We read with much interest the recently published paper by Timóteo et al.1 This study makes an important contribution to the expanding field of risk stratification in myocardial infarction (MI), which is the cornerstone for patient management. The authors developed a simple risk model from a large cohort of real-world MI patients, comprising common and easily accessible clinical variables, constructing a high-performing in-hospital mortality risk score.
Several risk scores have been developed to predict outcomes in patients with acute coronary syndromes. The GRACE score2 is the most widely used and has been shown to outperform other previously developed mortality risk models.3 The ACHTUNG-Rule,4 based on clinical and laboratory parameters, outperformed the GRACE score in its derivation and validation sets but, in addition to requiring a calculator, it still lacks calibration and validation in larger and external cohorts. McNamara et al.5 recently developed a novel in-hospital mortality risk score from a large contemporary cohort, with calibration curves demonstrating its utility even in patients presenting with cardiac arrest, a significant advantage in the context of MI given the difficulty in accurately predicting outcomes in this patient subgroup.
Although the GRACE and ProACS1 scores share some variables, the latter does have some advantages: (i) it is simpler to use in clinical practice, with fewer variables and no need for a calculator; (ii) it uses the same cutoffs for ST-elevation (STEMI) and non-ST-elevation (NSTEMI) MI, unlike GRACE; and (iii) it is particularly useful in identifying truly low-risk patients, as a score of 0 is associated with very low risk of in-hospital mortality (0.4%). In contrast, the GRACE score predicts mortality risk as a continuum, although low-risk strata have been proposed for STEMI and NSTEMI cases.
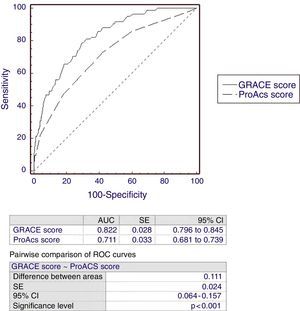
We validated the ProACS risk model in an independent and somewhat more contemporary (2010-2013) cohort of 1000 consecutive MI patients (43.5% with STEMI). Figure 1 illustrates the performance of both GRACE and ProACS for predicting in-hospital mortality in our cohort. Although the intermediate and high-risk strata of the ProACS score identified nearly 98% of in-hospital deaths, confirming the utility of the score in the stratification of ACS patients, its discriminative power was significantly inferior to that reported in its internal and external validation cohorts. Perhaps more importantly, the discriminative performance of ProACS was significantly inferior to that of GRACE.
We believe that any new risk score should provide simplicity without significantly compromising accuracy of risk stratification. Using a more intuitive approach with a measure of risk reclassification, known as the integrated discrimination improvement (IDI) index,6 we noticed that compared with GRACE, the ProACS score is indeed particularly useful in identifying truly low-risk patients who could potentially be considered for conservative management or early discharge (a 56.3% improvement in prediction for patients who did not die during hospitalization). However, this comes at the expense of a significantly lower (61.8%) predictive ability in the identification of patients who eventually die during their hospitalization. The relative IDI index was -5.5%. We further expanded on this by using a category-based measure of risk reclassification known as net reclassification improvement (NRI).6 A positive and significant NRI index translates a net overall successful reclassification of subjects into more appropriate risk categories (e.g. a patient who reaches the primary endpoint who is reclassified into a higher risk group with the new model or a subject who does not reach the primary endpoint who is reclassified into a lower risk category). We used the same risk categories proposed by the GRACE and ProACS investigators. As seen in Tables 1 and 2, altogether the ProACS score reclassified 26.2% of STEMI patients and 17.7% of NSTEMI patients into risk strata which were less accurate representations of their observed mortality risks. However, ProACS did reclassify low-risk NSTEMI patients into more appropriate (lower) risk categories (partial NRI of +9.3%). The above observations suggest that the GRACE score is superior in identifying high-risk patients, whereas ProACS may be more useful in identifying low-risk patients who present with NSTEMI (but not STEMI).
Net reclassification improvement for in-hospital all-cause mortality, comparing ProACS and GRACE scores for ST-elevation myocardial infarction.
| In-hospital all-cause mortality | GRACE (STEMI) | |||||
|---|---|---|---|---|---|---|
| Low risk | Moderate risk | High risk | ||||
| Events (n=48) | ProACS | Low risk | 0 | 0 | 0 | NRI: -26.5% p<0.001 |
| Moderate risk | 1 | 2 | 9 | |||
| High risk | 0 | 0 | 36 | |||
| Non-Events (n=387) | Low risk | 4 | 1 | 0 | ||
| Moderate risk | 81 | 86 | 56 | |||
| High risk | 1 | 12 | 146 | |||
NRI: net reclassification improvement.
For patients with ST-elevation myocardial infarction (STEMI), a GRACE score below 126 was considered low risk, a score between 126 and 154 was assigned to the intermediate risk category and above 154 was assigned to the high risk group.
Net reclassification improvement for in-hospital all-cause mortality, comparing ProACS and GRACE scores for non-ST-elevation myocardial infarction.
| In-hospital all-cause mortality | GRACE (NSTEMI) | |||||
|---|---|---|---|---|---|---|
| Low risk | Moderate risk | High risk | ||||
| Events (n=37) | ProACS | Low risk | 0 | 0 | 2 | NRI: -17.6% p=0.051 |
| Moderate risk | 0 | 1 | 8 | |||
| High risk | 0 | 0 | 26 | |||
| Non-Events (n=528) | Low risk | 20 | 18 | 12 | ||
| Moderate risk | 55 | 82 | 101 | |||
| High risk | 0 | 27 | 213 | |||
NRI: net reclassification improvement.
For patients with non-ST-segment elevation myocardial infarction (NSTEMI), a GRACE score below 109 was considered low risk, while scores between 109 and 140 and above 140 were assigned to intermediate and high risk categories, respectively.
Furthermore, the ability to also estimate mortality during clinical follow-up and across different types of MI would surely improve the applicability of ProACS, since risk models differ significantly in their predictive performance when applied to MI that arises from a primary coronary event (type 1) vs. supply/demand mismatch (type 2).7
In summary, although the authors should be commended for their attempt to improve and simplify risk stratification of MI patients, it remains to be determined whether the simplicity of this new score, derived from a large Portuguese registry, is offset by its inferior prognostic power compared to the gold standard ACS risk score.
Conflicts of interestThe authors have no conflicts of interest to declare.