Pulmonary sequestration is a rare disease consisting of a non-functioning bronchopulmonary mass separated from the tracheobronchial tree, supplied from a systemic artery.
A 20-year-old primigravida was referred to the fetal cardiology clinic at 22 weeks’ gestation due to an intrapulmonary mass suggestive of pulmonary sequestration. The fetal echocardiogram showed a structurally normal heart and a tortuous feeding vessel arising from the abdominal aorta, proximally to the celiac trunk (Figure 1). She maintained regular follow-up, during which time the intrapulmonary mass gradually decreased in size and the collateral artery disappeared.
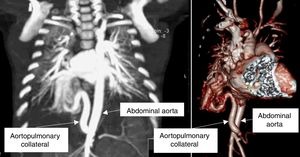
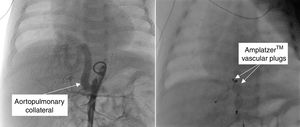
A 1.5-month-old infant was referred for a paediatric cardiology review due to poor weight gain and breathlessness. On examination, he had increased work of breathing and a gallop rhythm. The transthoracic echocardiogram showed dilatation of the left atrium and ventricle, and no intracardiac shunts. Chest computed tomography showed a large aortopulmonary collateral artery originating in the abdominal aorta (Figure 2), irrigating a small portion of the right lower lobe. He underwent transcatheter embolization of the collateral artery (Figure 3) and is now 12 months old and asymptomatic.
These are two cases of pulmonary sequestration with different presentations, outcomes and treatment. In the first case, the diagnosis was made antenatally and the feeding vessel disappeared spontaneously. The second case initially presented with heart failure and required interventional closure of the aortopulmonary collateral.
Most pulmonary sequestrations regress spontaneously in utero. When this does not occur, the child may develop symptoms and transcatheter embolization can be a successful alternative to surgery in selected cases.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank Mr. Adam Cockle for helping with the patient consent for the uses of images in medical research.