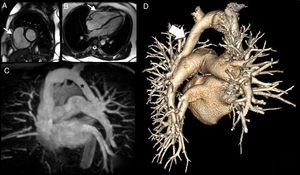
A 57-year-old woman with known asymptomatic paroxysmal atrial fibrillation underwent transthoracic Doppler echocardiography, which revealed mild-to-moderate right ventricular (RV) dilatation, mild tricuspid regurgitation and mild pulmonary hypertension. Cardiac magnetic resonance imaging showed severe right ventricular enlargement (right-ventricular end-diastolic volume index 120 ml/m2, Figure 1, A–B, thin white arrow) without systolic dysfunction (RV ejection fraction of 66%). Magnetic-resonance angiography demonstrated partial anomalous pulmonary venous return (PAPVR) with all left upper lobe veins draining into the left brachiocephalic vein (Figure 1, C, asterisk). Phase-contrast magnetic resonance demonstrated a pulmonary flow/systemic flow of 1.48. Computed tomography angiography confirmed PAPVR with veins from the left upper lobe and also the apical segment of the basal lobe draining through a common vein to the left brachiocephalic vein (Figure 1, D, bold white arrow). PAPVR is a rare cause of right ventricular enlargement in adults with a reported incidence of 0.4-0.7% (2). Patients with these defects are most frequently asymptomatic with the absence of associated abnormalities. Physiologic disturbance is determined by degree of shunting, the number of anomalous veins, any associated valvular abnormalities, presence and size of atrial septal defect and the state the pulmonary vascular bed (3). The isolated evaluation of right ventricular volumes and physiology can mislead diagnosis. In this way, the authors would like to emphasize the importance of multimodality imaging when studying right ventricular disease. Although PAPVR is rare, professionals should be aware of the importance of performing angiographic studies on these patients.
Magnetic resonance imaging, magnetic resonance angiography (MRA) and computed tomography angiography (CTA) images. A) Image of a small cardiac magnetic resonance imaging (CMRI) axis showing dilatation of the right ventricle (thin white arrow). B) Long-term CMRI showing dilatation of the right ventricle (thin white arrow). C) Maximum intensity projection in the anterior view of the coronal plane of the MRA, with the wings of the left upper lobe (LUL) and the apical segment of the left lower lobe (LLL) towards the venous trunk of a common vein (asterisk) for the left brachycephalic venous trunk. D) Rear view of the three-dimensional volume-rendering CTA images revealing a common vein for the LUL and the LLL of the left brachiocephalic venous trunk.
The authors have no conflicts of interest to declare.