Heart failure with reduced ejection fraction (HFrEF) poses a significant challenge to healthcare. While clinical trials have shown the therapeutic benefits of dapagliflozin in patients with HFrEF, it is essential to understand treatment patterns and patient characteristics in real-world settings. The EVOLUTION-HF study sought to address this gap by analyzing real-world data.
MethodsEVOLUTION-HF is a retrospective cohort study conducted at eight sites in Portugal, which included patients who began treatment with dapagliflozin for HFrEF. Medical records were reviewed to collect information on the initiation date of dapagliflozin (the index date) and at the six- and 12-month follow-ups.
ResultsThis study included 228 patients. The majority were male, with an average age of 65 years, a mean left ventricular ejection fraction of 29%, and 85% classified as NYHA class II. More prevalent comorbidities were dyslipidemia (59%) and arterial hypertension (56%). On the index date, baseline medications showed a high utilization of standard HFrEF therapies: 92% of patients received betablockers, 71% were on aldosterone antagonists, and 55% were taking angiotensin receptor-neprilysin inhibitors. At the end of the follow-up period, there was a significant increase in the dosage of beta-blockers and a decrease in the dosage of loop diuretics. A low discontinuation rate of 5% was observed for dapagliflozin.
ConclusionsThese findings support the established safety profile of dapagliflozin. The patient characteristics in the EVOLUTION-HF study closely resemble those in the DAPA-HF randomized trial. The observed treatment patterns indicate an optimization in guideline-directed medical therapy.
A insuficiência cardíaca com fração de ejeção reduzida (ICFEr) representa um desafio para os cuidados de saúde. Após a demonstração do valor terapêutico da dapagliflozina na ICFEr através dos ensaios clínicos, é essencial compreender os padrões de tratamento e as características dos doentes num contexto de prática clínica. O estudo EVOLUTION-HF pretende colmatar esta lacuna através da análise de dados do mundo real.
MétodosEstudo de coorte retrospetivo, realizado em oito centros portugueses, que incluiu doentes que iniciaram o tratamento com dapagliflozina para a ICFEr. Através da revisão de registos clínicos, foi recolhida informação na data de início da dapagliflozina (index date) e após 6 e 12 meses.
ResultadosForam incluídos 228 doentes, maioritariamente do sexo masculino, com fração de ejeção do ventrículo esquerdo média de 29% e 85% em classe NYHA II. As comorbilidades mais prevalentes foram a dislipidemia (59%) e a hipertensão arterial (56%). Na index date, observou-se uma elevada utilização de terapêutica recomendada para a ICFEr: 92% de bloqueadores beta (BB), 71% de antagonistas da aldosterona e 55% de antagonista do recetor da angiotensina-inibidor da neprilisina. No final do seguimento, registou-se um aumento da dosagem de BB e uma diminuição da dosagem de diuréticos de ansa. A taxa de descontinuação de dapagliflozina foi de 5%.
ConclusõesOs resultados sustentam o já estabelecido perfil de segurança da dapagliflozina. As características dos doentes no estudo EVOLUTION-HF assemelham-se às do ensaio clínico DAPA-HF. Os padrões de tratamento observados realçam a otimização da Terapêutica Médica Recomendada.
Heart failure (HF) is a chronic condition that poses a significant challenge for healthcare.1 In developed countries, the prevalence of HF is estimated to be between 1% and 2% of the general adult population.2 Studies conducted in the Portuguese population indicate a higher prevalence. EPICA,3 a community-based epidemiological study conducted over 25 years ago with subjects over 25 years attending primary care units, estimated an overall prevalence of HF of 4.36%. Recently, the PORTHOS4 study showed an overall estimated HF prevalence of 16.54% in community-dwelling individuals aged 50 years or older. In both studies, HF with preserved ejection fraction (HFpEF) was the most common HF phenotype, while HF with reduced and mildly reduced ejection fraction (HFrEF) estimated prevalence was 1.3% in both EPICA (ejection fraction <45%) and PORTHOS (ejection fraction <50%). The estimated prevalence of HFrEF in the PORTHOS study was 0.35%. Although the increase in overall HF prevalence is driven by HFpEF, managing HFrEF continues to pose significant challenges.5
The health costs of HF are expected to increase in the coming years.6–8 Gouveia et al. estimated that, in 2014, HF direct costs (hospitalizations, medications, diagnostic and therapeutic procedures, medical appointments, and emergency and long-term care) in Portugal amounted to €299 million, with indirect costs (employment-related) totaling €106 million.9 By 2036, total costs were projected to rise from €405 million to €503 million.8
Both cardiac and non-cardiac comorbidities are prevalent among patients with HF. HFrEF presents a grim outlook as patients are at a high risk of disease progression, worsening symptoms, hospitalization, and death.10 Despite advancements in HF treatments, mortality remains high. The European Society of Cardiology (ESC) Heart Failure Long-Term Registry reports 1-year mortality of 23% for acute HF and 6% for chronic HF.11 Furthermore, patients with HF experience a variety of symptoms that significantly impair their quality of life and daily activities.12
Sodium-glucose co-transporter 2 inhibitors (SGLT2i) were initially developed to treat type 2 diabetes mellitus (T2DM). However, during clinical trials, researchers observed a significant reduction in HF hospitalizations among patients with T2DM taking SGLT2i.13 The Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF) study then evaluated the efficacy and safety of dapagliflozin in patients with HFrEF regardless of the presence of T2DM. Notably, dapagliflozin was well-tolerated, with no significant difference in safety events compared to placebo.10 Beyond its impact on mortality and hospitalization, dapagliflozin also improved symptoms, physical function, and quality of life on top of optimization of HF treatment.10,14 Based on the robust efficacy and safety profile demonstrated in DAPA-HF,10 dapagliflozin was recommended to reduce mortality and morbidity in HFrEF patients.15
However, like most clinical trials, the DAPA-HF study had specific eligibility criteria, which limits its external validity for a broader population. Therefore, it was important to explore real-world data (RWD), to analyze the population under dapagliflozin treatment for HFrEF in a real-world clinical setting.10
ObjectivesEVOLUTION-HF sought to characterize patients who initiated dapagliflozin for HFrEF treatment and to provide early insights regarding real-world dapagliflozin treatment patterns.
MethodsStudy design and populationThis retrospective cohort study was conducted in the cardiology department of eight Portuguese sites which have expertise in HFrEF management and diversely distributed from north to south of the country. The study analyzed data from electronic medical records of adult patients who had previously been diagnosed with HFrEF, defined by a documented left ventricular ejection fraction (LVEF) of ≤40% and confirmed through the physician's clinical judgment. The analysis focused on patients who initiated dapagliflozin for HFrEF between 1 March 2021 and the 31 October 2021; it included outpatients and inpatients. Patients were enrolled at least 30 days following initiation of dapagliflozin. Clinical assessments and supporting laboratory data (e.g., NT-proBNP levels) were also considered as part of routine diagnostic evaluations.
Patients with prior SGLT2i treatment, those who received dapagliflozin for reasons outside the approved HFrEF indication in Portugal, and those diagnosed with type 1 diabetes before enrollment were excluded. Data analysis occurred at three different time points: baseline, six-months (6M), and 12-months (12M) follow-up visits, aligning with routine clinical visits. The study received favorable ethical approval from each site's committee, including approval for a waiver of informed consent since only secondary data were used.
Data collectionThe variables collected included demographics, present illness, past medical history, medication and devices, physical examination, symptoms, electrocardiogram (ECG), and laboratory and imaging tests.
StatisticsA descriptive analysis of the patients was conducted using the statistical software R. The descriptive categorical variables are described using the number of observations (n), number and percentage (%) within each category, number of missing observations, and 95% confidence intervals (Clopper–Pearson method). Numeric variables are described using the number of observations (n), mean and standard deviation, minimum, maximum, median, and interquartile range, number of missing observations, and 95% confidence intervals. A Cox proportional hazards model was planned to evaluate the association between defined baseline characteristics, such as sex, age, NYHA class, and LVEF, and (1) dapagliflozin discontinuation and (2) compliance with other HF medication.
ResultsSociodemographic characteristicsA total of 231 patients were included from November 2022 to 2023. After excluding three individuals (two with prior SGLT1i treatment, and one for having ejection fraction ≥40%), data from 228 participants were included in this analysis.
The baseline characteristics measured at the time patients began dapagliflozin treatment (index date) showed that the population was predominantly male (72.8%) with a mean age of 64.7 years (±standard deviation [SD] 13.0). Table 1 provides a detailed overview of the sociodemographic and disease characteristics.
Sociodemographic and disease characteristics at index date.
| Characteristic | Value | na |
|---|---|---|
| Age, years, mean (SD) | 64.7±13.0 | 228 |
| Male sex, n (%) | 166 (72.8) | 228 |
| BMI, kg/m2, mean (SD) | 27.7±5.3 | 206 |
| Systolic BP, mmHg, mean (SD) | 120.4±20.1 | 223 |
| Diastolic BP, mmHg, mean (SD) | 70.0±12.3 | 222 |
| Heart rate, bpm, mean (SD) | 68.3±12.7 | 218 |
| Laboratory values | ||
| eGFR, mL/min/1.73 m2, mean (SD)b | 76.5±24.9 | 215 |
| NT-proBNP, pg/mL, median (IQR) | 920.0 (1616.5) | 192 |
| Clinical features of HF | ||
| LVEF, %, mean (SD) | 29.1±6.6 | 228 |
| Ischemic cause, n (%) | 96 (42.1) | |
| Non-ischemic cause, n (%) | 124 (54.4) | |
| Unknown cause, n (%) | 8 (3.5) | |
| Previous HF hospitalization, n (%) | 40 (17.5) | |
| NYHA class, n (%) | ||
| II | 192 (84.2) | 228 |
| III | 32 (14.0) | |
| IV | 3 (1.3) | |
| Unknown | 1 (0.4) | |
| Medical history – conditions | ||
| Dyslipidemia, n (%) | 135 (59.2) | 228 |
| Hypertension, n (%) | 128 (56.1) | |
| Atrial fibrillation, n (%) | 61 (26.8) | |
| Myocardial infarction, n (%) | 58 (25.4) | |
| T2DM, n (%) | 44 (19.3) | |
| Heart valve regurgitation/stenosis, n (%) | 26 (11.4) | |
| CKD, n (%) | 19 (8.3) | |
| Medical history – devices/interventions | ||
| ICD, n (%) | 68 (29.8) | 228 |
| Coronary revascularization, n (%) | 44 (19.3) | |
| CRT, n (%) | 24 (10.5) | |
| Pacemaker, n (%) | 8 (3.5) | |
BMI: body mass index; BP: blood pressure; bpm: beats per minute; CKD: chronic kidney disease; CRT: cardiac resynchronization therapy; eGFR: estimated glomerular filtration rate; HF: heart failure; ICD: implantable cardioverter-defibrillator; IQR: interquartile range; LVEF: left ventricular ejection fraction; NT-proBNP: N-terminal pro-hormone BNP; NYHA: New York Heart Association; SD: standard deviation; T2DM: type 2 diabetes mellitus.
Since this is a retrospective observational study, not all variables were available for the 228 participants. Therefore, the column “n” shows exactly how many results we were able to obtain for each characteristic. In grey, we highlighted the characteristics where we could not collect information for all (n=228) participants.
The majority of participants (54.4%) had non-ischemic HF, 84.2% were in NYHA class II, with mean (SD) LVEF of 29.1 (6.6) %, and mean (SD) eGFR of 76.5 (24.9) mL/min/1.73 m2. In terms of prior hospitalizations, 17.5% of patients had been hospitalized for heart failure (HF) within the past year. The median time since their last hospitalization to the initiation of dapagliflozin was 3.0 months, with an interquartile range of 5.2 months.
We further analyzed the available ECG results from patients before they started dapagliflozin (n=191), and 24.1% of them were not in sinus rhythm. Among these abnormalities, atrial fibrillation was the most common, occurring in 84.8% of cases. Atrial flutter (8.7%), atrial tachycardia (2.2%), and other unspecified arrhythmias (4.3%) were also noted. The available ECGs revealed abnormalities in 93.7% of patients, including non-specific repolarization changes in 21.2% of cases and complete left bundle branch blocks in 14.0% of cases.
Medical conditionsDyslipidemia and hypertension were the most prevalent comorbidities, affecting 59.2% and 56.1% of patients, respectively. Additionally, 26.8% had atrial fibrillation, 19.3% had type 2 diabetes, and 8.3% had chronic kidney disease (CKD). Regarding interventions and/or devices, implantable cardioverter-defibrillators were placed in 29.8% of patients, 19.3% had undergone coronary revascularization, and 10.5% had cardiac resynchronization therapy.
Study outcomesDapagliflozin discontinuationThe study revealed a very high rate of treatment compliance throughout the 12-month follow-up period. Only a small proportion of patients (5%) discontinued dapagliflozin, with most discontinuations occurring in the first six months of treatment (Figure 1).
The reasons for dapagliflozin discontinuation included adverse drug reaction/adverse event (n=5), poor/non-adherence (n=2), switch to other SGLT2i (n=2), other (n=2), and unknown reasons (n=1).
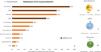
Cardiovascular medications at index date and changes after dapagliflozin initiationThe most commonly used CV medication classes at index date were betablockers (92%), aldosterone receptor antagonists (MRAs) (71%), loop diuretics (71%), and angiotensin receptor-neprilysin inhibitors (ARNIs) (55%) (Figure 2A). Specific medications within each class are described in Figure 2B–D.
Distribution of cardiovascular medications at index date. (A) Percentage of participants under each medication. (B) Distribution within the beta-blockers class. (C) Distributions within the aldosterone receptor antagonists (MRA) class. (D) Distribution within the diuretics class. ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; ARNI: angiotensin receptor-neprilysin inhibitor; CV: cardiovascular; GDMTs: guideline-directed medical therapy according to 2021 ESC HF Guidelines; MRA: aldosterone receptor antagonists; n: number of participants.
The most frequent changes in medication after the start of dapagliflozin treatment involved betablockers, loop diuretics and ARNIs. There were 44 increases in beta-blocker dosages, 40 decreases in loop diuretics dosages, and 34 increases in ARNIs dosages. Angiotensin-converting enzyme inhibitors (ACEi) were the most often discontinued medication class (Figure 3).
Changes in cardiovascular medications for HFrEF during the 12-month follow-up period (These numbers refer to the number of changes, not changes per patient. This means that when there are 44 dose increases in beta-blockers, for example, there may have been 2 increases in one patient. It does not mean that 44 participants had changes. What we do know is the number of beta blockers that existed at baseline (n=160), and we know that there were 44 increases.) ACE: angiotensin-converting enzyme; ARNI: angiotensin receptor-neprilysin inhibitor; CV: cardiovascular; HFrEF: heart failure with reduced ejection fraction; MRA: aldosterone receptor antagonists.
A total of 40 patients were taking glucose-lowering agents at index date. Of these, metformin was the most common medication (75.0%), while 32.5% were taking dipeptidyl peptidase 4 inhibitors (DPP-4i), 15.0% were taking insulin and sulphonylureas, and 5.0% were taking glucagon-like peptide-1 receptor agonists (GLP1-RA).
Over the 12-month follow-up period, changes in glucose-lowering medications were not significant, with three patients discontinuing metformin.
DiscussionThe EVOLUTION-HF study aimed to characterize patients with HFrEF who initiated treatment with dapagliflozin in a real-world setting in Portugal. Our findings indicate that the majority of patients in our study are young males who exhibit mild HF symptoms, with dyslipidemia (59%) and hypertension (56%) being the most prevalent comorbidities. The results indicate a high utilization of guideline directed medical therapy (GDMT) for HFrEF at baseline: 92% received betablockers, 71% were on MRAs, and 55% on ARNIs. Most patients (95%) adhered to dapagliflozin treatment, and there was an increase in the prescription and/or dosage adjustment of beta-blockers, mineralocorticoid receptor antagonists (MRAs), and angiotensin receptor-neprilysin inhibitors (ARNI). In contrast, loop diuretics and ACE inhibitors were reduced or discontinued during the 12-month period. This is the first study, to our knowledge, that characterizes a real-world cohort of HFrEF patients treated with dapagliflozin across various regions of Portugal.
The high adherence to dapagliflozin suggests that it is well tolerated; in fact, only 2% of those who stopped taking the medication did so due to adverse events. We were unable to carry out the planned analysis of the factors influencing the discontinuation of dapagliflozin due to the small number of cases.
Compared to contemporary trials including HFrEF patients, the cohort from EVOLUTION-HF presented a high level of GDMT use at index date, according to the 2021 ESC HF Guidelines.16 Data from Registries show a much lower level of HF GDMT implementation.17,18
By comparing clinical characteristics and treatment patterns of patients included in the DAPA-HF randomized trial10 and the EVOLUTION-HF study, similar characteristics in terms of age, sex, mean LVEF, and baseline eGFR were observed. Notwithstanding, it is worth mentioning that patients in the EVOLUTION-HF study tend to have a higher percentage of NYHA II (85% vs 68%) and lower median NT-proBNP value (920 vs. 1428 pg/mL) in comparison with DAPA-HF. Additionally, lower comorbidities in this study when comparing to DAPA-HF, such as CKD (8% vs 41%, respectively), might reflect a tendency to initiate dapagliflozin in patients with less burden of comorbidities, as these were the first subset of HF patients being treated with the drug. Regarding treatment patterns, the EVOLUTION-HF study showed a tendency for higher use of ARNI and lower use of diuretics at the index date. These differences can be attributed to the time elapsed between the DAPA-HF read-out date (March 2019), the update of HF guidelines,16 and inclusion of patients in EVOLUTION-HF. This indicates the gradual integration of evidence and updated guidelines into clinical practice, particularly concerning the use of ARNI.
The higher level of prescription and/or up-titration of betablockers, MRAs, and ARNI after dapagliflozin initiation, while loop diuretics and ACE inhibitors were down-titrated/withdrawn, aligns with findings from other studies suggesting that dapagliflozin initiation may facilitate a better optimization of GDMT.18,19 One of the reasons for such an effect might be that dapagliflozin is associated with a lower risk of hyperkalemia, an adverse event responsible for the down-titration/discontinuation of MRA or ARNIs. Moreover, we can argue that dapagliflozin's effect on the cardiac cell19,20 allows for a more favorable cardiac environment which might grant the opportunity for enhanced therapeutic benefits, although further randomized research is warranted. It is also important to note that the 2021 ESC HF Guidelines16 advise for a more aggressive treatment regimen, where the four pillars of GDMT (iECA/ARA or ARNI, betablockers, MRA, and SGLT2) should be introduced as soon as possible – EVOLUTION-HF's results might again be reflecting the gradual integration of said guidelines into clinical practice throughout the duration of the study.
This study has some limitations. It is important to acknowledge the site selection bias, since participating sites were chosen for their expertise in HFrEF management and are not representative of HF clinical practice in Portugal. Nevertheless, it was not an aim of the EVOLUTION-HF study to fully capture the Portuguese clinical practice, but to analyze the first real-world experiences of dapagliflozin use in this new setting of patients. Since the study relied on existing medical records, data collection was limited by the information documented for each patient. Another relevant aspect to consider is that real-world HFrEF populations may differ depending on the clinical setting in which they are managed. While our study was conducted exclusively in Cardiology departments and ambulatory patients, other settings, such as Internal Medicine departments, might exhibit different patients’ baseline characteristics, comorbidity burdens, and treatment patterns. Although our study was not designed to capture these broader patient groups, future research including more diverse clinical settings could provide further insights into the generalizability of our findings across different real-world HFrEF populations.
There are important strengths to acknowledge as well. While not representative of all Portuguese HF care, this is a multicentric study and patients were recruited from distinct geographic locations (north to south) and various hospital settings (university to regional hospitals). Finally, this Portuguese EVOLUTION-HF cohort will be integrated with a multicountry study. By combining data across countries, researchers can gain a clearer understanding of global treatment patterns and clinical characteristics of HFrEF patients receiving dapagliflozin in real-world practice.
ConclusionThe results of this study confirm, in a real-world setting, the favorable safety profile of dapagliflozin that was previously reported in clinical trials, with the therapeutic levels of dapagliflozin maintained in 95% of patients. Despite a high use of HF GDMT at baseline, an increase in prescriptions and/or up-titration for betablockers, MRAs, and ARNIs was observed, alongside a decrease in the use of loop diuretics and ACEi throughout the study.
Central figureCentral picture legend: Intake of HFrEF medications throughout the study. (A) At index date. (B) Changes at follow-up (These numbers refer to the number of changes, not changes per patient. This means that when there are 44 dose increases in beta-blockers, for example, there may have been 2 increases in one patient. It does not mean that 44 participants had changes. What we do know is the number of beta blockers that existed at baseline (n=160), and we know that there were 44 increases.) ACE: angiotensin-converting enzyme; ARB: angiotensin; ARNI: angiotensin receptor-neprilysin inhibitor; CV: cardiovascular; HRrEF: heart failure with reduced ejection fraction; MRA: aldosterone antagonist.
Central message: Despite the high use of GDMT at dapagliflozin initiation, an optimization of HFrEF therapy was observed during the 12-month follow-up period.
Conflicts of interestThere are the following conflicts of interest to consider, although without influence to the content of the work: A.A. has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Bial and AstraZeneca, support for attending meetings and/or travel from Amgen, Bial, Boehringer-Ingelheim, Novartis, and Pfizer. A.T.T. was Vice-President of the Portuguese Society of Cardiology between 04-2021 and 04-2023, and Board Member of the European Association of Cardiovascular Imaging from 12/2024 to the present. S.G. has received payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing or educational events from Bial and AstraZeneca, and support for attending meetings and/or travel from Boehringer-Ingelheim and Novartis. M.P., M.A., M.L. and F.B. are AstraZeneca Portugal employees. A.B., A.O.S., F.F., J.S.C., and O.S., have no conflicts of interest to declare.
The authors would like the thank all the sites and study team members who participated in the EVOLUTION-HF Retrospective study and contributed to the collection of data here presented, namely Prof. Alexandra Sousa, Dr. Ana Neto, Dr. Ana Rita Almeida, Nurse Ana Rita Sousa, Nurse Andreia Soares, Dr. António Gonçalves, Dr. Bárbara Ferreira, Dr. Carlos Xavier Resende, Dr. Carolina Lourenço, Dr. Catarina Carvalho, Dr. Cátia Ferreira, Nurse Crisálida Jesus, Dr. David Roque, Nurse Dina Batista, Dr. Diogo Cunha, Prof. Elisabete Martins, Prof. Emília Moreira, Nurse Filipa Silva, Dr. Hugo Antunes, Dr. Hugo Viegas, Dr. Inês Almeida, Dr. Inês Campos, Dr. Inês Fialho, Nurse Mafalda Selas, Prof. Manuel Campelo, Nurse Manuela Fonseca, Dr. Margarida Madeira, Dr. Marta Bernardo, Dr. Marta Braga, Nurse Patrícia Silva, Dr. Paulo Araújo, Dr. Pedro Carreira, Dr. Pedro Carvalho, Dr. Rita Moreira, Dr. Roberto Pinto, Prof. Sandra Amorim, Dr. Susana Costa, Dr. Tatiana Duarte, and Prof. Tiago Silva. The authors would like to acknowledge the CRO CETERA team (Francisca Patuleia Figueiras, Susana Silva, Beatriz Ricardo, Margarida Nogueira) for the implementation and management of the study in Portugal, and their medical writing contribution to this article.