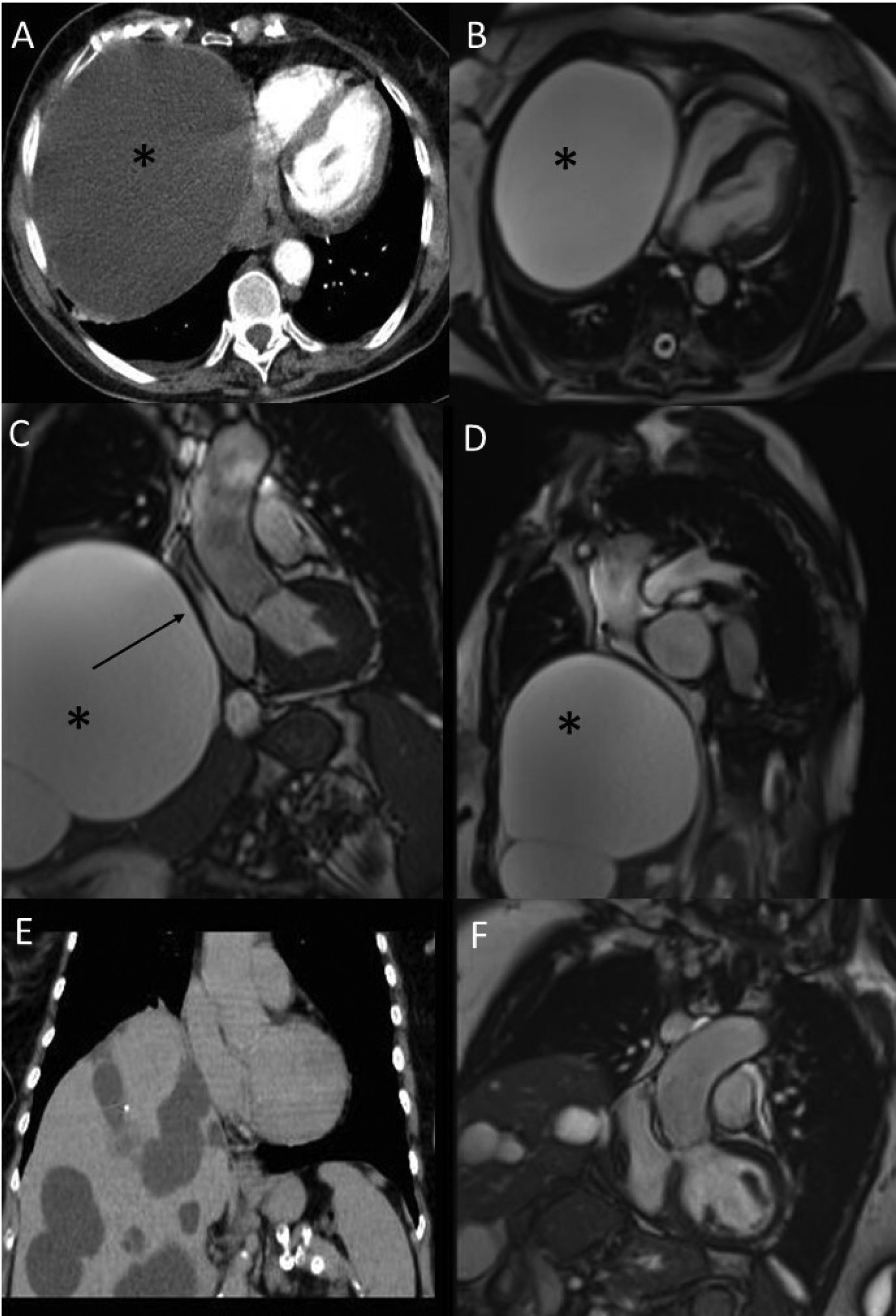
A 79-year-old woman with type II diabetic and history of multiple liver cysts was admitted to the emergency room for syncope. On physical examination a loud diastolic murmur at cardiac apex, hypotension (80/50 mmHg) and peripheral oxygen saturation of 93% were found. An electrocardiogram depicted sinus tachycardia and diffuse repolarization abnormality. The laboratory reported high levels of cardiac troponin T and brain natriuretic peptide. With a high suspicion of acute pulmonary embolism, a computed tomographic pulmonary angiography was performed. There was not any evidence of embolism, however, a giant cyst in the cranial right lobe of the liver with an axial diameter of 15 × 14 cm and a craniocaudal extension up to 13 cm with compression of the right heart was detected (Figure 1A). A cardiovascular magnetic resonance (CMR) with gadolinium revealed in balanced turbo field-echo sequences a giant cyst compressed the right atrium and the inferior vena cava with a normal biventricular function (Figure 1B–D). Finally, a laparoscopic surgical resection was decided upon by the heart team (Figure 1E and 1F) and the pathology examination confirmed a simple liver cyst. The procedure was successful, and the patient was relieved of her symptoms and is doing well to date.
(A) Axial thoracic computed tomography showing a giant cyst (*) compressing the right heart. (B) Four-chamber view, balanced turbo field-echo (BTFE) cardiovascular magnetic resonance (CMR) showing a giant cyst (*) compressing the right heart. (C) Left ventricular tract outflow (LVOT) view, BTFE CMR showing a giant cyst (*) compressing the right atrium (black arrow). (D) BTFE CMR sagittal view of the cyst extension. (E) Coronal thoracic computed tomography after the cyst resection. (F) BTFE CMR showing the LVOT view after the cyst resection.
The authors have no conflicts of interest to declare.