Diabetes mellitus is a significant risk factor for the development of heart disease (HD), with heart failure (HF) being one of the early manifestations of the disease in this population. The diagnostic process is challenging and contributes to a significant number of undiagnosed cases of HD among individuals with diabetes. This is largely due to the non-specific nature of symptoms and signs in the initial stages of disease, making early detection elusive. Timely identification and prevention of HD in patients with diabetes have the potential to significantly improve patient prognosis and alleviate the growing burden of this population on the national healthcare system.
Natriuretic peptides (BNP and NT-proBNP) have been recognized as reliable, cost-effective biomarkers for detecting HD and can be further used as risk assessment biomarkers in asymptomatic patients. Despite being recommended in several European and American guidelines to rule-out and rule-in HF, the routine use of these biomarkers for the diagnosis of HDs in patients with diabetes has only recently been proposed by the American Diabetes Association (ADA) and has not yet been implemented in Portugal. Therefore, a multidisciplinary panel of experts from four medical societies, the Portuguese Society of Endocrinology, Diabetes and Metabolism, the Portuguese Society of Cardiology, the Diabetes Study Group from the Portuguese Society of Internal Medicine and the Portuguese Association of Family Medicine were convened to discuss and establish consensus recommendations for natriuretic peptide screening in patients with diabetes and its integration into routine diabetes management protocols.
This manuscript draws on the consensus recommendations from four Portuguese medical societies, offering clear guidance on natriuretic peptides use tailored to Portuguese clinical practice. Accordingly, this consensus advises the use of NT-proBNP analysis for all patients with diabetes aged 50 years and older, or under 50 if they have risk factors and/or comorbidities. Adjusted rule-out and rule-in values for age, sex and risk factors are provided. NT-proBNP levels above 125 pg/mL should prompt additional testing and cardiovascular investigation. Routine evaluation every two to three years for low-risk patients and annually for high-risk patients is proposed when NT-proBNP is below 125 pg/mL and in the absence of suspected heart disease.
A diabetes mellitus é um fator de risco significativo para o desenvolvimento de doenças cardíacas, sendo a insuficiência cardíaca uma das primeiras manifestações da doença nesta população. O processo de diagnóstico é complexo e contribui para um número significativo de casos não diagnosticados de doença cardíaca em doentes diabéticos, devido à natureza não específica dos sintomas e sinais, ou à impossibilidade da sua deteção em fases iniciais da doença. A deteção precoce e a prevenção da doença cardíaca em doentes diabéticos poderão contribuir para melhorar significativamente o prognóstico dos doentes e reduzir os encargos crescentes desta população sobre o Sistema Nacional de Saúde.
Os peptídeos natriuréticos (BNP e NT-proBNP) têm sido reconhecidos como fidedignos, rentáveis e com um peso relevante na deteção de doença cardíaca, podendo ser utilizados como biomarcadores para avaliação de risco em doentes assintomáticos. Apesar de serem recomendados em várias diretrizes europeias e americanas na exclusão ou identificação da insuficiência cardíaca, a utilização sistemática destes biomarcadores para o diagnóstico de doenças cardíacas em doentes diabéticos só recentemente foi proposta pela American Diabetes Association (ADA), não estando ainda em prática em Portugal. Como tal, foi reunido um painel de especialistas de quatro sociedades médicas portuguesas, a SPEDM (Sociedade Portuguesa de Endocrinologia, Diabetes e Metabolismo), SPC (Sociedade Portuguesa de Cardiologia), NEDM-SPMI (Núcleo de Estudos da Diabetes Mellitus da Sociedade Portuguesa de Medicina Interna) e APMGF (Associação Portuguesa de Medicina Geral e Familiar) com o objetivo de discutir e estabelecer recomendações de consenso para o rastreio de péptidos natriuréticos em doentes diabéticos, bem como a sua integração no protocolo de rotina de gestão da diabetes.
Este manuscrito transpõe as recomendações de consenso das quatro sociedades médicas portuguesas, fornecendo orientações claras, e ajustadas à prática clínica portuguesa, sobre o uso dos peptídeos natriuréticos. É recomendada a análise do NT-proBNP em todos os doentes diabéticos com idade igual ou superior a 50 anos, ou inferior a 50 se tiverem fatores de risco e/ou comorbilidades. São fornecidos valores recomendados para exclusão e diagnóstico de doenças cardíacas na população diabética, tendo em conta a idade, sexo e outros fatores de risco. Os níveis de NT-proBNP superiores a 125 pg/mL devem motivar testes adicionais e investigação cardiovascular. Propõe-se uma avaliação de rotina a cada 2-3 anos para os doentes de baixo risco e anualmente para os doentes de alto risco quando o NT-proBNP é inferior a 125 pg/mL e na ausência de suspeita de doença cardíaca.
Diabetes imposes a significant burden on individuals and society. The global estimate of persons affected by diabetes in 2021 reached 537 million people, a figure projected to increase to 700 million by 2045.1 In Portugal, estimates of the prevalence of diabetes in 2021 stood at approximately 1.1 million individuals (14.1% of the adult population), with an associated mortality of around 3.3% of total deaths.2
Individuals with diabetes, both type 1 (T1D) and type 2 (T2D), face an increased risk of developing heart disease, with T2D recognized as an independent risk factor for both atherosclerotic cardiovascular disease and heart failure (HF). Recently, data has emerged documenting HF as a prevalent complication of diabetes and often the inaugural manifestation of heart disease (HD) in these patients.3 Specifically, the risk of HF development in T2D patients is 2–4 times higher than those without diabetes4,5 and therefore, warrants specific screening strategies.6 The latest epidemiological study of HF in Portugal revealed that this condition has an overall prevalence of 16.5% for individuals older than 50 years, and that 90% of the cases were undiagnosed. Additionally, 45% of HF with reduced ejection fraction (HFrEF) patients and 25% of HF with preserved ejection fraction (HFpEF) patients had T2D (PORTHOS study results, Gavina C & Baptista R, personal communication, NOVA Medical School, Lisbon, Portugal, 12 December 2023). Numerous factors, including diabetes duration, poor glycemic control, sex, poorly controlled hypertension, hyperlipidemia, obesity, microalbuminuria and glomerular hyperfiltration, renal dysfunction, ischemic HD and peripheral arterial disease, contribute to the risk of HF in both T2D and T1D patients. Despite the complex and multifactorial nature of HF pathophysiology in patients with diabetes, diabetes can contribute directly to the development of structural HD and HF via systemic, myocardial, and cellular mechanisms,7 a process leading to the so-called “diabetic cardiomyopathy”.8 Therefore, timely and accurate diagnosis of HD in the context of diabetes is critical to delay disease progression and improve quality of life.
This consensus paper summarizes the collective recommendations of the Portuguese Society of Endocrinology, Diabetes and Metabolism (SPEDM), the Portuguese Society of Cardiology (SPC), the Diabetes Study Group from the Portuguese Society of Internal Medicine (NEDM-SPMI) and the Portuguese Association of Family Medicine (APMGF), which support the integration of natriuretic peptides (NPs) testing in the comprehensive management of patients with diabetes. These recommendations apply to the primary care setting as well as to patients with diabetes followed in the hospital for non-cardiac conditions. The document emphasizes the central role of NP testing as an integral element in the early diagnosis and risk assessment of HD. In addition, it provides tailored guidance on the effective use of NPs for the surveillance of HD in Portuguese clinical practice, considering the presence or absence of signs and symptoms, risk factors and comorbidities, while suggesting additional diagnostic tests when deemed appropriate.
The value of early heart disease diagnosis in patients with diabetesThe diagnosis of HD in individuals with diabetes poses a significant challenge due to its potentially asymptomatic nature. Even when symptoms like dyspnea and fatigue do manifest, their lack of specificity often results in delayed or missed diagnoses.9 Indeed, it is estimated that one in three adults with T2D in the United States may harbor asymptomatic or undetected cardiovascular disease.10
Numerous studies have highlighted the intricate relationship between diabetes and HD, emphasizing the need for early detection and management of cardiovascular risk factors.3,11–13 Patients with diabetes who develop HD face higher mortality and increased hospitalization risk compared to their non-diabetic counterparts. Recognizing the substantial global impact of these conditions in terms of burden, mortality, disability, and costs, early diagnosis becomes crucial for modifying unhealthy lifestyles and enhancing effective treatment.14 Notably, screening for HF in these patients, incorporating a comprehensive assessment of medical records and symptom evaluation, proved to be cost-effective, prompting reflection on the potential impact of proactive screening on overall patient well-being and reduced healthcare costs associated with the treatment of HF in this population. The American Diabetes Association (ADA) and the American Heart Association (AHA) jointly recommend regular screening for HF in patients with diabetes, especially for those with additional risk factors such as hypertension and obesity. Diabetic HD, including coronary artery disease and cardiomyopathy, may progress silently without noticeable symptoms in its early stages. The accurate and early identification of HD in patients with diabetes allows for the implementation of preventive measures and prompt initiation of treatment and lifestyle modifications, preserving cardiac function, alleviating symptoms, and enhancing overall quality of life.3 Specifically, early diagnosis of diabetic-associated HD, particularly diabetic cardiomyopathy, facilitates timely targeted interventions, potentially preventing the progression to ACC/AHA stage C HF.15
The pivotal role of prevention in HF and cardiac events is evident in landmark studies. The Screening To Prevent Heart Failure (STOP-HF) randomized trial, which involved patients with cardiovascular risk factors, demonstrated that BNP-based screening, along with collaborative care involving a specialist cardiovascular service, reduces the risk of left ventricular systolic and/or diastolic dysfunction and newly diagnosed HF.16 Another study, the PONTIAC trial, showcased the safe and effective use of RAS antagonists and beta-blockers for prevention of cardiac events in high-risk patients with diabetes.17
In summary, early diagnosis of HD in diabetes improves health outcomes, reduces cardiovascular morbidity and mortality, and enhances quality of life. These findings underscore the critical importance of early detection and management of HD in people with diabetes and highlight the potential for health benefits and resource savings in healthcare systems.
The crucial role of natriuretic peptides in early detection of heart diseaseScreening for structural HD in asymptomatic patients with diabetes is challenging. Easy access to sensitive diagnostic methods would optimize the identification of the patients for echocardiography referral. Natriuretic peptides (NPs), primarily BNP and NT-proBNP, are recognized biomarkers of myocardial stretch and biomechanical stress18 that have been used to aid in the diagnosis, assessment of disease severity and prognosis in HD, including for DM patients.18,19 Slightly elevated NP concentrations in the bloodstream may serve as early indicators of changes in heart structure and function, heightening the risk for future HF, coronary HD, or mortality.10 In the absence of clinically overt HF, this condition has been termed as “heart stress”. The concept of “heart stress,” based on increased NT-proBNP levels in asymptomatic patients with risk factors for HD (i.e. diabetes, arterial hypertension, ischemic HD), has also been introduced by the European Society of Cardiology (ESC), underscoring the pivotal role of NT-proBNP in the early and accurate diagnosis of HD, even in the absence of other symptoms.20
Natriuretic peptides, secreted by cardiac ventricles in response to increased pressure and volume, are sensitive indicators of cardiac stress and dysfunction.11,21 Indeed, NT-proBNP levels have been shown to be a valuable biomarker in the evaluation of HF in patients with diabetes.22–24 A comparative cohort study analyzing the role of NT-proBNP levels in the assessment of individuals with both diabetes and HF concluded that NT-proBNP holds a pivotal role in the comprehensive evaluation of their overall status, facilitating the establishment of appropriate management strategies and subsequent follow-up procedures.23 In addition, a randomized trial revealed an association between NT-proBNP levels and an elevated risk of hospitalization in HF patients, including those with diabetes.24 Collectively, these findings underscore the utility of NT-proBNP as an insightful biomarker for assessing cardiac health beyond conventional imaging assessments.
NT-proBNP, recognized for its high sensitivity and stability, is the most widely employed peptide in Europe for HF diagnosis and management. Its longer half-life, stability at room temperature without requiring additives, and resistance to treatments affecting BNP degradation contribute to its advantageous characteristics over BNP.20,25,26 Elevated NP levels, often observed in HD patients with DM, reflect the severity of the condition, even in the absence of classic symptoms or clear echocardiographic evidence. NP measurements have been successfully combined with clinical risk scores (WATCH-DM) to refine the prediction of incident HF risk for the population of adults with diabetes.27 Furthermore, studies show that elevated NT-proBNP levels predict overall and cardiovascular mortality in T2D patients,19 as well as short-term cardiovascular mortality risk in elderly people, even for those who do not have pre-existing cardiovascular disease.28
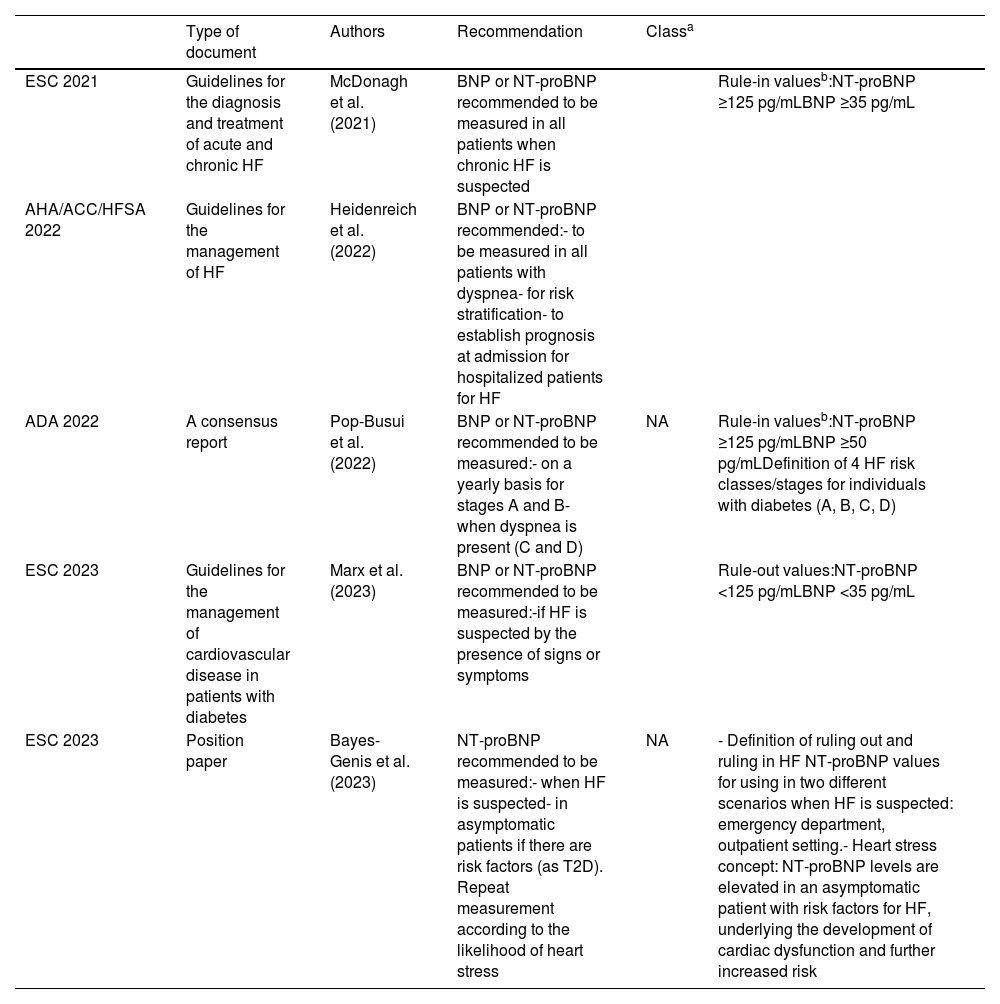
Recent guidelines from the ESC, the American Heart Association/American College of Cardiology (AHA/ACC), and the consensus report of the ADA suggest that the measurement of NPs should be considered for the diagnosis of HF, along with a systematic screening for HF signs and symptoms during each clinical encounter, recognizing the relevance of these biomarkers for the early detection of the disease and risk prediction (Table 1).3,6,20,29 This builds upon previous guidelines where NP usage was solely recommended for ruling out HF.11
Summary of the most recent guidelines on the use of natriuretic for heart failure diagnosis.
| Type of document | Authors | Recommendation | Classa | ||
|---|---|---|---|---|---|
| ESC 2021 | Guidelines for the diagnosis and treatment of acute and chronic HF | McDonagh et al. (2021) | BNP or NT-proBNP recommended to be measured in all patients when chronic HF is suspected | Rule-in valuesb:NT-proBNP ≥125 pg/mLBNP ≥35 pg/mL | |
| AHA/ACC/HFSA 2022 | Guidelines for the management of HF | Heidenreich et al. (2022) | BNP or NT-proBNP recommended:- to be measured in all patients with dyspnea- for risk stratification- to establish prognosis at admission for hospitalized patients for HF | ||
| ADA 2022 | A consensus report | Pop-Busui et al. (2022) | BNP or NT-proBNP recommended to be measured:- on a yearly basis for stages A and B- when dyspnea is present (C and D) | NA | Rule-in valuesb:NT-proBNP ≥125 pg/mLBNP ≥50 pg/mLDefinition of 4 HF risk classes/stages for individuals with diabetes (A, B, C, D) |
| ESC 2023 | Guidelines for the management of cardiovascular disease in patients with diabetes | Marx et al. (2023) | BNP or NT-proBNP recommended to be measured:-if HF is suspected by the presence of signs or symptoms | Rule-out values:NT-proBNP <125 pg/mLBNP <35 pg/mL | |
| ESC 2023 | Position paper | Bayes-Genis et al. (2023) | NT-proBNP recommended to be measured:- when HF is suspected- in asymptomatic patients if there are risk factors (as T2D). Repeat measurement according to the likelihood of heart stress | NA | - Definition of ruling out and ruling in HF NT-proBNP values for using in two different scenarios when HF is suspected: emergency department, outpatient setting.- Heart stress concept: NT-proBNP levels are elevated in an asymptomatic patient with risk factors for HF, underlying the development of cardiac dysfunction and further increased risk |
AHA/ACC/HFSA: American Heart Association/American College of Cardiology/Heart Failure Society of America; ESC: European Society of Cardiology; NA: not applicable.
Natriuretic peptide levels can be influenced by factors such as advanced age, renal dysfunction (low estimated glomerular filtration rate [eGFR]), obesity, atrial fibrillation, anemia, obstructive sleep apnea, pulmonary hypertension, or sepsis.3,30,31 Some factors, like age, sex, chronic kidney disease, and atrial fibrillation, tend to increase NP levels, whereas obesity is associated with their reduction. NT-proBNP levels independently increase with age in healthy individuals, particularly after the age of 70,32 with women often exhibiting higher values than men.33 Higher NP levels have also been associated with a decrease in eGFR as renal functional deteriorates and the decreased renal clearance raises NP concentrations.34,35 Atrial fibrillation (AF), also associated with an elevation of NP levels, may be related to the immediate hemodynamic alterations during the actual episode of AF, since NPs are mainly produced and secreted by the cardiomyocytes in the atria and ventricles in response to hemodynamic wall stress, and are sensitive to heart rate and rhythm disturbances.36,37 In contrast, excess weight and obesity are associated with lower NP levels38,39 potentially linked to impaired NP production.40 Overweight and obese individuals have a 1.4- to 3.5-fold and 1.8- to 4.8-fold increased odds of having low plasma natriuretic peptide levels compared to those with a normal body mass index.41 Adjusting NT-proBNP cut-off values considering these factors may enhance the diagnostic and prognostic accuracy of biomarkers in HF diagnosis.
The Portuguese consensus for early diagnosis of heart disease in patients with diabetesNT-proBNP concentrations to trace and diagnose HD in the outpatient settingIndividuals with T2D are predisposed to an earlier onset of HF compared to those without the disease, and the incidence of HF also rises as they age.42 A Portuguese epidemiological survey indicates a 1.36% (0.39–2.33%) prevalence of chronic HF in the age group of 25–49 years, increasing markedly with age.43 This result is similar to other European reports suggesting a relatively low cardiovascular risk below age 50.33 In light of this, it is proposed that NT-proBNP levels should be assessed for every patient with diabetes aged 50 or above, irrespective of risk factors or comorbidities (Figure 1). For T1D and T2D patients under the age of 50, NT-proBNP analysis is recommended in the presence of risk factors (obesity, hypertension, CKD, coronary artery disease, smoking or HbA1c above target).44,45 It is important to highlight that NT-proBNP levels interact heavily with several clinical factors, namely age, sex, BMI, renal function, heart rhythm and volume status; therefore, the pre-test probability of HD (prior history, risk factors, physical exam) must be taken in consideration when assessing the diagnostic and prognostic value of this biomarker.
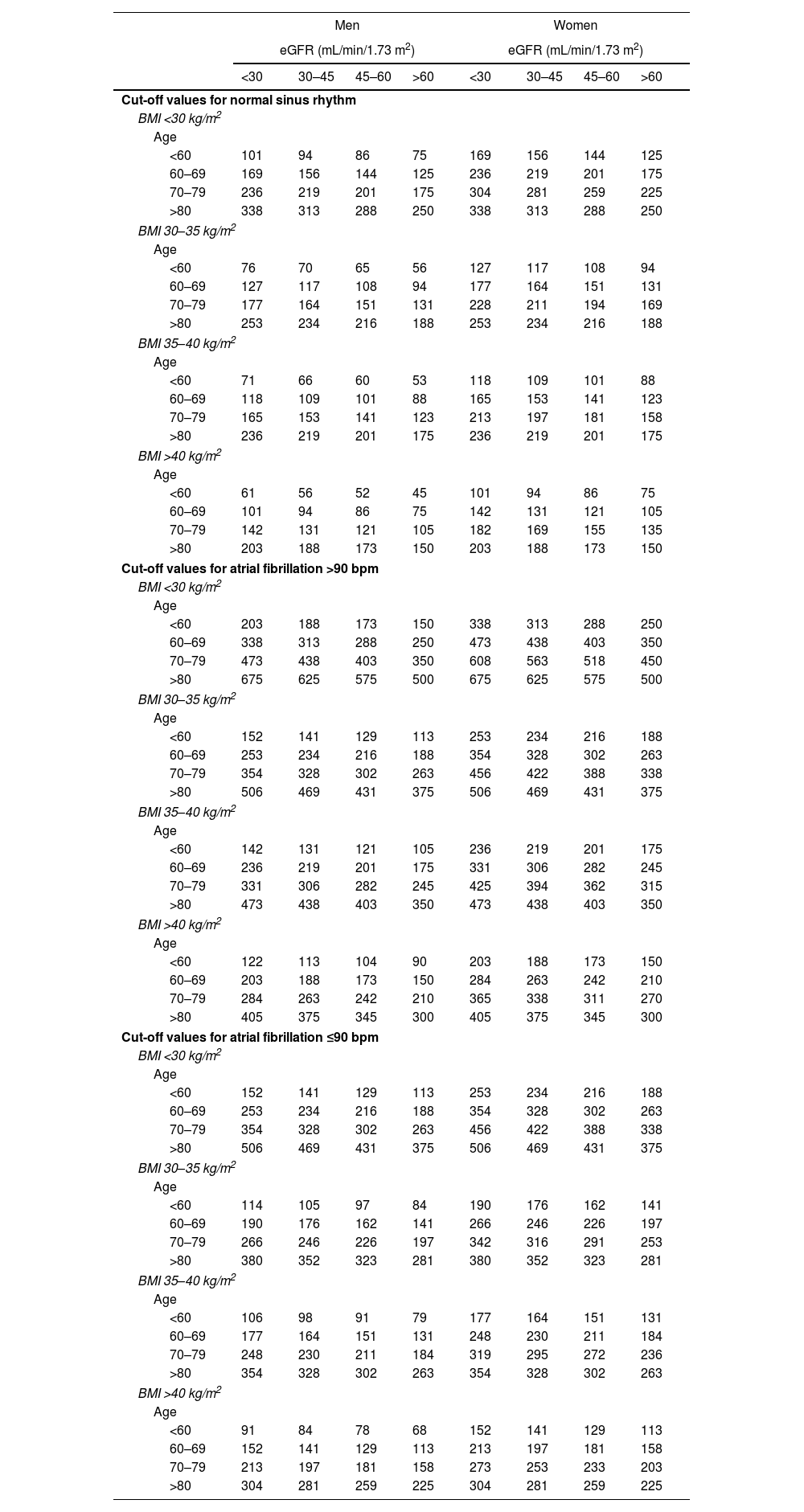
In agreement with European and American guidelines,3,6,11,20 HF and structural HD are considered very unlikely when NP-proBNP concentrations fall below 125 pg/mL. The directive to evaluate NP for DM patients over 50, regardless of symptoms or signs indicative of HD, should be complemented with a comprehensive assessment for HD symptoms (e.g., breathlessness, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, nocturia, fatigue, tiredness, increased time to recover after exercise) and signs (e.g., weight gain, peripheral edema, elevated jugular venous pressure, hepatojugular reflux, third heart sound, or laterally displaced apical impulse).6 Risk factors such as advanced age and sex, along with comorbidities including obesity, chronic kidney disease, and AF, can influence NP concentrations and modify the rule-in levels. The joint SPEDM, SPC, NEDM-SPMI and APMGF consensus proposes NT-proBNP cut-off values adjusted for the aforementioned risk factors and comorbidities (Table 2), based on a previous consensus document by the ESC.20 To facilitate risk calculation, the working group has developed an online application for calculating age-, sex-, and comorbidity-adjusted NT-proBNP cut-off values, which can be accessed at www.calculadorantprobnp.pt.
Cut-off values for the diagnosis of HF adjusted for: age, sex, BMI, renal dysfunction, AF or flutter.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| eGFR (mL/min/1.73 m2) | eGFR (mL/min/1.73 m2) | |||||||
| <30 | 30–45 | 45–60 | >60 | <30 | 30–45 | 45–60 | >60 | |
| Cut-off values for normal sinus rhythm | ||||||||
| BMI <30 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 101 | 94 | 86 | 75 | 169 | 156 | 144 | 125 |
| 60–69 | 169 | 156 | 144 | 125 | 236 | 219 | 201 | 175 |
| 70–79 | 236 | 219 | 201 | 175 | 304 | 281 | 259 | 225 |
| >80 | 338 | 313 | 288 | 250 | 338 | 313 | 288 | 250 |
| BMI 30–35 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 76 | 70 | 65 | 56 | 127 | 117 | 108 | 94 |
| 60–69 | 127 | 117 | 108 | 94 | 177 | 164 | 151 | 131 |
| 70–79 | 177 | 164 | 151 | 131 | 228 | 211 | 194 | 169 |
| >80 | 253 | 234 | 216 | 188 | 253 | 234 | 216 | 188 |
| BMI 35–40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 71 | 66 | 60 | 53 | 118 | 109 | 101 | 88 |
| 60–69 | 118 | 109 | 101 | 88 | 165 | 153 | 141 | 123 |
| 70–79 | 165 | 153 | 141 | 123 | 213 | 197 | 181 | 158 |
| >80 | 236 | 219 | 201 | 175 | 236 | 219 | 201 | 175 |
| BMI >40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 61 | 56 | 52 | 45 | 101 | 94 | 86 | 75 |
| 60–69 | 101 | 94 | 86 | 75 | 142 | 131 | 121 | 105 |
| 70–79 | 142 | 131 | 121 | 105 | 182 | 169 | 155 | 135 |
| >80 | 203 | 188 | 173 | 150 | 203 | 188 | 173 | 150 |
| Cut-off values for atrial fibrillation >90 bpm | ||||||||
| BMI <30 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 203 | 188 | 173 | 150 | 338 | 313 | 288 | 250 |
| 60–69 | 338 | 313 | 288 | 250 | 473 | 438 | 403 | 350 |
| 70–79 | 473 | 438 | 403 | 350 | 608 | 563 | 518 | 450 |
| >80 | 675 | 625 | 575 | 500 | 675 | 625 | 575 | 500 |
| BMI 30–35 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 152 | 141 | 129 | 113 | 253 | 234 | 216 | 188 |
| 60–69 | 253 | 234 | 216 | 188 | 354 | 328 | 302 | 263 |
| 70–79 | 354 | 328 | 302 | 263 | 456 | 422 | 388 | 338 |
| >80 | 506 | 469 | 431 | 375 | 506 | 469 | 431 | 375 |
| BMI 35–40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 142 | 131 | 121 | 105 | 236 | 219 | 201 | 175 |
| 60–69 | 236 | 219 | 201 | 175 | 331 | 306 | 282 | 245 |
| 70–79 | 331 | 306 | 282 | 245 | 425 | 394 | 362 | 315 |
| >80 | 473 | 438 | 403 | 350 | 473 | 438 | 403 | 350 |
| BMI >40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 122 | 113 | 104 | 90 | 203 | 188 | 173 | 150 |
| 60–69 | 203 | 188 | 173 | 150 | 284 | 263 | 242 | 210 |
| 70–79 | 284 | 263 | 242 | 210 | 365 | 338 | 311 | 270 |
| >80 | 405 | 375 | 345 | 300 | 405 | 375 | 345 | 300 |
| Cut-off values for atrial fibrillation ≤90 bpm | ||||||||
| BMI <30 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 152 | 141 | 129 | 113 | 253 | 234 | 216 | 188 |
| 60–69 | 253 | 234 | 216 | 188 | 354 | 328 | 302 | 263 |
| 70–79 | 354 | 328 | 302 | 263 | 456 | 422 | 388 | 338 |
| >80 | 506 | 469 | 431 | 375 | 506 | 469 | 431 | 375 |
| BMI 30–35 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 114 | 105 | 97 | 84 | 190 | 176 | 162 | 141 |
| 60–69 | 190 | 176 | 162 | 141 | 266 | 246 | 226 | 197 |
| 70–79 | 266 | 246 | 226 | 197 | 342 | 316 | 291 | 253 |
| >80 | 380 | 352 | 323 | 281 | 380 | 352 | 323 | 281 |
| BMI 35–40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 106 | 98 | 91 | 79 | 177 | 164 | 151 | 131 |
| 60–69 | 177 | 164 | 151 | 131 | 248 | 230 | 211 | 184 |
| 70–79 | 248 | 230 | 211 | 184 | 319 | 295 | 272 | 236 |
| >80 | 354 | 328 | 302 | 263 | 354 | 328 | 302 | 263 |
| BMI >40 kg/m2 | ||||||||
| Age | ||||||||
| <60 | 91 | 84 | 78 | 68 | 152 | 141 | 129 | 113 |
| 60–69 | 152 | 141 | 129 | 113 | 213 | 197 | 181 | 158 |
| 70–79 | 213 | 197 | 181 | 158 | 273 | 253 | 233 | 203 |
| >80 | 304 | 281 | 259 | 225 | 304 | 281 | 259 | 225 |
BMI: body mass index.
- –
eGFR <30 mL/min/1.73 m2, NT-proBNP cut-off increased by 35%;
- –
eGFR 30–45 mL/min/1.73 m2, NT-proBNP cut-off increased by 25%;
- –
eGFR 45–60 mL/min/1.73 m2, NT-proBNP cut-off increased by 15%;
- –
BMI 30–35 kg/m2, NT-proBNP cut-off reduced by 25%;
- –
BMI 35–40 kg/m2, NT-proBNP cut-off reduced by 30%;
- –
BMI >40 kg/m2, NT-proBNP cut-off reduced by 40%.
- –
For AF or flutter:
- •
ventricular rate ≤90 bpm, NT-proBNP cut-off increased by 50%;
- •
ventricular rate >90 bpm, NT-proBNP cut-off increased by 100%.
- •
To facilitate the cut-off determination process, the standard baseline, age- and sex-adjusted cut-offs were multiplied by the upper referenced factors and stratified by the basal heart rhythm.20
Elevated concentrations of NT-proBNP exceeding the rule-out value of 125 pg/mL warrant further investigation.6 Aligned with European Guidelines, the SPEDM, SPC, NEDM-SPMI and APMGF joint consensus recommends initiating the investigation for HD with a detailed clinical history and selected ancillary studies. Prior history should focus on conditions increasing the risk of HF, as prior history of coronary artery disease (including myocardial infarction and revascularization procedures), arterial hypertension, prior exposure to cardiotoxins and/or thoracic radiation and use of diuretics, along with a dedicated symptom-directed questionnaire, including the most typical and less common symptoms. The physical exam must try to elicit signs of congestion and, seldomly, low output features.46 The FIND-HF (Fatigue, Increased water accumulation/congestion, NP testing, Dyspnea and HF) mnemonic has been proposed to promote both awareness for the condition (HF) and for taking NP measurements in at-risk patients.20
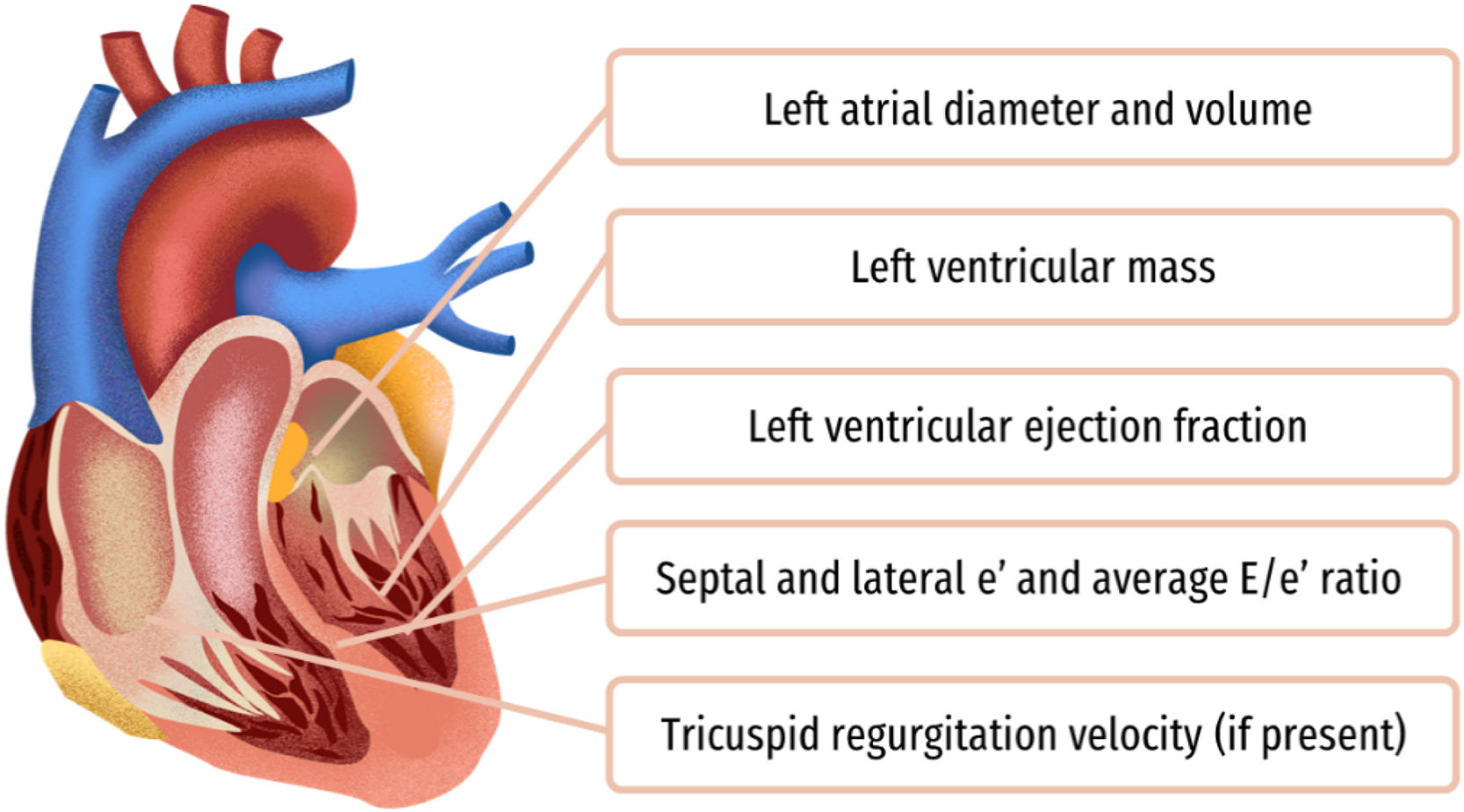
The next step is the request for an electrocardiogram (ECG) and doppler transthoracic echocardiogram (TTE). The threshold for this should be low, taking into consideration the low sensitivity of signs and symptoms. ECGs are advised for detecting arrhythmias, AF, or atrial flutter and abnormalities suggestive of ischemia or left ventricular hypertrophy, serving as baseline for monitoring potential changes in subsequent ECGs. TTEs are recommended to comprehensively assess cardiac function and structure, including left ventricle systolic and diastolic function (Figure 2). A chest X-ray is suggested solely if the clinical evaluation indicates that it would yield additional information. Request for ancillary exams should accompany an investigation aimed at excluding cardiovascular disease, focusing on aspects detailed in Figure 2. In instances where HF is ruled out but NT-proBNP levels are elevated, investigations into other diseases such as AF, chronic kidney disease, pulmonary hypertension, COPD and high-output conditions as liver failure or hyperthyroidism are warranted.
Referral to a cardiovascular specialist is contingent upon clinical evaluation, NT-proBNP levels assessment, and the results of complementary exams. A cardiologist or HF specialist, in addition to confirming or excluding other conditions, will optimize risk factors and comorbidities, assess prognosis, explore potential advanced HD therapies, and establish a collaborative framework with primary care clinicians for ongoing management of symptoms, comorbid conditions, and prognosis.47
Routine evaluationGiven the increased risk of developing HD in patients with diabetes, regular evaluation is recommended. The frequency of NT-proBNP evaluation depends on two main factors: NT-proBNP concentration and the presence of risk factors and/or symptoms of HD (Figure 1). For patients with diabetes without associated comorbidities and NT-proBNP levels below 125 pg/mL, a follow-up evaluation for HD is advised every two to three years. In cases where other risk factors are present (obesity, hypertension, CKD, coronary artery disease, smoking or HbA1c above target) even if NT-proBNP is below 125 pg/mL, an annual assessment of NP levels is recommended.
In instances of elevated NT-proBNP concentrations, the NP levels and results of complementary exams should be taken into account to establish an appropriate follow-up plan. The frequency of evaluation should increase with rising NT-proBNP concentration, the severity of findings in complementary diagnostic testing, and a higher short-term risk of adverse events.
Implications for therapeutic approachThe identification of HD in patients with diabetes has important implications for clinical practice. For patients with HFpEF, sodium-glucose cotransporter 2 inhibitors (SGLT2i) are proven to reduce HF hospitalizations, and treatment with spironolactone or sacubitril/valsartan can be considered.3 For HFrEF, the recommendations from guideline-directed medical therapy for patients with or without diabetes are similar.3,6 QYEsuadruple therapy is recommended to reduce the risk of HF hospitalization and death: angiotensin receptor neprilysin inhibitors (ARNI)/ACE-I as sacubitril/valsartan, mineralocorticoid receptor antagonists as spironolactone, beta-blockers, and SGLT2i as dapagliflozin, empagliflozin, or sotagliflozin.6,46 Diuretics are recommended for both HFpEF and HFrEF when there are signs and/or symptoms of fluid overload.
For patients with elevated levels of NT-proBNP levels without criteria for the diagnosis of HF or other cardiac disease, the evidence to guide the clinical practice is scarce. The PONTIAC trial supports the initiation and up-titration of RAS antagonists and beta-blockers in patients with diabetes with elevated NT-proBNP (>125 pg/mL) but free of cardiac disease.17 SGLT2is have shown reductions of HF events in patients with diabetes even in the absence of previous diagnosis of HF and their use must be strongly considered when NP levels are elevated.48 GLP-1 receptors have been shown to decrease the risk of HF events in patients with diabetes without previous diagnosis of HF,49 and their use must be considered in those without reduced left ventricle ejection fraction.50 In all cases, promotion of healthy lifestyle behaviors and intensive management of cardiovascular risk factors is recommended.51
ConclusionsHeart disease in patients with diabetes is often overlooked or diagnosed at an advanced stage. This paper presents the consensus position of the SPEDM, SPC, NEDM-SPMI and APMGF on the use of NPs, particularly NT-proBNP, for the diagnosis of HD in patients with diabetes, even in asymptomatic cases, to assess risk and monitor progression. Early diagnosis improves patient outcomes through prognosis-modifying interventions and lifestyle changes, reducing morbidity and mortality. This paper also highlights the critical role of primary care in screening patients with diabetes for HD using NPs, providing practical guidance to improve care, cardiovascular prevention, and quality of life for people with diabetes in Portugal.
Key points of consensus include:
- •
NT-proBNP quantification is recommended for all patients with diabetes over 50, or under 50 if risk factors and/or comorbidities are present.
- •
Adjusted rule-out and rule-in values for NT-proBNP for age, sex and risk factors, are provided in Table 2.
- •
For elevated NT-proBNP, complementary diagnostic tests such as electrocardiography and echocardiography are recommended, followed by an investigation for cardiovascular disease.
- •
Routine re-evaluations are recommended when NT-proBNP is below 125 pg/mL and HD is not suspected, occurring every two to three years for patients with diabetes without risk factors and yearly for those with risk factors or comorbidities.
The authors would like to thank Carla Gomes and Mafalda Costa (W4Research) for the writing support and Roche Diagnostic Portugal for funding.