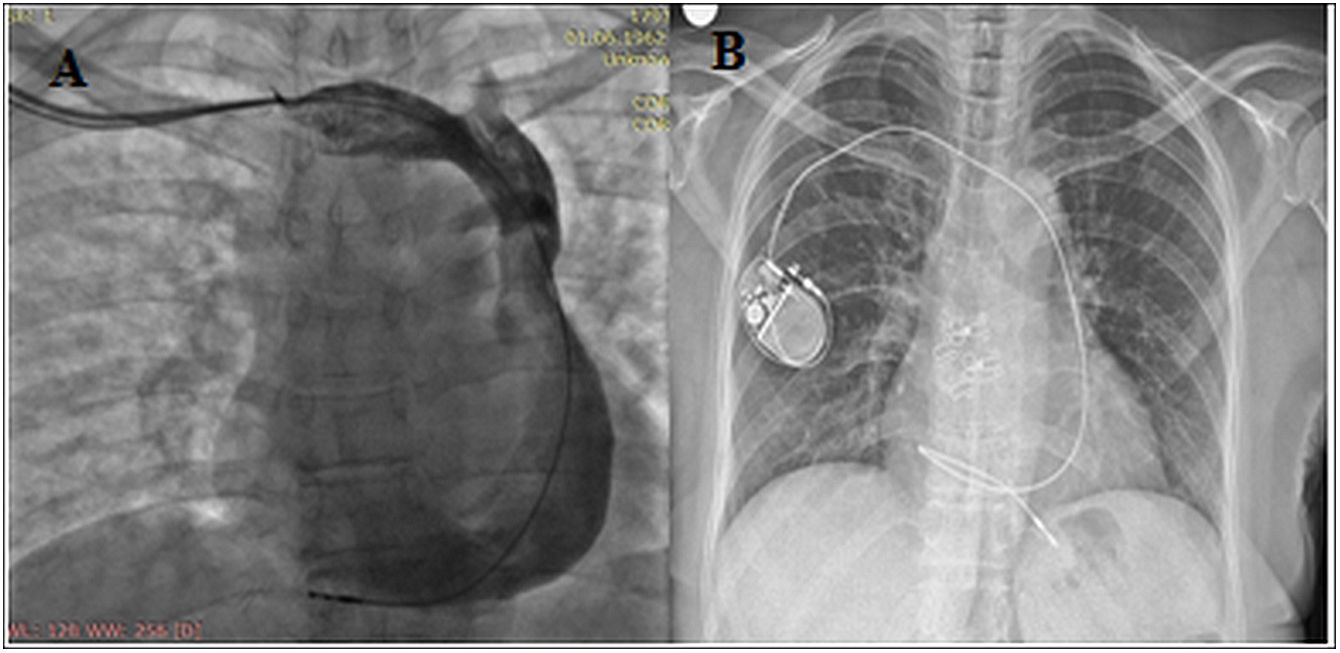
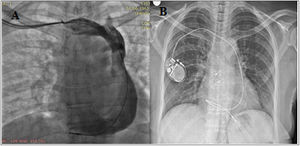
A 58-year-old female patient was admitted to our hospital with dizziness and near syncope. The diagnosis of Mobitz type 2 atrioventricular block was made on electrocardiogram. A dual-chamber pacemaker was inserted through the right side as the patient actively used her left arm. The right ventricular (RV) lead was advanced in an attempt to access the right superior vena cava (SVC), but resistance was encountered. Venography revealed persistent left superior vena cava (PLSVC) draining through the dilated coronary sinus (CS) into the right atrium with absent right SVC (Figure 1A). Then, a classic lead delivery system was used to reach the right atrium through CS and then through the tricuspid valve into the right ventricle. The RV lead was advanced via PLSVC through the CS and was actively fixed to the right ventricle apex with loop configuration. Following RV lead placement, an atrial active fixation lead was introduced, however we were unable to implant a pacemaker lead in a proper location. The parameters of the implanted VVIR pacemaker were ventricular sensing of 6 mV, pacing threshold of 0.4 V, and impedance of 630 ohms. Chest X-ray revealed satisfactory positioning of the ventricular lead (Figure 1B).
While implanting cardiac devices in patients with PLSVC and absent right SVC, it is difficult to pass through the tricuspid valve to place the ventricular lead. Although lead implantation is very challenging due to abnormal vena cava anatomy, different techniques can be used to facilitate the crossing tricuspid valve. Physicians should be aware of the use of active fixation leads, and conforming the loop configuration of the ventricular lead may overcome this technical challenge.
Conflict of interestsNo potential conflict of interest was reported by the author(s).