Heart failure (HF) is a complex clinical syndrome, affecting millions of people and placing significant strain on healthcare systems, patients and families. Approximately one in every four individuals will develop HF in their lifetime.1 Hypercholesterolemia is an independent risk factor for incident HF, particularly in women, and explains up to 28% of new cases of HF with reduced left ventricular ejection fraction (LVEF) and up to 6% of new cases of HF with preserved LVEF.1,2 Lowering low-density lipoprotein cholesterol (LDL-C) can reduce the burden of HF, and the European Society of Cardiology (ESC) guidelines recommend treatment with statins in patients at high risk of cardiovascular disease (CVD) or with CVD to prevent or delay the onset of HF and HF hospitalizations.2
In contrast to the undisputed effect of statin therapy in the prevention of HF, its role in the treatment of patients with symptomatic HF remains to be fully elucidated. This is an important knowledge gap for three reasons. First, patients with HF have a high residual risk of morbidity and mortality despite guideline-directed medical therapy (GDMT) for HF. Second, ischemic heart disease (IHD), in which LDL-C plays a major pathogenic role, is the most common cause of HF and an important prognostic factor across the entire range of ejection fractions. Globally, IHD is estimated to account for 30.7% of all causes of HF in men and 22.8% in women.3 Among patients hospitalized due to HF, registry data show that about half have an underlying ischemic etiology.4 Third, the anti-inflammatory, antihypertrophic, antifibrotic, and antioxidant effects of statins are potentially beneficial in patients with HF, including those without an ischemic etiology.
The effects of statin therapy on outcomes in stable patients with symptomatic HF were evaluated in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA) and the Gruppo Italiano per lo Studio della Sopravvivenza nell’Insufficienza cardiaca Heart Failure (GISSI-HF) trial.5,6 In the CORONA trial, every patient had IHD and a reduced LVEF. In contrast, the GISSI-HF trial enrolled patients with any LVEF, and 40% had IHD. Both trials randomly assigned patients to receive 10 mg of rosuvastatin or matching placebo once daily. In the rosuvastatin groups, LDL-C was reduced by 40–45% and achieved LDL-C levels were 76–83 mg/dl. The primary endpoint in CORONA was the composite of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke. The primary endpoints in GISSI-HF were time to death, and time to death or admission to hospital for cardiovascular reasons.
Neither of the trials met their primary endpoints and rosuvastatin had no effect on CV mortality, but there was no indication of harm in any subgroup.5,6 Among patients with IHD, statin therapy reduced HF hospitalizations by 15–20% and reduced the risk of myocardial infarction by 19%.7,8 A post hoc analysis of the CORONA trial suggests that a statin-related reduction of atherothrombotic events in patients with HF of ischemic etiology is restricted to those with less advanced HF.9 Among patients without IHD, statin therapy had no effect on the primary endpoints of the GISSI-HF trial.6 Based on these results, the ESC does not recommend routine administration of statins in patients with HF without other indications for their use.2 Additionally, because there is no evidence of harm in patients on statin treatment after the occurrence of HF, the ESC does not recommend discontinuation of statin therapy for patients already treated.2
Nonstatin LDL-C lowering therapies have mixed results in patients with HF of ischemic etiology. In the subgroup of patients with HF enrolled in the IMPROVE-IT trial, the addition of ezetimibe to simvastatin reduced the primary endpoint, a composite of cardiovascular death, nonfatal myocardial infarction, unstable angina requiring rehospitalization, coronary revascularization, or nonfatal stroke.10 In the subgroup of patients with HF enrolled in the ODYSSEY OUTCOMES trial, adding alirocumab to high-intensity statin therapy had no effect on the primary endpoint, death, and the combined HF endpoint of mortality and HF hospitalization, and was associated with a significant increase in nonfatal myocardial infarctions.11 The prognostic effects of inclisiran and bempedoic acid are unknown in patients with or at high risk for atherosclerotic CVD who concomitantly have HF.
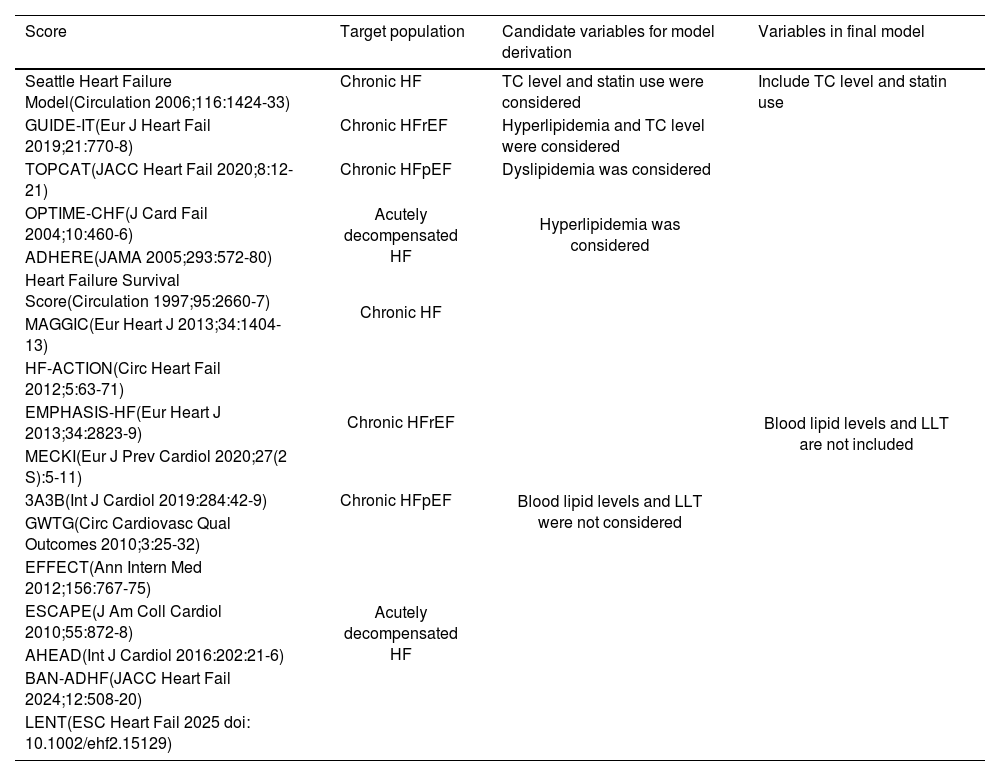
The association between LDL-C levels and outcomes in patients with HF remains unclear. On the one hand, higher LDL-C levels have been associated with better survival in patients with chronic HF, regardless of LVEF, and in patients with acute HF (the “cholesterol paradox”).12,13 On the other hand, LDL-C is not included in contemporary scores used for prognostication in HF (Table 1), suggesting that LDL-C is not a predictor of HF severity and disease progression.
Multiparametric models for risk stratification of patients with HF.
| Score | Target population | Candidate variables for model derivation | Variables in final model |
|---|---|---|---|
| Seattle Heart Failure Model(Circulation 2006;116:1424-33) | Chronic HF | TC level and statin use were considered | Include TC level and statin use |
| GUIDE-IT(Eur J Heart Fail 2019;21:770-8) | Chronic HFrEF | Hyperlipidemia and TC level were considered | Blood lipid levels and LLT are not included |
| TOPCAT(JACC Heart Fail 2020;8:12-21) | Chronic HFpEF | Dyslipidemia was considered | |
| OPTIME-CHF(J Card Fail 2004;10:460-6) | Acutely decompensated HF | Hyperlipidemia was considered | |
| ADHERE(JAMA 2005;293:572-80) | |||
| Heart Failure Survival Score(Circulation 1997;95:2660-7) | Chronic HF | Blood lipid levels and LLT were not considered | |
| MAGGIC(Eur Heart J 2013;34:1404-13) | |||
| HF-ACTION(Circ Heart Fail 2012;5:63-71) | Chronic HFrEF | ||
| EMPHASIS-HF(Eur Heart J 2013;34:2823-9) | |||
| MECKI(Eur J Prev Cardiol 2020;27(2 S):5-11) | |||
| 3A3B(Int J Cardiol 2019:284:42-9) | Chronic HFpEF | ||
| GWTG(Circ Cardiovasc Qual Outcomes 2010;3:25-32) | Acutely decompensated HF | ||
| EFFECT(Ann Intern Med 2012;156:767-75) | |||
| ESCAPE(J Am Coll Cardiol 2010;55:872-8) | |||
| AHEAD(Int J Cardiol 2016:202:21-6) | |||
| BAN-ADHF(JACC Heart Fail 2024;12:508-20) | |||
| LENT(ESC Heart Fail 2025 doi: 10.1002/ehf2.15129) |
HFrEF: heart failure with reduced ejection fraction; HFpEF: heart failure with preserved ejection fraction; LLT: lipid-lowering therapy; TC: total cholesterol.
In this issue of Rev Port Cardiol, Brito et al. retrospectively studied 167 patients admitted for acute HF and found that 1-year mortality was inversely associated with the LDL-C level measured on admission.14 Patients with lower LDL-C levels were older and had higher NT-proBNP levels. Previous studies have shown that patients with low total cholesterol levels more often display characteristics associated with frailty, malnutrition (lower body mass index and serum albumin), and more advanced HF (less favorable hemodynamic profile and lower serum sodium level).15 These and other characteristics that distinguish patients with HF and low LDL-C levels from those with higher LDL-C levels are confounding factors that can generate a spurious inverse association between LDL-C levels and mortality in patients with HF (Table 1). Contrary to LDL-C, these characteristics are included in many multiparametric models used for HF prognostication. It is noteworthy that in the study by Brito et al., several measures of HF severity – such as the hemodynamic profile and the levels of NT-proBNP and serum sodium – were not included in the multivariable analysis. The interpretation of this study is further complicated by the observation that patients alive at 1-year follow-up more often were discharged on statin therapy (66.4% against 16.7% in patients who died within one year after discharge), even though the difference was not statistically different.
In summary, it is reasonable to state that neither the association between LDL-C and HF outcomes nor the role of LDL-C lowering therapy in patients with HF have been fully clarified. We need an adequately powered, pragmatic randomized trial with sufficiently long duration of follow-up to evaluate the potential benefit of statins in patients with HF that is not advanced and who are receiving optimal GDMT including sodium-glucose co-transporter 2 inhibitors and the angiotensin receptor neprilysin inhibitor. Until then, there is insufficient evidence to support withdrawing statins from patients with HF or withholding statins in those with indications for their use.
Conflicts of interestRui Gomes has no conflicts of interest to declare. Carlos Aguiar has received honoraria from Abbott, Abbvie, Amgen, Alnylam, AstraZeneca, Bayer, BiAL, Boehringer-Ingelheim, Daiichi-Sankyo, Ferrer, Gilead, GSK, Lilly, Novartis, Novo Nordisk, Pfizer, Sanofi, Servier, Takeda, and Tecnimede.