Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in Portugal, thus it is important to identify individuals at risk. Patients with hypertension have an increased risk of adverse cardiovascular (CV) events. The role of LDL cholesterol (LDL-C) in atherosclerotic CVD is well-established. SCORE2, a new CV risk calculation tool, is used to predict the 10-year risk of fatal or non-fatal CVD. The aim of this study was to understand the impact of SCORE2 on CV risk assessment in a population with hypertension from a moderate risk country, compared to the previously used SCORE.
MethodsThis observational cross-sectional study analyzed a population census of 3146 patients diagnosed with hypertension without complications (K86). After applying inclusion and exclusion criteria, 654 patients were included. Data from medical records were collected to calculate and compare SCORE and SCORE2 categories and LDL-C targets.
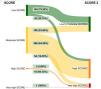
ResultsPatients were classified into SCORE categories: 188 (28.75%) low, 448 (68.5%) moderate, 17 (2.6%) high and 1 (0.15%) very high risk. Using SCORE2, individuals in the SCORE low risk category were reclassified, requiring new targets: 149 individuals (80%) as low to moderate and 39 (20%) as high risk. These differences became more evident when considering SCORE moderate and high-risk categories, where 358 patients (77%) received a higher CV risk categorization, and therefore a lower LDL-C target. There was a significant increase in individuals failing to meet the target when using SCORE2, compared to SCORE (p<0.001).
ConclusionThese findings support the importance of CV risk assessment using SCORE2 algorithm in patients with hypertension.
As doenças cardiovasculares (DCV) são a principal causa de morbimortalidade em Portugal, tornando-se importante identificar indivíduos em risco. Os hipertensos apresentam um risco aumentado de eventos cardiovasculares (CV) adversos. O papel do colesterol LDL (C-LDL) nas DCV ateroscleróticas está bem estabelecido. A nova ferramenta de cálculo do risco CV SCORE2 é usada para predizer o risco de DCV fatais e não fatais a 10 anos. O objetivo deste estudo é compreender o impacto do uso do SCORE2 no cálculo do risco CV, numa população de hipertensos, comparado com o SCORE.
MétodosEste estudo observacional transversal analisou um censo populacional de 3146 pacientes com hipertensão sem complicações (K86). Depois de aplicados os critérios de inclusão e exclusão, incluíram-se 654 pacientes. Colheram-se dados dos registos clínicos para calcular e comparar categorias do SCORE e SCORE2 e alvos de C-LDL.
ResultadosOs pacientes foram classificados nas categorias do SCORE: 188 (28,75%) baixo, 448 (68,5%) moderado, 17 (2,6%) alto e 1 (0,15%) muito alto risco. Usando o SCORE2, os indivíduos na categoria de baixo risco foram reclassificados, exigindo-se novos alvos: 149 (80%) para risco baixo a moderado e 39 (20%) para alto risco. Estas diferenças tornam-se mais evidentes nas categorias de moderado e alto risco, onde 358 pacientes (77%) apresentaram categorizações de risco superiores com o SCORE2, implicando alvos de C-LDL mais baixos. Houve um aumento significativo de indivíduos fora do alvo usando o SCORE2, comparado com o SCORE (p < 0,001).
ConclusãoEstes resultados reforçam a importância do cálculo do risco CV usando o SCORE2 em hipertensos.
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity in Portugal.1 In 2016, the direct and indirect costs of atherosclerosis accounted for approximately 1% of the national gross domestic product and 11% of current healthcare expenditure, imposing a significant economic burden.2,3
In recent decades, various modifiable risk factors for atherosclerotic CVD have been identified. Today, we know that the most significant modifiable risk factors include the presence of apolipoprotein B-containing lipoproteins in the blood (with non-HDL cholesterol levels serving as a representative marker), smoking, hypertension, and diabetes (DM). The most recent data in Portugal revealed a prevalence of hypertension of 42%.4 Therefore, it is crucial to identify individuals who would benefit from the correction of these risk factors, in order to establish goals, individualize therapy, and estimate the potential benefits in terms of primary and secondary prevention.5,6
The causal role of LDL cholesterol (LDL-C) and other apolipoprotein B-containing lipoproteins in the development of atherosclerotic CVD is now well-established. On the one hand, the cumulative burden of LDL-C throughout an individual's life is a determining factor in the onset and progression of atherosclerotic CVD. On the other hand, reducing LDL-C levels proportionally decreases the risk of CVD, even at low levels of LDL-C (e.g., LDL-C <55 mg/dL), regardless of the specific medication used.6–10
Cardiovascular risk assessment toolsThe Systematic Coronary Risk Assessment (SCORE) tool was developed to calculate cardiovascular (CV) risk for each individual, Initially, it was introduced in 2003 for the European population, it provides an estimate of the 10-year risk of a fatal CV event. The tool categorized different European regions into low- and high-risk levels; the calculated risk holds the same significance regardless of the patient's age.11 In Portugal, this tool has been integrated into SClínico™, the clinical records system used by general practitioners (GPs).
In 2021, a new CV risk calculation tool called SCORE2 was introduced. SCORE2 is a calibrated algorithm designed for more recent cohorts and is used to predict the 10-year risk of fatal or non-fatal CVD in a stratified European population across four risk levels. Its primary objective is to enhance the identification of individuals at a higher risk of developing CVD. SCORE2 serves as the foundation for personalized care and should be applied across various populations, ranging from apparently healthy individuals to those with known CV risk factors. The SCORE2 tool incorporates five variables: age, gender, smoking status, systolic blood pressure (SBP), and non-HDL cholesterol, with the latter being one of the primary differences compared to the previous SCORE.12
Categorization of cardiovascular riskAccording to the new risk stratification using SCORE2, three risk categories have been established: low to moderate, high, and very high risk.12
Some patients are directly categorized into a specific risk category based on their past medical history. The presence of established atherosclerotic CVD, such as acute coronary syndrome, ischemic heart disease, cerebrovascular disease, or peripheral artery disease, indicates a very high risk. Depending on the presence of target organ damage, its severity, duration, and concomitant risk factors, individuals with type 2 DM can be classified into different risk categories. The same applies to patients with a history of chronic kidney disease (CKD), based on the severity of the condition. Patients with familial hypercholesterolemia are considered to have a high CV risk.12 For individuals who do not have any of the aforementioned conditions, their CV risk should be calculated using the SCORE2 tool if they are between 40 and 69 years of age, or the SCORE2-Older Persons tool if they are over 69 years of age.12
Age is the primary risk factor for CVD.12 Unlike the previous SCORE, in SCORE2, the same CVD risk at different ages carries a different meaning. If one takes the example of a person aged 55 with a 4% risk of developing a fatal or non-fatal CV event in 10 years, this individual falls into a higher risk category (high risk) compared to a person with a 4% risk at age 60 (low to moderate risk).
LDL-C target valuesAccording to the latest guidelines on CVD prevention, the management of dyslipidemia should encompass two steps: initially, efforts should be made to lower LDL-C levels to below 100 mg/dL, and subsequently, the focus should be on achieving the intensified goals based on the assigned risk category.13
Portuguese primary care realityThe International Classification of Primary Care, 2nd edition (ICPC-2), classifies the patient's reason for encounter, the problems/diagnosis managed, interventions, and the ordering of these data in the structure of care episodes in general/family practice and primary care.14
In primary care, patients with hypertension and/or diabetes are a vulnerable population requiring regular follow-up consultations, intended for the stabilization of existing diseases and preventive measures, particularly for the management of CV risk factors. Hypertension is codified as a problem/diagnosis according to ICPC-2: K86 – hypertension without complications and K87 – hypertension with complications.
As mentioned above the SCORE tool remains integrated into the medical record system SClínico™ as the CV risk calculator for patient stratification and management. This tool is currently outdated in view of the most recent guidelines.13 This could, therefore, have implications for routine clinical practice, particularly for therapeutic decision-making.
ObjectivesThe aim of this study was to understand the impact, in a moderate risk country, on the CV risk assessment using the SCORE2 tool on a population of individuals with hypertension, compared to the previously used SCORE calculation.
MethodsStudy type and populationThis observational cross-sectional study analyzed a population census of patients diagnosed with hypertension without complications (K86) according to ICPC-2 at the Nova Via Family Health Unit (n=3146). Sample recruitment was carried out through the MIM@UF™ platform, which is normally used in Portuguese primary care for data collection. The period under analysis ran from 1 January to 30 June 2022.
The patient selection steps can be found in the flowchart in Figure 1. First, we applied the only inclusion criteria – age between 40 and 69 years – and excluded 1401 patients. We applied our exclusion criteria in two steps. In the first one, 533 patients who had conditions leading to a direct CV risk category allocation were excluded automatically using, once again, the ICPC-2 classification codes for those conditions. Then, in a second step and after analyzing the patients’ electronic data using the SClínico™ software, we excluded 558 patients who met the following exclusion criteria: no in-person consultation in the period under analysis; no lipid profile entered into the system between one year prior to the consultation and June 30, 2022; no record of information regarding smoking, SBP and/or anti-dyslipidemia medication; CKD stage 3 or higher and also those who had coding errors in their clinical records. After applying the inclusion and exclusion criteria, the final sample size included 654 patients.
The research protocol was approved by the Ethics Committee of the Northern Regional Health Administration (Administração Regional de Saúde do Norte).
Data collectionThe authors consulted the patients’ medical records, collecting data regarding age, date of consultation, lipid profile values, smoking habits, SBP, usual medication, the SCORE value calculated by the tool implemented in the SClínico™ program and the SCORE2 value recorded by the physician. When SCORE or SCORE2 values were not registered on the clinical record, the researchers calculated them as recommended by the 2012 European Society of Cardiology (ESC) guidelines15 or by using the online tool U-prevent™, respectively. LDL-C targets for each SCORE and SCORE2 risk categories were defined according to 2019 ESC/EAS guidelines for the management of dyslipidaemias16 and 2021 ESC guidelines on CVD prevention in clinical practice,13 respectively. Statins intensity was determined according to 2018 American Heart Association Guidelines on the Management of Blood Cholesterol.17
Data were stored in a Microsoft Office Excel™ program file database and were encrypted and password protected.
Statistical analysisFor statistical analysis of the data, Microsoft Office Excel™ and SPSS™ software were used. To compare the fulfillment of LDL-C targets using SCORE and SCORE2 a McNemar test was applied. Data obtained were summarized in tables and figures and described quantitatively.
ResultsCharacterization of the population in the studyThis study included a total of 654 individuals, aged between 40 and 69 years, of whom 263 (40.21%) were men and 391 (59.79%) were women (Table 1). The mean age±standard deviation of all patients was 59±7 years (59±7 years for women and 58±7 years for men) with the larger group aged between 60 and 69 years (n=334, 51.07%). Most individuals were non-smokers (n=561, 85.78%). In the smokers’ group, 51 (54.84%) were men, with the highest percentage of smokers in the 50–59 age range. Based on SBP, the median (interquartile range) value was 134 (18.75) mmHg; lower median values were found in the women's group compared to the men's group.
Characterization of study population.
| n (%) | Mean age±SD, years | Smokers, n (%) | Median SBP, mmHg (IQR) | |
|---|---|---|---|---|
| Male | 263 (40.21) | 58±7 | 51 (7.80) | 136 (16) |
| 40–49 years | 41 (6.27) | 45±3 | 10 (1.53) | 135 (43.4) |
| 50–59 years | 92 (14.07) | 55±3 | 23 (3.52) | 136 (40.05) |
| 60–69 years | 130 (19.88) | 64±3 | 18 (2.75) | 136 (33) |
| Female | 391 (59.79) | 59±7 | 42 (6.42) | 132 (18.5) |
| 40–49 years | 58 (8.87) | 46±3 | 6 (0.92) | 125 (35.35) |
| 50–59 years | 129 (19.72) | 55±3 | 21 (3.21) | 130 (39.8) |
| 60–69 years | 204 (31.19) | 65±3 | 15 (2.29) | 135 (36.5) |
| Total | 654 (100) | 59±7 | 93 (14.22) | 134 (18.75) |
IQR: interquartile range; SBP: systolic blood pressure; SD: standard deviation.
When using the SCORE tool to assess CV risk, 188 of the 654 patients (28.75%) were classified as CV low risk and 448 (68.5%) as moderate risk. Finally, 17 patients (2.6%) were classified as high risk and only one male patient (0.15%) as very high risk (Figure 2). For further detail on gender distribution refer to supplementary material – Table 1.
Upon switching to the SCORE2 tool, patients were redistributed into three categories instead of the four in SCORE. Specifically, 255 patients (38.99%) were classified as low to moderate risk with a predominance of female gender, 328 (50.15%) as high risk and 71 (10.86%) as very high risk, primarily consisting of males (Figure 2). For further details on gender distribution, please refer to the supplementary material – Table 2.
When comparing the two methods of assessing CV risk (Figure 3), the low risk group determined by the SCORE tool was recategorized using the SCORE2 algorithm: 149 individuals (79.26%) were categorized as low to moderate risk, 39 (20.74%) as high risk, and none as very high risk. Regarding the moderate risk category determined by SCORE, the transition to the SCORE2 calculator resulted in 106 patients (23.66%) remaining in the low to moderate risk category, while 288 (64.29%) were reclassified as high risk and 54 (12.05%) as very high risk. These discrepancies became even more pronounced when analyzing the high-risk category determined by SCORE: only one patient (5.88%) remained in the same category, while 16 (94.12%) were classified as very high risk.
Lipid profile and lipid-lowering therapyThe median (interquartile range) of total cholesterol, HDL-C and LDL-C, was 189 (48) mg/dL, 49 (16) mg/dL and 112.4 (36.7) mg/dL, respectively. These values were higher in the women's group compared to men (Table 2). Analyzing by SCORE risk category, LDL-C median values were higher in the high-risk category [115 (41.4) mg/dL], followed by the low [113.1 (36.85) mg/dL] and moderate [111.9 (37.25) mg/dL] risk categories. The only individual representing the very high-risk category had an LDL-C level of 141 mg/dL (supplementary material – Table 3). Considering SCORE2 risk categories, LDL-C median values were higher in the very high-risk category [114.6 (36.4) mg/dL], followed by the high and low to moderate risk categories, with minimal differences [113.3 (38.85) mg/dL and 111.4 (34.15) mg/dL, respectively] between them (supplementary material – Table 4).
Characterization of study's population lipid profile.
| Median TC (IQR), mg/dL | Median HDL-C (IQR), mg/dL | Median LDL-C (IQR), mg/dL | |
|---|---|---|---|
| Male | 181 (50.5) | 45 (14) | 108.6 (37.5) |
| 40–49 years | 183 (12) | 43 (19) | 119 (46) |
| 50–59 years | 184.5 (13) | 43.5 (15) | 110.2 (51.25) |
| 60–69 years | 177.5 (14) | 47 (15.75) | 102.6 (42.75) |
| Female | 194 (43.75) | 52 (15) | 115 (36.7) |
| 40–49 years | 189.5 (13.5) | 47 (18.25) | 113.8 (38.75) |
| 50–59 years | 193 (18.25) | 52 (18) | 112.8 (46.75) |
| 60–69 years | 196 (15) | 53.5 (17) | 115.7 (45.5) |
| Total | 189 (48) | 49 (16) | 112.4 (36.7) |
HDL-C: high-density lipoprotein cholesterol; IQR: interquartile range; LDL-C: low-density lipoprotein cholesterol; TC: total cholesterol.
A similar analysis was applied to lipid-lowering therapy (LLT). Concerning SCORE, in the low risk category, 43 patients (22.87%) were treated with a moderate intensity statin in monotherapy, while more than half (n=128, 68.09%) did not use any LLT. In the moderate risk category, the most commonly prescribed LLT was a moderate intensity statin (n=210, 46.88%), followed by a high intensity statin (n=34, 7.59%) and a low intensity statin (n=9, 2.01%), all of them in monotherapy; 171 individuals (38.17%) in this category were not medicated with LLT. In the high-risk group, 9 patients (52.94%) used a moderate intensity statin in monotherapy and eight patients (47.06%) did not use any LLT. The only individual in the very high-risk category was not treated with LLT. Addressing SCORE2 risk categories, the majority of patients in the low to moderate risk category were not using any LLT (n=153, 60%). Among those who were, a moderate intensity statin in monotherapy was the preferred LLT. In the high and very high-risk categories, most patients were treated with a moderate intensity statin in monotherapy, and approximately 40% in both groups did not take any LLT (126 and 29 patients, respectively). Detailed results are provided in Tables 3 and 4.
Use of lipid-lowering treatment according to SCORE risk category.
| Low, n (%) | Moderate, n (%) | High, n (%) | Very high, n (%) | |
|---|---|---|---|---|
| Low intensity statin | 5 (2.66) | 9 (2.01) | 0 (0.00) | 0 (0.00) |
| Moderate intensity statin | 43 (22.87) | 210 (46.88) | 9 (52.94) | 0 (0.00) |
| High intensity statin | 8 (4.26) | 34 (7.59) | 0 (0.00) | 0 (0.00) |
| Ezetimibe monotherapy | 1 (0.85) | 2 (0.45) | 0 (0.00) | 0 (0.00) |
| Low intensity statin plus ezetimibe | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Moderate intensity statin plus ezetimibe | 2 (1.06) | 5 (1.12) | 0 (0.00) | 0 (0.00) |
| High intensity statin plus ezetimibe | 0 (0.00) | 2 (0.45) | 0 (0.00) | 0 (0.00) |
| Fibrates monotherapy | 0 (0.00) | 9 (2.01) | 0 (0.00) | 0 (0.00) |
| Moderate intensity statin plus fibrate | 1 (0.85) | 6 (1.34) | 0 (0.00) | 0 (0.00) |
| PCSK9 inhibitors | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| None | 128 (68.09) | 171 (38.17) | 8 (47.06) | 1 (100) |
| Total | 188 (100) | 448 (100) | 17 (100) | 1 (100) |
PCSK9: proprotein convertase subtilisin/kexin type 9.
Use of lipid-lowering treatment according to SCORE2 risk category.
| Low to moderate, n (%) | High, n (%) | Very high, n (%) | |
|---|---|---|---|
| Low intensity statin | 6 (2.35) | 7 (2.13) | 1 (1.41) |
| Moderate intensity statin | 74 (29.02) | 156 (47.56) | 32 (45.07) |
| High intensity statin | 12 (4.71) | 23 (7.01) | 7 (9.86) |
| Ezetimibe monotherapy | 3 (1.18) | 0 (0.00) | 0 (0.00) |
| Low intensity statin plus ezetimibe | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Moderate intensity statin plus ezetimibe | 2 (0.78) | 4 (1.22) | 1 (1.41) |
| High intensity statin plus ezetimibe | 1 (0.39) | 1 (0.30) | 0 (0.00) |
| Fibrates monotherapy | 1 (0.39) | 7 (2.13) | 1 (1.41) |
| Moderate intensity statin plus fibrate | 3 (1.18) | 4 (1.22) | 0 (0.00) |
| PCSK9 inhibitors | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| None | 153 (60) | 126 (38.41) | 29 (40.85) |
| Total | 255 (100) | 328 (100) | 71 (100) |
PCSK9: proprotein convertase subtilisin/kexin type 9.
Patients were studied according to the fulfillment of LDL-C goals within each risk category of SCORE (Figure 4) and SCORE2 (Figure 5). According to SCORE and SCORE2, 408 patients (62.39%) and 550 patients (84.10%) did not meet the LDL-C target, respectively. There was a significant increase in individuals failing to meet the LDL-C target when using SCORE2, compared to the use of SCORE (p<0.001).
When using the SCORE tool, among individuals categorized as low risk, 97 patients (51.60%) successfully met the LDL-C target (<115 mg/dL), while 149 patients (33.26%) in the moderate risk category achieved the target of <100 mg/dL. Nevertheless, none of the individuals classified as high risk or very high risk reached their respective targets of <70 mg/dL and <55 mg/dL, respectively. When restricting the analysis to the group of patients who met the LDL-C targets according to SCORE and switching the CV risk assessment tool to SCORE2, we observed that 49 patients (50.52%) in the low risk category and 93 patients (62.42%) in the moderate risk category failed to meet their new LDL-C target (Figure 6).
DiscussionConsidering that CVD, particularly stroke and coronary heart disease, were the leading cause of death in Portugal in 2018, effective management of CV risk factors, which contribute to the development of these diseases, becomes crucial to control these statistics.1
In the study by Csenteri et al., conducted in a high-risk country, it was estimated that 43.91% of the individuals included transitioned to a higher CV risk category when using the SCORE2 tool instead of SCORE. This significant increase indicates a substantial rise in the number of patients classified as high or very high risk.18 In specific populations, such as patients with rheumatoid arthritis and systemic lupus erythematosus from a low risk country, the use of SCORE2 for CV risk calculation identified a significantly higher proportion of patients at high or very high risk. Furthermore, SCORE2 has demonstrated the ability to predict the presence of subclinical atherosclerosis in these populations better.19,20
Our study collected data from a population of patients with hypertension eligible for CV risk estimation using SCORE2 tool, in a Portuguese (moderate risk country) primary care health unit. These patients have an established CV risk factor, which places them at an increased risk of adverse CV events13 and they regularly attend in-person appointments to monitor and control their disease, providing a crucial opportunity to manage and optimize CV risk factors. According to the most recent CVD prevention guidelines,13 we excluded patients with other comorbidities, because that would mean a direct CV risk stratification, as mentioned in the “Introduction and Methods” sections.
According to SCORE, 188 individuals (28.75%) in our population were assigned to the low risk category, with a LDL-C target of <115 mg/dL, based on the 2019 European Guidelines for the management of dyslipidaemias.16 However, with the implementation of the new SCORE2, all patients in this category were reclassified into new risk categories, requiring them to meet new targets: <100 mg/dL in 149 individuals (79.26%) and <70 mg/dL in 39 (20.74%), according to the 2021 ESC Guidelines on CVD prevention in clinical practice.13 These differences become more evident when considering the SCORE moderate and high risk categories, where most patients (n=358, 76.99%) received a higher CV risk categorization when using the SCORE2 calculator and therefore a lower LDL-C target. New and more demanding LDL-C targets can translate into the need for LLT adjustments in clinical practice.
Analysis of LDL-C target achievement revealed that 408 patients with hypertension (62.39%) in the studied health unit had LDL-C values above the recommended levels according to their SCORE category and the 2019 European Guidelines.16 Furthermore, none of the SCORE high or very high-risk patients met their therapeutic goals. These findings align with those from a Portuguese study conducted over a 20-year period, which concluded that only 7% and 3% of high risk and very high-risk patients, respectively, achieved their therapeutic LDL-C target.21 When re-estimating CV risk using SCORE2, there was a significant increase in off-target patients. In fact, when analyzing the remaining 246 patients (37.61%) who appeared to be optimized with SCORE, the results revealed that over half of them (n=142, 57.72%) did not achieve their goals with SCORE2.
Clinician- and patient-related factors can be considered to explain the number of off-target patients in this population. Clinician-related factors may include inertia in CV risk calculation, establishment of LDL-C goals and initiation or adjustment of appropriate LLT; beyond that, clinical reasoning may prioritize other factors, resulting in a perceived lack of significant benefit in initiating or changing therapy, such as the socioeconomic context or when the patient's LDL-C value was close to target. This is reflected by the fact that approximately 47% of individuals belonging to SCORE high risk and 40% to SCORE2 high and very high-risk categories (8 and 38 patients, respectively) were not using any LLT at all. Patient-related factors may involve non-compliance with therapeutic regimens and/or lifestyle measures that should be privileged; medication costs; possible contraindications or adverse effects and refractory to lifestyle measures and/or already optimized therapy. Patient health literacy education is fundamental to improve these results. It is also important to note that our analysis period reflects a post-pandemic season.
Our findings strengthen the importance of CV risk assessment using the SCORE2 algorithm and the need to share this new tool among clinicians, particularly GPs, who play a central role in health promotion, prevention and early detection of CVD. It is essential to improve and tailor the medical information systems to current clinical recommendations. To support this need, we found that in our population only 23 patients (3.5%) had their CV risk assessment estimated by SCORE2 registered on the appointment record system. Hence, updating the already incorporated SCORE tool on primary clinical record system SClínico™ (used in Portugal) to the SCORE2 calculator would be an important step toward improving these results. It is crucial to acknowledge that although SCORE2 is an important tool, therapeutic optimization should be guided by an assessment of individual risk–benefit profiles, particularly in an aging and/or vulnerable population.
The strengths of our study lie in its originality, relevance and topicality. Our results demonstrate that the recent SCORE2 tool could have a great impact on clinical practice and potentially on morbimortality outcomes. Additionally, we conducted the study on an entire population of patient with hypertension from a primary care health unit in whom SCORE2 could be applied.
We also recognize certain limitations, such as the exclusion of 523 individuals (29.97%) from our initial population due to the lack of an appointment or lipid profile within the established period. This could introduce a bias by overrepresenting older patients and those with more comorbidities, although all of them were summoned for an appointment. In addition, several investigators were involved in data collection, and we cannot exclude the possibility of errors or omissions in clinical records, as well as potential sphygmomanometer calibration errors, non-optimal conditions for blood pressure measurement and discrepancies in laboratory procedures or errors.
Overall, this study contributes to the growing body of evidence supporting the value of the SCORE2 algorithm in CV risk assessment. It underscores the need for wider adoption of this tool among healthcare professionals, particularly family physicians, and emphasizes the importance of continuous improvement in risk management strategies. To date, there are some studies similar to ours; however, none of them study a population from a moderate risk country.
ConclusionThe use of the new SCORE2 algorithm allows patients to be reclassified into three rather than four categories and establishes new LDL-C targets. In this study, changing the CV risk assessment tool from SCORE to SCORE2 resulted in a significant increase in the number of patients with hypertension failing to meet their LDL-C target. Therefore, SCORE2 should be a part of the evaluation and management of these patients, since its use has implications for clinical decision-making in daily practice, guiding the need for therapeutic adjustments.
Our study reflects the reality of one primary health unit from a moderate risk country, and uncomplicated patients with hypertension aged between 40 and 69 years, so these results cannot be extrapolated to other realities. Further studies, including different types of patients, including those who do not have hypertension, and involving other health units in Portugal and other countries, are needed to provide a more comprehensive understanding of the subject matter.
Conflict of interestsThe authors have no competing interests to declare.