Abnormal vascular connections to the right ventricle (RV) are rare congenital malformations. The majority of cases are diagnosed incidentally, and most patients are asymptomatic. The authors present three cases of right ventricular fistulae of non-coronary origin.
Case 1A 2-year-old asymptomatic boy with a heart murmur underwent an echocardiogram which showed turbulent flow in the subaortic region. He was catheterized and the aortic angiogram revealed a hemodynamically insignificant fistulous tract between the right sinus of Valsalva and the RV (Figure 1).
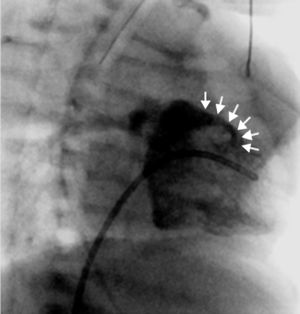
Case 2A 3-year-old asymptomatic boy was referred due to a murmur suggestive of a ventricular septal defect. In the echocardiogram, a turbulent flow was evident in the proximal ascending aorta, as well as in the right ventricular wall. In order to clarify the morphology of this apparent fistulous tract, he underwent a cardiac computerized tomography scan, which confirmed the presence of a fistula between the ascending aorta and the RV (Figure 2).
Case 3A 19-day-old baby boy was admitted to a Pediatric Intensive Care Unit following cardiorespiratory arrest of unknown cause. Cardiac catheterization to rule out anomalous coronary artery anatomy was performed and the right ventricular angiogram revealed a fistulous tract between the RV and the pulmonary artery (Figure 3).
ConclusionsThe majority of congenital fistulae to the RV originate in the coronary artery bed. Other sites of origin, such as those demonstrated in these cases, are exceedingly rare. To the best of our knowledge, few have been reported during infancy. As these fistulae were found accidentally, we opted for a conservative approach.
Conflicts of interestThe authors have no conflicts of interest to declare.