O objetivo deste estudo foi avaliar o controlo de fatores de risco cardiovascular (FRCV), nomeadamente dislipidemia, hipertensão e diabetes mellitus, em doentes após EAM que completaram um programa de reabilitação cardíaca (PRC).
MétodosEstudo de coorte retrospetivo, observacional, que incluiu doentes admitidos num centro terciário com o diagnóstico de EAM, entre novembro de 2012 e abril de 2017. Foi avaliado o atingimento dos alvos recomendados pelas guidelines da Sociedade Europeia de Cardiologia para colesterol LDL (LDLc), pressão arterial (PA) e hemoglobina glicada (HbA1C). Os parâmetros lipídicos foram avaliados e comparados em três momentos (hospitalização, início e fim do programa).
ResultadosForam incluídos 379 doentes (58,8±10,6 anos, 81% homens). Considerando as guidelines, 61%, 87% e 71% atingiram os alvos recomendados de LDLc, PA e HbA1c, respetivamente, no fim do programa. Combinando os três FRCV, 42% dos indivíduos atingiram os alvos recomendados. Os níveis de proteína C reativa de alta sensibilidade diminuíram entre o início e o fim do programa [0,14 (0,08-0,29) mg/L versus. 0,12 (0,06-0,26) mg/L; p<0,001].
ConclusãoApesar de estratégias contemporâneas, incluindo a participação num PRC, uma proporção importante de doentes apresentou um controlo subótimo dos FRCV. Considerando dislipidemia, hipertensão e diabetes mellitus combinados, menos de metade atingiu os alvos recomendados. Estes dados reforçam a importância da otimização de estratégias de prevenção secundária, dado o potencial impacto em outcomes cardiovasculares.
Patients with previous acute myocardial infarction (AMI) are at very high risk of recurrent events.1–3 As short-term mortality continues to decrease as a result of major overall advances in the management of AMI, secondary prevention strategies encompassing lifestyle modifications, cardiovascular (CV) risk factor control and the use of cardioprotective medications remain of the utmost importance.4,5 Major CV risk factors associated with the development of cardiovascular disease (CVD) include hypertension, dyslipidemia, diabetes, obesity, smoking habits, excessive alcohol consumption, unhealthy diet and a sedentary lifestyle.1,3,6 Several reports have addressed the relationship between these factors and overall CVD burden extensively,7 with recent data highlighting the impact of secondary prevention guideline compliance on mortality.1,5
Pharmacological interventions are one of the pillars in the optimal management of hypertension, dyslipidemia and diabetes.1 Over the last years, different studies have explored the relationship between the prescription of anti-hypertensive drugs, lipid-lowering medication and anti-diabetic agents and CV risk factor control.4,8,9 Almost half of very high cardiovascular risk patients maintain blood pressure (BP) levels above the recommended targets.4,10 Current recommendations for low-density lipoprotein (LDL) cholesterol and glycated hemoglobin (HbA1c) levels among diabetic individuals are also not being met in a large number of patients.4,10–12 Poor compliance with medical therapy, as well as worsening control of risk factors over time are some of the potential explanations for these findings.11,13
Studies have also shown that appropriate lifestyle modifications that affecting the remaining risk factors are not being made. The proportion of obese patients, smokers and sedentary individuals on unhealthy diets (including high alcohol consumption) is still far from optimal.14–16
Exercise-based cardiac rehabilitation (EBCR) programs are one of the hallmarks of optimal contemporary management after an AMI,1,17,18 and are associated with improvements in both mortality and morbidity.18,19 Furthermore, smoking cessation, weight management, physical activity levels, and medication adherence are higher among patients who attend these programs.20 Despite this, there are still important hindrances concerning both patient referral and attendance.4,19
Notably, ischemic heart disease (IHD) remains the most common manifestation of CVD,3 with a relevant proportion of major coronary events occurring in patients with a previous diagnosis of IHD.14 Furthermore, among patients who survive a first AMI, up to 20% can suffer a second CV event in the first year.14 As such, there is a high level of interest in the optimization of secondary prevention measures, in order to optimize residual risk among this challenging subset of patients.1,14,21,22
Given the present data, in this study we aimed to assess the level of CV risk factor control, specifically in terms of hypertension, dyslipidemia and diabetes, in a contemporary cohort of AMI survivors who completed an EBCR program.
MethodsThis was an observational, retrospective cohort study. The study sample comprised all patients discharged from the Cardiology Department of the Gaia/Espinho Hospital Center with a diagnosis of AMI (according to the International Classification of Diseases, 9th edition), between November 2012 and April 2017.
In order to be included, patients had to have completed an EBCR program which consisted of an eight-week long (three sessions per week) outpatient protocol, including endurance and resistance training sessions, prescribed individually by an expert in EBCR. This protocol has been described in further detail in previous studies.17,23 At the beginning and at the end of the program, patients underwent a clinical evaluation, as well as performing a symptom-limited cardiopulmonary exercise testing (CPET) on a treadmill.
Clinical and analytical variablesData for clinical, analytical, and echocardiographic variables were collected from hospital records. Previous history of arterial hypertension, dyslipidemia and diabetes was defined according to the presence of these diagnoses on clinical files. The diagnosis of dyslipidemia was also considered in patients previously under anti-dyslipidemia medication or with LDL cholesterol ≥190 mg/dL.1 Diabetes was also considered in patients previously under anti-diabetic agents and in those with a HbA1c ≥6.5%.24
Blood pressure (systolic BP (SBP) and diastolic BP (DBP)) was measured at rest, at the start of each CPET. Total cholesterol (TC), LDL cholesterol, high-density lipoprotein (HDL) cholesterol, triglyceride (TGL) and HbA1c levels were measured during hospitalization, at the beginning and at the end of the EBCR program. High-sensitivity C-reactive protein (hsCRP) levels were measured at the beginning and at the end of the EBCR program. Statins prescribed at discharge were classified as high-intensity (atorvastatin 40-80 mg or rosuvastatin 20-40 mg) or low-moderate intensity (other regimens).25
Cardiovascular risk factor goals definitionThree independent analyses were performed of BP, LDL cholesterol and HbA1c levels to quantify the proportion of patients who achieved the recommended target values for these parameters according to the European Society of Cardiology (ESC) guidelines.24,26–29 In each of these analyses, patients were dichotomized according to whether they achieved guideline recommended targets or not.
Additionally, lipid profile parameters and their variation over time were also assessed by comparing levels upon hospitalization, at the beginning and at the end of the EBCR program. Lastly, a similar sub-analysis of hsCRP level variations between the beginning and the end of the program was also performed.
Statistical analysisContinuous variables were expressed and compared according to the normality of their distribution, which was assessed by the Kolmogorov-Smirnov test. Variables with a normal distribution were expressed as mean ± standard deviation and those with a non-normal distribution as median (percentile 25-75, interquartile range (IQR)). Categorical variables were expressed as absolute count and percentage. Continuous variables were compared using the independent samples t-test for those with a normal distribution, or with the Mann-Whitney U or Wilcoxon tests (for unmatched and matched data, respectively) for those with a non-normal distribution. Categorical variables were compared with the chi-square test.
All results were two-sided and a p-value under 0.05 was considered as significant. Statistical analysis was performed using IBM SPSS Statistics 26 (Armonk, NY: IBM Corp).
ResultsA total of 379 patients were included (Table 1). Data concerning BP levels were available for all patients (n=379), whereas LDL cholesterol data were available in 328 patients (87%) and for hsCRP in 226 patients (60%). HbA1c levels were available for 86 out of the 100 diabetic patients.
Study population characteristics.
| Age (years) | 58.8±10.6 |
| Male sex | 307 (81%) |
| STEMI | 255 (67%) |
| Revascularisation | 335 (88%) |
| History of CAD | 60 (16%) |
| Arterial hypertension | 203 (54%) |
| Dyslipidemia | 233 (61%) |
| Diabetes | 100 (26%) |
| Smoking status | |
| Current smoker | 173 (46%) |
| Former smoker | 74 (20%) |
| Body mass index | 26.7±3.5 |
| Ejection fraction (%) | 52 (44-56) |
| Reduced ejection fraction | 155 (41%) |
| Medication at discharge | |
| Acetylsalicylic acid | 376 (99%) |
| Clopidogrel | 226 (60%) |
| Ticagrelor | 145 (38%) |
| Anti-coagulants | 27 (7%) |
| ACEi/ARB | 365 (96%) |
| BB | 353 (93%) |
| Spironolactone | 50 (13%) |
| Diuretics | 70 (18%) |
| CCB | 33 (9%) |
| Nitrates | 46 (12%) |
| Nicorandil | 7 (2%) |
| Ivabradine | 2 (1%) |
| Anti-diabetic agents1 | 87 (23%) |
| Insulin | 15 (4%) |
| Statins | 377 (99%) |
| High-intensity statins | 332 (88%) |
ACEi: angiotensin-converting enzyme inhibitors; ARB: angiotensin II receptor blockers; BB: beta-blockers; CAD: coronary artery disease; CCB: calcium-channel blockers; n: number of patients, STEMI: ST-segment elevation acute myocardial infarction.
1 Excluding insulin.
Upon discharge, 88% of patients were under high-intensity statin therapy and 11% were treated with low-moderate intensity statins. Two patients were not under statin therapy at discharge and no patients were treated with ezetimibe.
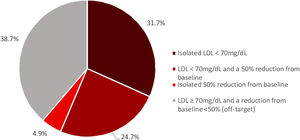
Median LDL cholesterol levels were significantly reduced from 107 (85-135) mg/dL during hospitalization to 66 (52-82) mg/dL at the end of the EBCR program. Considering the 2016 ESC guidelines, 61% of patients achieved the recommended LDL cholesterol target (LDL cholesterol <70 mg/dL or a 50% reduction from baseline),26 with 31.7% having an isolated LDL cholesterol < 70 mg/dL, 4.9% an isolated 50% reduction from baseline and 24.7% having both LDL cholesterol < 70 mg/dL and a 50% reduction from baseline (Figure 1). Patients who achieved this target were more likely to have a history of arterial hypertension (57% vs. 46%, p = 0.041), diabetes (32% vs. 21%, p = 0.025) and to be under anti-diabetic agents other than insulin (28% vs. 17%, p=0.014) and less likely to have a history of dyslipidemia (56% vs. 72%, p = 0.004) than those who did not.
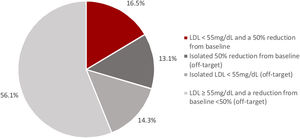
When using the new LDL cholesterol target levels recommended in the 2019 ESC guidelines, only 17% of patients achieved the recommended LDL cholesterol target (LDL cholesterol < 55 mg/dL and a 50% reduction from baseline).28 Among the group that did not achieve the target (83% of patients), 13.1% had an isolated 50% reduction from baseline, 14.3% had isolated LDL cholesterol < 55 mg/dL and 56.1% had both LDL cholesterol ≥ 55 mg/dL and a reduction from baseline < 50% (Figure 2). Patients achieving the target were more likely to be under ticagrelor therapy (54% vs. 37%, p = 0.018) and less likely to have a history of coronary artery disease (6% vs. 17%, p=0.030), dyslipidemia (32% vs. 68%, p < 0.001) and to be under clopidogrel therapy (43% vs. 61%, p = 0.011) when compared to those who did not achieve the target.
Cardiovascular risk factor control: Blood pressureMedian BP was 115/70 (105-125/65-80) mmHg at both the beginning and end of the EBCR program. At the end of the program, 87% of patients achieved the recommended BP target, according to the 2013 ESC guidelines (SBP < 140 mmHg and DBP < 90 mmHg).29 These patients were younger than those who did not achieve the target (58.0 ± 10.4 vs. 64.2 ± 10.2 years old; p < 0.001), more likely to be male (83% vs. 70%; p = .033), to have a reduced ejection fraction (EF) (44% vs. 24%, p = 0.009) and to be under spironolactone therapy (15% vs. 4%; p = 0.039). They were less likely to have a previous history of arterial hypertension (49% vs. 82%, p < 0.001) and calcium-channel blocker (CCB) use (7% vs. 22%; p < 0.001).
When considering the new BP goals recommended in the 2018 ESC guidelines, which recommend a lower target for patients < 65 years old, 90% of patients achieved the target (SBP ≤ 130 mmHg and DBP ≤ 80 mmHg, for patients under 65 years old). These patients were more likely to be under spironolactone therapy (13% vs. 0%; p = 0.042) and less likely to have a history of arterial hypertension (42% vs. 71%; p = 0.003), when compared to those who did not achieve the target.
Cardiovascular risk factors control: Glycated hemoglobinAmong the 86 diabetic patients whose data were available in the present study, median HbA1c levels were lower at the end of the program than during hospitalization [6.40% (6.05-7.05) vs. 7.20% (6.50-8.20); p < 0.001]. A total of 71% of patients achieved a HbA1C target of <7%, whereas a total of 51% of patients achieved a HbA1c target <6.5%.24 Patients who achieved a HbA1c level < 7% were less likely to be under spironolactone (12% vs. 40%; p = 0.003) and insulin (3% vs. 40%; p < 0.001) therapy, compared to those who did not achieve this target. Patients who achieved HbA1C < 6.5% were more likely to be men (89% vs. 71%; p = 0.045) and had a higher EF value [54 (45-58) vs. 47 (37-56); p = 0.025] than the group who did not achieve this target. They were also less likely to have a history of arterial hypertension (61% vs. 81%; p = 0.046), as well as of being under spironolactone (11% vs. 29%; p = 0.045), diuretics (14% vs. 38%; p=0.009), CCB (5% vs. 29%; p = 0.003) or insulin therapy (2% vs. 26%; p = 0.001).
Among diabetic individuals, 42% had all three risk factors within the recommended goals (LDL cholesterol < 70 mg/dL or a 50% reduction from baseline, BP < 140/90 mmHg and HbA1c < 7%, Figure 3). Compared to those who did not achieve all three recommended goals, these patients were less likely to have a history of arterial hypertension and to be under spironolactone and insulin therapy. Considering the latest 2019 ESC guidelines, 11% of individuals achieved the recommended goals for all three risk factors (LDL cholesterol < 55 mg/dL and a 50% reduction from baseline, BP < 140/90 mmHg and HbA1c < 7%).
Time-variation between lipid parameters and hsCRPMedian LDL cholesterol were 107 (85-135) mg/dL upon admission, 60 (47-78) mg/dL at the beginning of the EBCR program and 66 (52-82) mg/dL at the end of the program. Values for TC, TGL and HDLc at each time-point are displayed in Figure 4. Differences between time points (i.e., between admission and the beginning of the program, beginning and end of the program and between admission and the end of the program) for each lipid parameter were statistically significant (p < 0.001 for all comparisons) except for TGL levels between the beginning and end of the program, and for HDLc levels between admission and beginning of the program (Figure 4).
Variation in lipid profile parameters between hospitalization and the end of the program. In each box: bottom edge – 25th percentile; mid-line – median; top edge – 75th percentile. Variations of parameters between each time period were statistically significant (p < 0.001) except for the ones represented on the figure.
Adm: Admission; Beg: Beginning of the EBCR program; End: End of the EBCR program; HDLc: high-density lipoprotein cholesterol; LDLc: low-density lipoprotein cholesterol; TC: total cholesterol; TGL: triglycerides.
Regarding the sub-analysis for hsCRP, there was a significant reduction in median levels between the beginning and end of the EBCR program (0.14 (0.08-0.29) mg/L vs. 0.12 (0.06-0.26) mg/L, p < 0.001).
DiscussionThis study shows a substantial gap in achieving guideline recommended goals for three major CVRF, especially dyslipidemia, hypertension and diabetes, in a post-MI group of patients. Despite the high rates of BP target achievement in the present study, achievement of LDL cholesterol and HbA1c goals was lower. Furthermore, less than half of patients achieved recommended goals for all three risk factors combined. Regarding lipid profile parameters, patients significantly decreased their LDL cholesterol levels in the first weeks after the event. Data also, however, showed that in the long-term there was an increment in their levels (Figure 4).
Cardiovascular risk factor control: LDL cholesterolLow-density lipoprotein is one of the most important determinants in the risk of recurrent events.1,28 Several studies have consistently shown the relevance of lowering LDL cholesterol,28 with a large meta-analysis showing that for each 39 mg/dL (1 mmol/L) reduction in LDL cholesterol there was an approximate 23% decrease in major vascular events.30,31 Therefore, after a CV event, it is of paramount importance to reach the recommended LDL cholesterol goals outlined in the guidelines.28 Nevertheless, patients at very high CV risk often do not achieve recommended targets (with stricter goals), although they are a subgroup which can benefit substantially from intensive lipid-lowering therapies.28,32–36
In this study, we showed that more than one third of patients did not achieve the target of LDL cholesterol < 70 mg/dL or a 50% reduction from baseline (as recommended in the 2016 ESC guidelines26), despite the use of a contemporary approach (as detailed in Table 1). This reveals an important unmet need among these patients. Although it should be acknowledged that 12% of individuals were not under high-intensity statin therapy at discharge and that no patients were under therapy with ezetimibe, we believe these data add to the present evidence-based research in this field and are of clinical relevance. Notably, ezetimibe was not routinely used at this point.30 Although up-titration of high-intensity statins to maximum tolerated doses and prescription of ezetimibe could increase the proportion of patients achieving this target,9,21 these results are in line with the current literature. In this regard, the recently published EUROASPIRE V registry highlights the need for improved lipid control (as 71% of individuals in the study had LDL cholesterol levels ≥70 mg/dL),10 findings also documented by Gitt et al. when assessing 3867 patients after acute coronary syndrome, 1071 of whom had lipid data at follow-up, where most patients had LDL cholesterol levels >70 mg/dL.32
The results were even more substantial when considering the 2019 ESC guidelines,28 which recommend a goal of LDL cholesterol < 55 mg/dL and a 50% reduction from baseline levels. In this context, 17% of patients achieved this target at the end of the EBCR program. This new target was set to lower LDL cholesterol as studies suggested that a greater reduction in LDL cholesterol could lead to improvements in CV risk reduction.9,28,35 Importantly, these LDL cholesterol levels were achieved in recent large-scale trials with the aid of proprotein convertase subtilisin/kexin type 9 inhibitors, the third pillar of current lipid-lowering therapy, which can achieve reductions in LDL cholesterol of approximately 55-60%.34,35 These results are in line with the current data, with a recent study by Allahyari et al. reporting on 25 466 patients after a MI showing that 82.9% of patients had not reached target levels (as 76.6% had not reached an LDL cholesterol level of < 55 mg/dL (1.4 mmol/L) and 6.3% had reached an LDL cholesterol of < 55 mg/dL (1.4 mmol/L) but had not achieved a ≥ 50% reduction in LDL cholesterol).21 Interestingly, in the current analysis, prior history of dyslipidemia at baseline was significantly more prevalent among patients who did not achieve LDL cholesterol goals (for both definitions), potentially suggesting that among these individuals, an earlier and more intensive approach could be of importance to achieve the current targets.9,28 Once more, these results should be interpreted in light of the medication at discharge (as discussed above), and also the possible lack of adherence to anti-dyslipidemia therapy, as described in previous studies.32,37Figure 4 shows lipid parameters’ profile variation between admission and the end of the EBCR program. There was an overall statistically significant reduction of TC, TGL and LDL cholesterol levels between hospitalization and the start of the program and between hospitalization and the end of the program. Interestingly, between the beginning and the end of the program (and therefore relatively early on after the event), there was an increase in both TC and LDL cholesterol levels. These findings could suggest that patients tend to follow recommendations on lifestyle modifications and compliance to therapy in the first weeks after the event, while in the long-term compliance tends to wane.38 As such, strategies aiming at increasing awareness of changes in lifestyle and medication adherence, to achieve the recommended risk factor goals, are of pivotal importance.39
Cardiovascular risk factor control: Blood pressureBlood pressure control is also of the utmost importance after a CV event. A large meta-analysis showed that a SBP reduction of 10 mmHg or a DBP reduction of 5 mmHg could reduce the risk of a coronary event by approximately 25%.40 In this study, BP targets were achieved in most patients. Considering the 2013 ESC guidelines (SBP 140 mmHg and DBP < 90 mmHg),29 87% of patients successfully achieved BP goals, while using the 2018 ESC guidelines, 90% of patients achieved the target (SBP ≤ 130 mmHg and DBP ≤ 80 mmHg, for patients < 65 years old).27 The high rates of BP control in this study could be potentially explained by the fact that approximately half of patients did not have a history of arterial hypertension (46%) and that angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers were prescribed in 96% of patients whereas beta-blockers were prescribed in 93%.
Cardiovascular risk factor control: Glycated hemoglobin (HbA1c)In the present study, 71% of patients achieved the goal recommended in the ESC guidelines (HbA1c < 7%).24 Considering a more-stringent target, which may be suggested in some subgroups of patients as long as not associated with significant hypoglycemia or other adverse effects of treatment,24 51% achieved HbA1c < 6.5%.
The UK Prospective Diabetes Study showed that, although a target of HbA1c < 7% reduced microvascular complications, there was a lack of compelling evidence for the existence of a target which would decrease macrovascular complications.41 Moreover, a long follow-up can be necessary to demonstrate the beneficial effect of HbA1c reduction on CV events.24
More recently, the diabetes treatment paradigm has significantly changed as it has been shown that both sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide 1 receptor agonists reduce the risk of CV events over a range of HbA1c levels.24 Although the data on the prescription of these agents were not present, the interplay between these factors should be kept in mind, when assessing the present data.
Other considerationsLow-grade inflammation has been associated with the early initiation, faster growth and rupture of atherosclerotic plaques.42 In this study, there was a significant reduction in hsCRP levels during the EBCR program. Some factors which could be related to these findings include increases in physical activity and implementation of overall healthier lifestyles.43 Importantly, medication could also be related to this decrease.42
Considering all three risk factors assessed in this study (dyslipidemia, hypertension and diabetes), among diabetic individuals, achievement of recommended goals for these parameters was limited, with only 42% of patients presenting optimal control of all three risk factors (LDL cholesterol < 70 mg/dL or a 50% reduction from baseline, BP < 140/90 mmHg and HbA1c < 7%). As such, 58% of patients in this study sample were at increased risk for the development of CV disease.
As previously described, participation in the EBCR program was associated with significant functional benefits, as attested by the improvements in both peak oxygen consumption (pVO2) and CPET duration.17,23,44 Briefly, pVO2 increased from 22.82±6.04 to 24.18±6.31 mL/kg/min, whereas CPET duration increased form 542 (480–660) to 661 seconds (540–780).17 Given the association between improvements in functional parameters and CV outcomes, as reviewed by Ross et al. and further illustrated in a recent report by De Schutter et al. (where improvements of 1 mL/kg/min in pVO2, when assessed as a continuous variable, were associated with a 10% reduction in all-cause mortality among individuals with coronary heart disease) we believe these results should be kept in consideration, as they are of clinical relevance.45,46 Although acknowledging that data on ambulatory levels of PA throughout the study period as well as on weight variation (and other body composition parameters) could have been of interest, particularly to further ascertain the potential of ancillary strategies to promote achieving CV risk factor goals,47 we believe these caveats should not limit the interpretation of the overall data.
The results of this study emphasize the need for better risk factor control in a secondary CV prevention setting. Beyond structured EBCR programs, to which coronary patients should be referred (as part of the optimal management strategy), further strategies aimed at improving patient adherence to medication and overall healthy lifestyles should also be implemented in routine clinical practice.1 One example of such an approach could be the use of the polypill, a single dose formulation including a statin, an anti-hypertensive agent and aspirin, which has proven to increase patient adherence and could have an impact on further CV event rates.48
Study limitationsSeveral caveats should be considered when interpreting the present results. Firstly, this was a retrospective study with no control group. Secondly, and as detailed above, data concerning weight variation and ambulatory levels of PA, both of which can increase the likelihood of CV events,1 were not available. Furthermore, although general assessment and counseling on smoking cessation is part of the overall management by the attending physician, specific data on smoking cessation was not available for the present study. While these data could be of interest, prior studies have previously addressed this issue.49,50 Thirdly, data regarding medication adherence was also not present. As previously discussed, poor medication adherence could be a potential explanation for the suboptimal and worsening of risk factor control over time.38 As such, further studies should address the relationship between these factors, in terms of overall control of CV risk and events. Additionally, the present data could provide an interesting framework for future studies assessing the role of different methods to improve compliance to therapy, as to address this hinderance.39 Additionally, data regarding lipid-lowering therapy used before the event was not available. Therefore, baseline levels were considered as the LDL cholesterol at hospitalization, instead of the LDL cholesterol in individuals not using lipid-lowering therapies and all individuals with a 50% reduction from baseline levels were considered as on-target, rather than only considering this criterion in individuals with a baseline level between 70 and 135 mg/dL, as stated in the 2016 ESC guidelines.26 Also, in this study, BP was measured once at rest at the start of the CPET. As such, white coat hypertension could be undercover, which would overestimate the proportion of hypertensive patients in the study sample.27 Additional data on out-of-office BP would also be of interest, as expressed in the current guidelines.27 Lastly, this study only comprised patients who completed the EBCR program (see Methods) and treated at a single center. This should be recalled when analyzing the current findings, namely in terms of a better CVRF control (particularly in the setting of LDL choleseterol) when compared to other reports.10,32,36 Generalizations to other settings should, therefore, be made with caution.
While these hinderances should be considered, this study provides relevant data on a contemporary cohort of AMI survivors, in a real-world setting. The present data further reiterates the lack of optimal CVRF control in this context, and the hypothesis that (at least in terms of dyslipidemia) it tends to worsen over time. Given its potential association with CV events, the present observations highlight the importance of further ancillary strategies to promote improvements in CVRF control, particularly among this high risk population.
ConclusionThis study shows that even in optimal contemporary management strategies, which included enrollment in a structured EBCR program, after an AMI, patients have suboptimal control of CV risk factors. Recommended targets for LDL cholesterol, BP and HbA1c were not achieved in a large proportion of patients and, considering the combination of all three factors, less than half achieved recommended targets, thus highlighting a substantial potential for improving CV outcomes in these patients.
The present data highlight the need for further strategies to improve CV risk factor control, a pivotal unmet need in this higher risk subset of individuals.
Conflicts of interestThe authors have no conflicts of interest to declare.