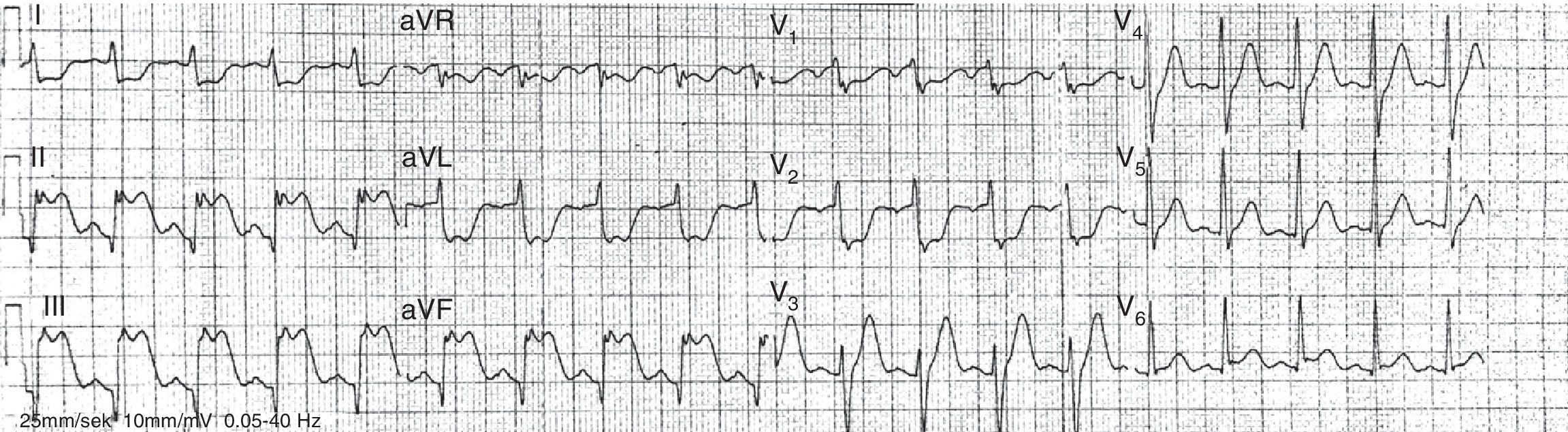
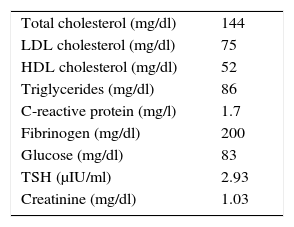
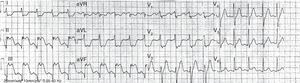
A 28-year-old man with no cardiovascular history or cardiovascular risk factors, who denied cigarette smoking or taking any medications, drugs, supplements or steroids, was referred to the cardiology department after an out-of-hospital cardiac arrest preceded by a four-hour angina episode. The initial rhythm (ventricular fibrillation) was successfully defibrillated. Subsequently, the electrocardiogram suggested inferior and inferobasal ST-elevation myocardial infarction (Figure 1).
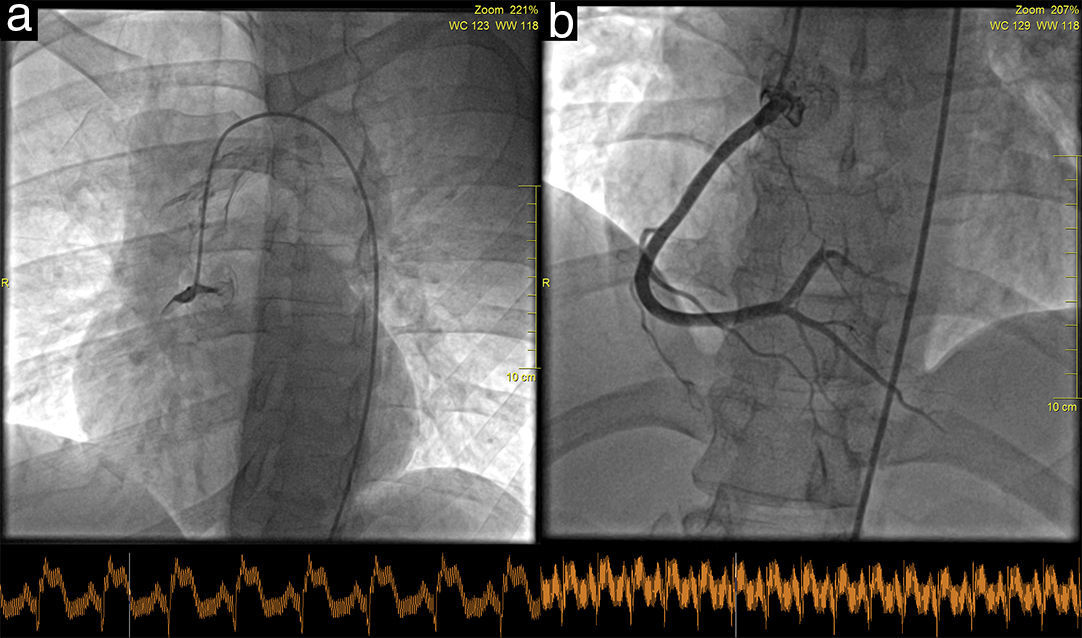
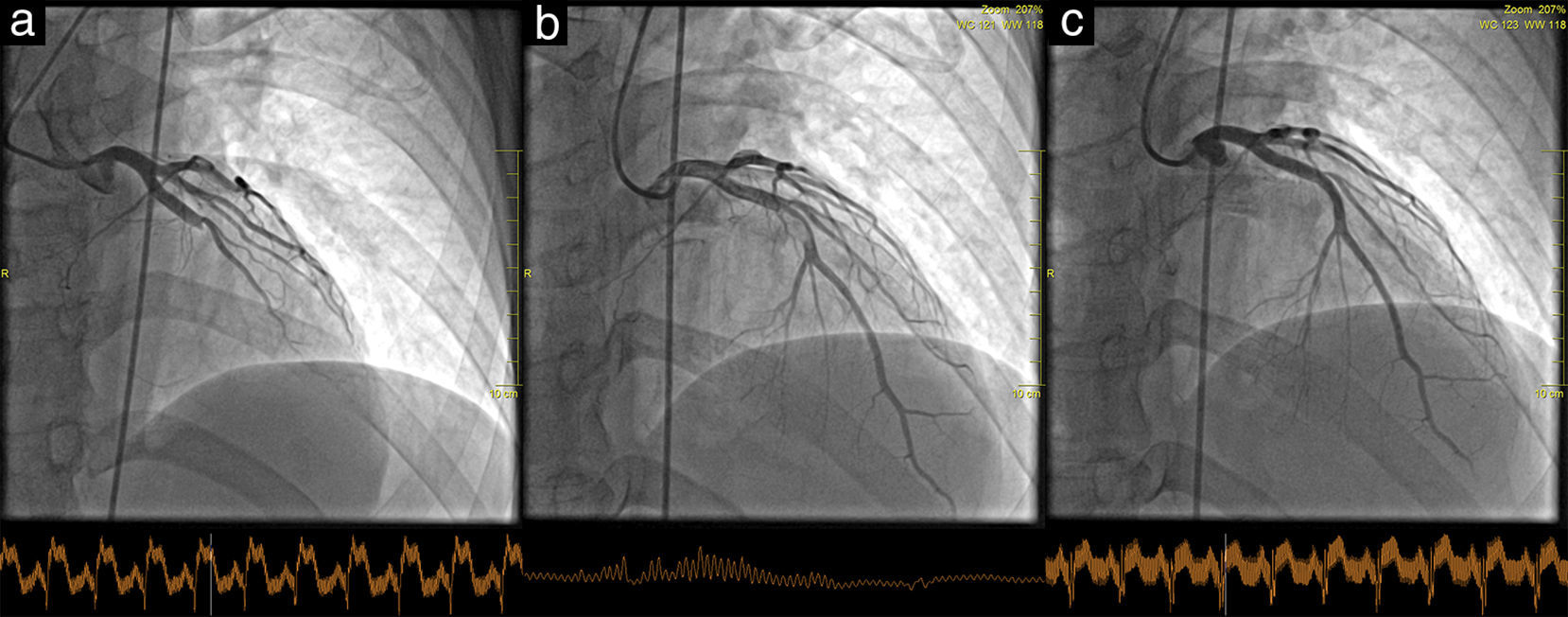
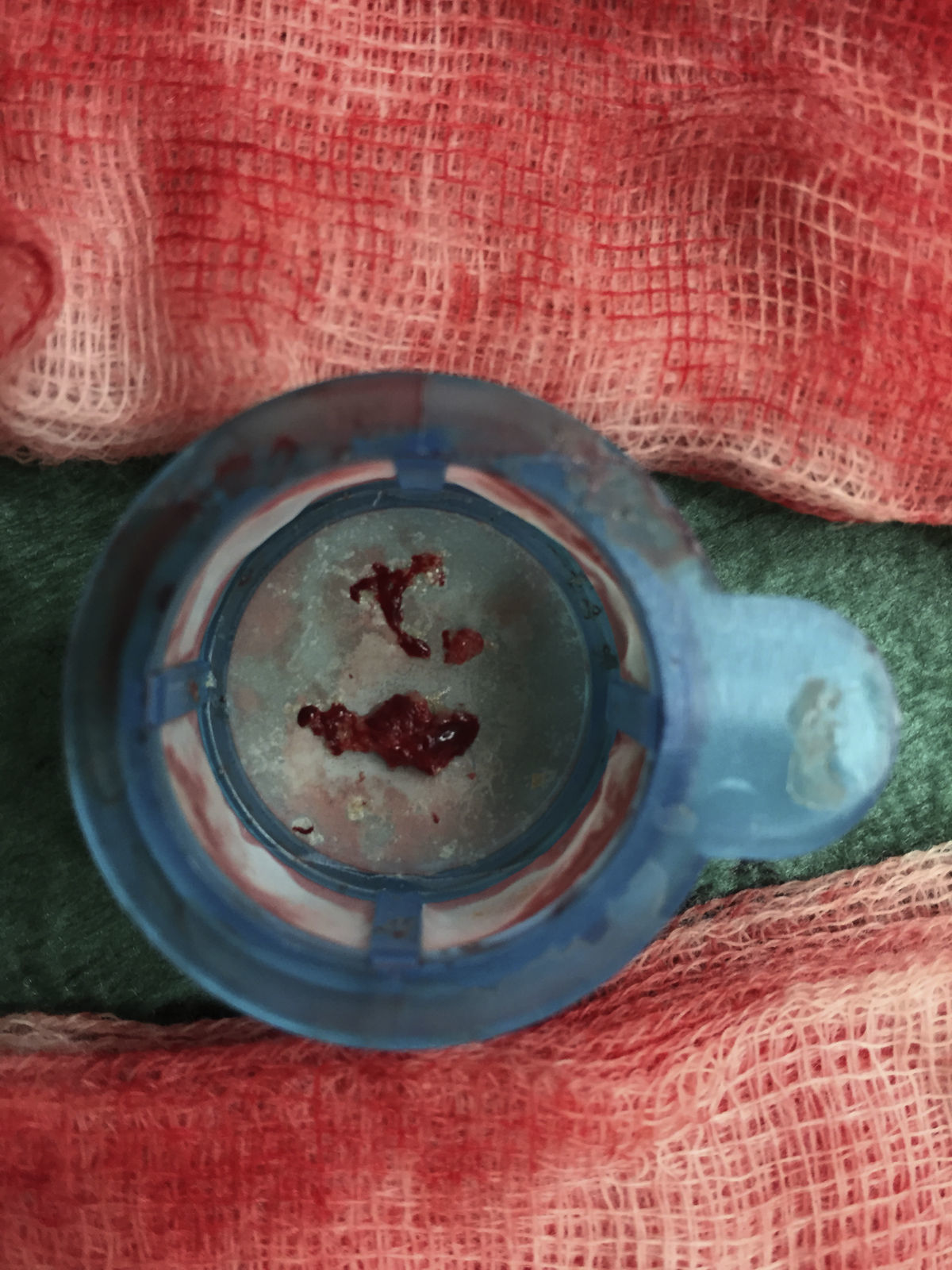
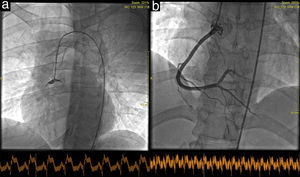
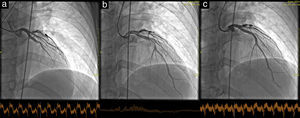
The coronary angiogram showed simultaneous acute thrombosis of the right coronary artery (RCA) (Figure 2a) and of the left anterior descending (LAD) artery (Figure 3a). Initially, to visualize suspected plaque rupture and to aid the decision whether to implant stents, multiple aspiration thrombectomies were performed, resulting in removal of substantial amounts of thrombotic material (Figure 4). After intravenous and intracoronary administration of abciximab, an everolimus-eluting stent was implanted into the RCA, restoring good epicardial coronary flow (Figure 2b). In the LAD spontaneous reperfusion occurred, revealing a massive thrombus (Figure 3b). After aspiration thrombectomy, a stent was implanted (Figure 3c). Echocardiographic examination revealed inferior wall and basal septal akinesis with ejection fraction of 35%. Right ventricular enlargement (5.4 cm in apical 4-chamber view) and hypokinesis (tricuspid annular plane systolic excursion [TAPSE] 14 mm) were present. Right ventricular function was improved on control echocardiography (TAPSE 27 mm).
Additional diagnostics available in our center failed to identify the cause of massive thrombus formation in both coronary arteries. An inflammatory etiology causing massive atherosclerotic plaque destabilization seemed unlikely, as C-reactive protein levels were normal on admission (Table 1). The patient was referred to the hematological department due to suspicion of thrombophilia.
Selected baseline laboratory results.
| Total cholesterol (mg/dl) | 144 |
| LDL cholesterol (mg/dl) | 75 |
| HDL cholesterol (mg/dl) | 52 |
| Triglycerides (mg/dl) | 86 |
| C-reactive protein (mg/l) | 1.7 |
| Fibrinogen (mg/dl) | 200 |
| Glucose (mg/dl) | 83 |
| TSH (μIU/ml) | 2.93 |
| Creatinine (mg/dl) | 1.03 |
HDL: high-density lipoprotein; LDL: low-density lipoprotein; TSH: thyroid-stimulating hormone.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.