Pheochromocytoma is a rare catecholamine-producing tumor, discovered incidentally in 50% of cases. We present the case of a 44-year-old male with a history of paroxysmal palpitations. Baseline ECG, transthoracic echocardiogram and ECG stress test showed no relevant alterations. Paroxysmal atrial fibrillation was detected on 24-hour Holter ECG. After antiarrhythmic therapy, the patient remained symptomatic, and was accordingly referred for electrophysiological study and atrial fibrillation ablation. Anticoagulation was initiated before the procedure. After ablation and still anticoagulated, he complained of hematospermia. The abdominal and pelvic imaging study showed a 10-cm left adrenal mass, predominantly cystic, compatible with pheochromocytoma, which was confirmed after biochemical tests (increased urine metanephrines and plasma catecholamines). Metaiodobenzylguanidine scintigraphy scanning confirmed localized disease in the adrenal gland, excluding other uptake foci. Following appropriate preoperative management, surgical resection of the giant mass was performed successfully and without complications.
O feocromocitoma é um tumor raro produtor de catecolaminas, que se descobre incidentalmente em 50% dos casos. Os autores apresentam o caso clínico de um homem de 44 anos de idade, com história de palpitações paroxísticas. O ECG basal, o ecocardiograma transtorácico e a prova de esforço não demonstraram alterações de relevo. O Holter de 24 h revelou fibrilhação auricular paroxística. Após terapêutica antiarrítmica, o doente manteve-se sintomático, pelo que foi orientado para estudo eletrofisiológico e ablação da fibrilhação auricular, tendo iniciado hipocoagulação oral pré-procedimento. No período pós-ablação, ainda hipocoagulado, referiu hematoespermia. O estudo imagiológico abdomino-pélvico revelou uma massa de 10 cm na glândula suprarrenal esquerda, predominantemente cística, compatível com feocromocitoma, diagnóstico que foi confirmado após testes bioquímicos (elevação das metanefrinas urinárias e das catecolaminas plasmáticas). A cintigrafia corporal com metaiodobenzilguanidina confirmou doença localizada na glândula suprarrenal, excluindo outros focos de captação. Após preparação pré-operatória adequada, procedeu-se à resseção cirúrgica da massa gigante com sucesso e sem complicações.
Pheochromocytoma is a rare catecholamine-producing tumor, with an incidence of 2–8 cases per million per year,1 occurring in about 0.5% of patients with hypertension and suggestive symptoms.2 Typical symptoms include paroxysmal hypertension, pounding headache, palpitations, diaphoresis and pallor.3 The diagnosis is based on biochemical tests, with demonstration of catecholamine oversecretion by adrenal chromaffin cells, and imaging studies, which localize the tumor and guide surgical resection.1,3 Half of all pheochromocytomas are discovered incidentally.4 Cardiovascular complications include myocardial hypertrophy, heart failure, myocardial infarction and various arrhythmias, of which atrial fibrillation is one of the most common.5–7
We report a case of a giant pheochromocytoma diagnosed after imaging study for hematospermia subsequent to oral anticoagulation for an atrial fibrillation ablation procedure.
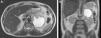
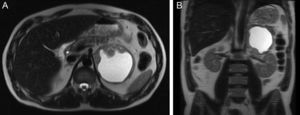
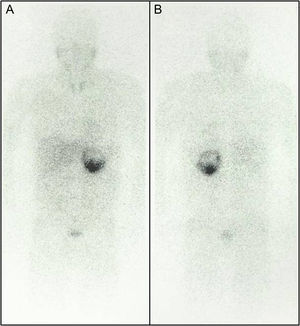
Case reportA 44-year-old man with a history of tobacco use was referred for cardiological assessment in July 2009 due to a three-year history of paroxysmal palpitations lasting about five minutes, which were associated with a throbbing feeling in the head. No other accompanying symptoms were reported. Physical examination, blood pressure (110/70 mmHg), 12-lead electrocardiogram (ECG), transthoracic echocardiogram, ECG stress testing and standard blood analysis including blood glucose (97 mg/dl) were unremarkable. The 24-hour Holter ECG study revealed sinus rhythm with tachycardic activity during 45% of the record, alternating with several periods of ectopic atrial rhythm and one episode of atrial fibrillation lasting 1 hour and 15 minutes. The patient was initially prescribed antiarrhythmic therapy, but the symptoms did not resolve. Electrophysiological study with catheter ablation for atrial fibrillation was discussed and accepted by the patient. Oral anticoagulation was initiated and the pulmonary veins were isolated successfully in November 2010, although the procedure was complicated by a transient period of arterial hypotension and hypoxemia, requiring surveillance in the cardiac intensive care unit for a short period. The patient recovered well and was discharged with indication to maintain oral anticoagulation for three months. During that period, he returned for his periodic cardiological assessment and complained of hematospermia. After discussion with the urology department, antibiotic therapy with levofloxacin was started and abdominal and pelvic ultrasonography was performed, which revealed a 10-cm mass, predominantly cystic, adjacent to the left kidney upper pole. Abdominal magnetic resonance imaging (MRI) enabled better visualization of the mass and showed a nodular formation on the left adrenal gland with a major axis diameter of 9.8 cm, predominantly cystic, with thickened irregular walls and a solid component in the anterior, medial and inferior portions (maximum thickness 4 cm), with heterogeneous late enhancement after contrast administration and diffusion restriction (Figure 1), findings compatible with a giant cystic pheochromocytoma. Urinary metanephrines and plasma catecholamines (specifically adrenaline and noradrenaline) were markedly elevated (Table 1), confirming the diagnosis. A metaiodobenzylguanidine scintigraphy scan revealed localized disease with an intense uptake focus in the left adrenal gland (Figure 2) and no evidence of other uptake foci. Since the patient had no family history of pheochromocytoma, germline mutations that predispose to catecholamine-secreting tumors were not investigated. After appropriate preoperative treatment with phenoxybenzamine, beta-blockers and intravenous fluid expansion, surgical resection of the neoplasm by traditional open surgery was performed in May 2011. Histopathologic and immunohistochemical evaluation were consistent with pheochromocytoma. The immunohistochemical study was positive for chromogranin A, synaptophisin and S100, findings consistent with a diagnosis of cystic pheochromocytoma.8 There were no intraoperative or postoperative complications. Urinary and plasma metanephrines normalized after surgery (Table 1). During follow-up (more than two years) the patient remained asymptomatic without evidence of recurrence.
Abdominal magnetic resonance imaging: T2-weighted transverse (A) and coronal (B) views showing a nodular formation on the left adrenal gland with major axis diameter of 9.8 cm, predominantly cystic, with thickened irregular walls and a solid component in the anterior, medial and inferior portions (maximum thickness 4 cm), with heterogeneous late enhancement after contrast administration and diffusion restriction.
Urinary and plasma metanephrines and catecholamines before and after surgery.
| Before surgery | After surgery | Reference value | |
| Plasma metanephrines | |||
| Metanephrine | – | <17 | <90 pg/ml |
| Normetanephrine | – | 82 | <200 pg/ml |
| Plasma catecholamines | |||
| Adrenaline | >698 | <20 | <150 pg/ml |
| Noradrenaline | >823 | 334 | <370 pg/ml |
| Dopamine | <20 | <20 | <200 pg/ml |
| Urinary metanephrines | |||
| Metanephrine | 6372 | 49 | 74–297 μg/24 h |
| Normetanephrine | 3913 | 156 | 105–354 μg/24 h |
| Urinary catecholamines | |||
| Adrenaline | – | <2 | <18 μg/24 h |
| Noradrenaline | – | 36 | <80 μg/24 h |
| Dopamine | – | 209 | 209 μg/24 h |
Body metaiodobenzylguanidine scintigraphy scan 24 hours after intravenous contrast administration in anterior (A) and posterior (B) views showing a pathological accumulation in the left adrenal gland compatible with pheochromocytoma (note the preferential distribution corresponding to the tumor's solid part); no other uptake foci are evident.
A “rule of 10s” has been attributed to pheochromocytoma, with approximately 10% extra-adrenal location (i.e., secretory paraganglioma), childhood onset, bilateral tumor formation, recurrence after resection, malignant phenotype and familial occurrence.3 Recently, however, inherited germ line mutations have been described in up to 25% of patients.4,9
The catecholamines secreted by these tumors (primarily norepinephrine and epinephrine) are responsible for the clinical manifestations, which can be highly diverse, producing signs and symptoms similar to many other clinical conditions.6 Our patient presented initially with symptoms that were attributed to paroxysmal atrial fibrillation, but these manifestations could have represented hyperadrenergic spells.
Hematospermia is defined as the presence of blood in the ejaculated seminal fluid. Although it is a painless, benign and self-limiting symptom in most cases, its advent may be frightening and alarming to the patient.10 In the case presented, the most likely mechanism for hematospermia was the association between oral anticoagulation and probable episodes of paroxysmal hypertension.11
Cystic pheochromocytomas are less common than the solid variant and are more often asymptomatic (or associated with upper abdominal discomfort only) and have negative biochemical tests, since the tumor burden is smaller.12,13 The cystic component reflects necrosis and liquefaction within the tumor, which can be visualized as a hyperintense signal on T2-weighted MRI. Morphologically, the main characteristic is the relatively thick wall (with or without septa within) and persistent wall enhancement after administration of contrast media,13 as in our patient.
Generally, tumors larger than 6 cm are malignant.12,14 Nevertheless, in this case, the giant cystic mass was probably a benign pheochromocytoma, since no metastatic disease has been detected. Although a variety of immunohistochemical and other prognostic markers have been assessed for association with malignancy in pheochromocytoma,15 currently the only criterion for diagnosis of malignancy is the presence of metastatic spread.16
Once an adrenal neoplasm is diagnosed, early resection is indicated to prevent complications. Before surgery, combined alpha- and beta-adrenergic blockade is recommended to control blood pressure and to prevent intraoperative hypertensive crisis.1,3
Some reports have concluded that laparoscopic adrenalectomy is safe, effective, and minimally invasive and, as such, it is considered the gold standard in the surgical management of small benign adrenal tumors.17 In our case, considering the large size of the tumor (about 10 cm) and possible malignancy, traditional open surgery was performed.
ConclusionThis case illustrates the importance of a high clinical index of suspicion to diagnose pheochromocytoma, since it can have multiple and unusual presentations. In particular, the cystic variant of pheochromocytoma can grow unnoticed due to the lesser tumor burden and give rise to a large mass that in most cases is detected incidentally.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.