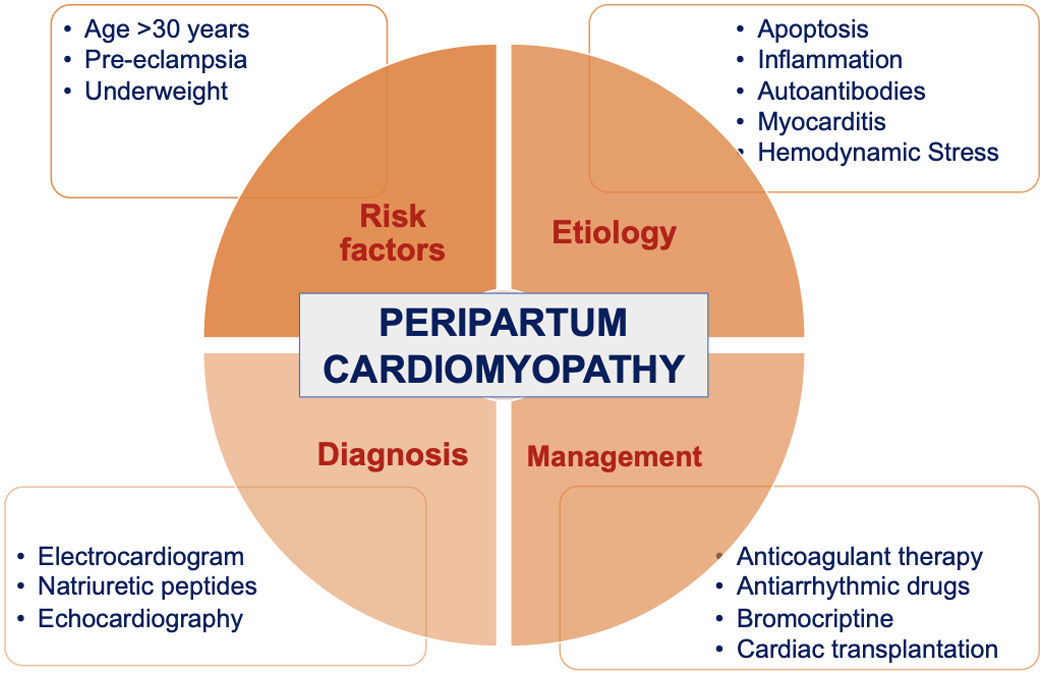
Peripartum cardiomyopathy is a rare type of heart failure manifesting towards the end of pregnancy or in the months following delivery, in the absence of any other cause of heart failure. There is a wide range of incidence across countries reflecting different population demographics, uncertainty over definitions and under-reporting. Race, ethnicity, multiparity and advanced maternal age are considered important risk factors for the disease. Its etiopathogenesis is incompletely understood and is likely multifactorial, including hemodynamic stresses of pregnancy, vasculo-hormonal factors, inflammation, immunology and genetics. Affected women present with heart failure secondary to reduced left ventricular systolic function (LVEF <45%) and often with associated phenotypes such as LV dilatation, biatrial dilatation, reduced systolic function, impaired diastolic function, and increased pulmonary pressure. Electrocardiography, echocardiography, magnetic resonance imaging, endomyocardial biopsy, and certain blood biomarkers aid in diagnosis and management. Treatment for peripartum cardiomyopathy depends on the stage of pregnancy or postpartum, disease severity and whether the woman is breastfeeding. It includes standard pharmacological therapies for heart failure, within the safety restrictions for pregnancy and lactation. Targeted therapies such as bromocriptine have shown promise in early, small studies, with large definitive trials currently underway. Failure of medical interventions may require mechanical support and transplantation in severe cases. Peripartum cardiomyopathy carries a high mortality rate of up to 10% and a high risk of relapse in subsequent pregnancies, but over half of women present normalization of LV function within a year of diagnosis.
A miocardiopatia periparto é um tipo raro de insuficiência cardíaca que se manifesta durante o último mês de gravidez ou nos primeiros meses pós-parto na ausência de doença cardíaca. Existe uma ampla gama de incidência entre os países, refletindo diferentes demografias populacionais, incerteza de definição e subnotificação. A raça, etnia, multiparidade e idade materna são consideradas importantes fatores de risco para a doença. A etiopatogenia é multifatorial, incluindo stress hemodinâmico da gravidez, fatores vasculo-hormonais, inflamatórios, imunológicos e genéticos. Na apresentação, a ecocardiografia normalmente revela ventrículo esquerdo dilatado, função sistólica reduzida, função diastólica comprometida, com FEVE reduzida de <45%, dilatação bi-auricular e aumento da pressão pulmonar. A eletrocardiografia, ressonância magnética, biópsia endomiocárdica e certos biomarcadores sanguíneos auxiliam no diagnóstico e tratamento. O tratamento do periparto inclui terapêuticas farmacológicas para insuficiência cardíaca, como diuréticos, inibidores da enzima de conversão da angiotensina, bloqueadores dos recetores da angiotensina, vasodilatadores, digoxina, betabloqueadores, anticoagulantes e bromocriptina. Os perfis de segurança de fármacos dessas terapêuticas decidem se as mesmas podem ser utilizadas durante a gravidez e a lactação. Terapêuticas direcionadas, como a bromocriptina, mostraram-se promissoras em vários ensaios. A falha das intervenções médicas pode exigir suporte mecânico e transplante em casos graves. A miocardiopatia periparto acarreta uma alta taxa de mortalidade de até 10% e um alto risco de recaída em gestações subsequentes, mas a maioria das mulheres recupera no período de 3 a 6 meses após o início da doença.
The term peripartum cardiomyopathy (PPCM) was first introduced in 1971 by Demakis et al. and Demakis and Rahimtoola in their influential publications.1,2 Although heart failure associated with pregnancy and/or the peripartum period had been identified much earlier by Virchow and others in the 1800s,3,4 the dawn of echocardiography permitted the development of diagnostic criteria for PPCM in 1999.5
Traditionally, PPCM was defined as the development of heart failure in the last month of pregnancy or within five months postpartum in the absence of prior heart disease or an identifiable cause of heart failure, with left ventricular ejection fraction (LVEF) <45%, fractional shortening <30%, or both, with or without a left ventricular (LV) end-diastolic dimension (LVEDD) >2.7 cm/m2 body surface area.5 This definition was first approved by a workshop held by the US National Heart, Lung, and Blood Institute (NHLBI) and the Office of Rare Diseases. However, in 2010 it was updated and simplified by the Heart Failure Association of the European Society of Cardiology (ESC) Working Group on peripartum cardiomyopathy. Many patients present with PPCM before the 36th week of gestation, giving rise to widespread concerns that the NHLBI definition could lead to underdiagnosis.6 The ESC therefore proposed a simpler definition: “Peripartum cardiomyopathy is an idiopathic cardiomyopathy presenting with heart failure secondary to left ventricular systolic dysfunction towards the end of pregnancy or in the months following delivery, where no other cause of heart failure is found. It is a diagnosis of exclusion. The left ventricle may not be dilated but the ejection fraction is nearly always reduced below 45%.”7
Irrespective of the diagnostic criteria, PPCM remains an overlooked or misdiagnosed condition. It is rare and is therefore not widely recognized among physicians, leading to delayed diagnosis and treatment. Counseling of women with a history of PPCM regarding risk of relapse in subsequent pregnancies is a challenge in the absence of definitive knowledge in this field. In this review we have attempted to summarize the current literature on the pathogenesis, presentation, and management of PPCM.
EpidemiologyFew countries worldwide have definitive data on the incidence of PPCM. The reported incidence in a single center in South India was one case per 1541 live births,8 while in the US it ranges from ≈1 in 1000 to 1 in 4000 live births.9,10 Analysis of data from the US Nationwide Inpatient Sample database of 64 million hospital records identified 34219 cases of PPCM, with an incidence of 1 in 968 births. A worldwide registry on PPCM revealed 500 cases up to April 30, 2016, the incidence varying according to ethnicity, i.e. Caucasian (34%), Black African (25.8%), Asian (21.8%), and Middle Eastern backgrounds (16.4%).11 A literature search revealed the highest incidence in Haiti and Nigeria, with reported incidences of 1 in 300 and 1 in 100 live births, respectively,12,13 and the lowest in Japan, with an incidence of 1 in 15000 births.14 This wide range of incidence reflects different population demographics and uncertainty over definition, resulting in under-reporting and lack of awareness or misdiagnosis.
Isogai and Kamiya investigated the worldwide incidence of PPCM in 2019, highlighting various difficulties in determining its incidence accurately.14 Their search revealed only four prospective studies, all the others being retrospective. Lack of clarity on the pathogenesis and diagnostic criteria for PPCM means a large-scale prospective cohort study is required to determine an accurate incidence; however, the rarity of PPCM makes conducting such a study difficult.
Risk factorsAge over 30 years is associated with PPCM in more than 50% of cases.6 In a 2011 study, women's race and ethnicity was found to be associated with the occurrence of PPCM, with higher rates observed among non-Hispanic African American and Filipino groups and lower rates in Chinese and Hispanic women.10 The study showed that PPCM was more likely to occur in older women with four or more total births. Independent predictors of PPCM included severe anemia, multiple gestation, pre-existing and pregnancy-related hypertension, pre-eclampsia or eclampsia, and hemolysis, elevated liver enzymes and low platelets syndrome.10
Pre-eclampsia is a rare but important cause of peripartum cardiomyopathy.14 A meta-analysis of 22 studies including 979 cases revealed a 22% prevalence of pre-eclampsia in women with PPCM, four times the 3–5% population prevalence, and a hypertensive disorder was present in 37% of cases.15 The ESC's EURObservational Research Programme PPCM registry revealed that women with pre-eclampsia had more severe symptoms, more frequent signs of heart failure and a smaller LVEDD than women with no hypertensive disorder. However, they were likely to have better recovery.16
A higher incidence of peripartum cardiomyopathy among Nigerian women and the results of the PEACE registry may indicate that poor nutrition plays a role.17 Selenium deficiency among Nigerian women is reported to be a risk factor for PPCM,13,18 and selenium supplementation in patients with heart failure leads to improved outcomes.18
EtiologyThere is evidence that various mechanisms may be responsible for PPCM, including hemodynamic stresses of pregnancy, vasculo-hormonal factors, inflammation, immunology and genetics.18–28 These remain plausible etiologies, but none of them is definitive since PPCM is primarily considered an idiopathic myocardial disease of pregnancy.
Vasculo-hormonal factorsPPCM is associated with angiogenic imbalance, which is accentuated by pre-eclampsia.15,20,27,28 Peroxisome proliferator-activated receptor-gamma coactivator-1 alpha (PGC-1α) regulates angiogenesis by facilitating expression of angiogenic factors like vascular endothelial growth factor (VEGF), and soluble fms-like tyrosine kinase 1 (sFlt-1) inhibits VEGF. It has been demonstrated that lack of cardiac PGC-1α in mice leads to the development of PPCM. The human placenta secretes sFlt-1 in late gestation, and this is accentuated in pre-eclampsia. The antiangiogenic environment created by sFlt-1 is accompanied by cardiac dysfunction, demonstrated by abnormally high serum levels of sFlt-1 that are found in women with PPCM. This strongly suggests that PPCM is primarily a vascular disease that is aggravated by the presence of hypertensive disorders of pregnancy, which would explain why pre-eclampsia is a risk factor for the development of PPCM.
Similarly, cardiac tissue-specific signal transducer and activator of transcription 3 (STAT3) promotes myocardial angiogenesis by paracrine and autocrine mechanisms.26 STAT3 also provides protection from oxidative stress by upregulating antioxidant enzymes such as the reactive oxygen species (ROS)-scavenging enzyme manganese superoxide dismutase. Increased oxidative stress causes cleavage of the nursing hormone prolactin into an antiangiogenic 16-kDa fragment. Increased levels of the 16-kDa form of prolactin and reduced levels of STAT3 are found in patients with PPCM. Deletion of cardiomyocyte-specific STAT3 in mice leads to the development of PPCM. This implies that inhibition of prolactin may form a therapeutic strategy for PPCM, which was demonstrated by treating STAT3-knockout mice with bromocriptine.26
Apoptosis and inflammationThe same 16-kDa prolactin fragment causes cardiomyocyte damage by inducing small lipid-encapsulated particles called microRNA 146a (miR-146a),20,25 which suppress certain pathways within cardiomyocytes, thereby promoting their apoptosis. Similarly, Fas/APO-1, an apoptosis-signaling surface receptor, also triggers programmed cell death. Plasma levels of miR-146a and Fas/APO-1 were found to be elevated in women with PPCM.
Sarojini et al. found elevated plasma levels of C-reactive protein (CRP), tumor necrosis factor alpha (TNF-α), and interleukin-6, with correspondingly greater LV dimensions and lower LVEF, in patients with PPCM in India.22 These results indicate that inflammatory markers can be predictors of mortality and that miR-146a could be used as a diagnostic biomarker for PPCM. Similarly, in a single-center study in South Africa, Sliwa et al. found elevated plasma levels of CRP, TNF-α and Fas/APO-1 in 15 patients who died of PPCM.23 These higher levels of inflammatory cytokines correlated with lower LVEF and greater LV dimensions.
AutoantibodiesRecently, autoimmune mechanisms in heart disease have attracted research interest. β1-Adrenergic receptor autoantibodies (β1R-AAs) and M2-muscarinic receptors (M2R-AABs) are involved in heart failure. Liu et al.24 demonstrated positive rates for β1R-AABs and M2R-AABs of 59.5% (22/37) and 45.9% (17/37) in PPCM patients, and 19.4% (7/36) (p<0.001) and 16.67% (6/36) (p<0.001) in normal pregnant women, respectively. These antibodies had a positive correlation with increased LV dimension and elevated natriuretic peptides. The authors concluded that they are independent risk factors for the onset of PPCM.
GeneticsThere is strong emerging evidence of an overlapping genetic substrate between dilated cardiomyopathy (DCM) and PPCM.29 The TTN gene, which encodes the sarcomere protein titin, has been linked with PPCM. In a cohort of 18 families with PPCM, Van Spaendonck-Zwarts et al. demonstrated a high proportion of TTN mutations and a low recovery rate in PPCM cases.30 Similarly, Goli et al. demonstrated that 10% of 469 enrolled women with PPCM harbored truncating variants of TTN. Although TTN is likely the most common genetic cause of PPCM, other previously unidentified genes including FLNC, DSP and BAG3 are now thought to be associated with its development. These genes are similar to those identified with non-ischemic DCM. These findings point toward a genetic cause of PPCM and may have important implications regarding genetic counseling in these patients.31
MyocarditisMyocarditis has traditionally been associated with the occurrence of PPCM. In a study on 18 patients, 14 patients had findings suggestive of myocarditis on endomyocardial biopsy.32 Myocarditis of viral etiology has been confirmed by endomyocardial biopsy in a few studies on women with PPCM, although similar proportions also had serologic evidence of viral infection in other forms of cardiomyopathy.19,33
Hemodynamic stressLarge hemodynamic shifts are triggered in pregnancy, peaking at the end of the second trimester,34 and can uncover pre-existing cardiac disease and present as heart failure.35 However, by definition this is not PPCM.
Clinical presentation and diagnosisWomen with PPCM most commonly present in the last month of pregnancy or in the first five months postpartum with symptoms of dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, edema of the lower extremities, fatigue, chest pain and cough.17,21,36 A few patients may also present in cardiogenic shock, in which case a diagnosis of myocardial infarction (MI), pulmonary embolism (PE) or amniotic fluid embolism (AFE) should also be considered. A minority of patients present with severe arrhythmias.37 Physical examination may reveal pulmonary rales, raised jugular venous pressure, peripheral edema, tachypnea, and tachycardia with irregular peripheral pulses, displaced apical impulse, or murmurs of mitral and tricuspid regurgitation.
Associated conditions such as hypertensive disorders of pregnancy, pre-eclampsia, advanced maternal age, multifetal pregnancy and multiparity are risk factors for PPCM and should be suspected in women presenting with symptoms and signs of cardiac failure.20,33 Women with pre-eclampsia present with peripheral edema and pulmonary rales, increased serum creatinine levels, prolonged QRS duration and left bundle branch block.16
An initial 12-lead electrocardiogram will help in identifying associated arrhythmia and differentiating PPCM form certain other cardiac causes. No specific electrocardiographic (ECG) pattern is associated with PPCM, therefore conditions with specific ECG findings such as acute MI and right heart causes of heart failure including PE and AFE can be ruled out.
In the epidemiological setting of COVID-19, viral myocarditis may also be ruled out.38 In the presence of raised cardiac biomarkers and viral symptoms, viral panels should be performed or the presence of virus in the endocardium can be demonstrated with an endomyocardial biopsy, to rule out viral myocarditis. Natriuretic peptides, with a threshold of <100 pg/ml for B-type natriuretic peptide (BNP) and <300 pg/ml for N-terminal proBNP, play an important role in ruling out heart failure,21,39 since levels remain normal or are only slightly elevated during pregnancy and postpartum and are markedly elevated in PPCM.
Echocardiography should be used early in all cases of suspected PPCM to confirm the diagnosis, to assess associated cardiac conditions and their severity, and to exclude complications of PPCM such as thromboembolism. Prognostic information can also be obtained at the same time. Echocardiography will typically reveal LV dilatation, depressed systolic function, impaired diastolic function, reduced LVEF (<45%), biatrial dilatation, and increased pulmonary pressure resulting in moderate to severe tricuspid and mitral regurgitation.4,40 Annular dilatation secondary to marked LV enlargement leads to mitral regurgitation. The echocardiographic features are generally indistinguishable from those of primary idiopathic DCM and can be differentiated based on the onset of presenting symptoms. Idiopathic DCM generally presents during the second trimester and PPCM has a rapidly worsening clinical course with poor outcome.
ManagementAcute heart failure during pregnancyRapid diagnosis and decision-making are essential for all pregnant women with acute heart failure, as are a management algorithm and establishment of a multidisciplinary team that includes cardiologists, intensivists, obstetric physicians, neonatologists, anesthesiologists, and cardiac surgeons. At the same time, the welfare of the fetus must be considered while implementing diagnostic tests and treatment during pregnancy. Therapeutic recommendations for mild, moderate, and severe forms of heart failure are listed under the BOARD (Bromocriptine, Oral heart failure therapy, Anticoagulation, vasoRelaxing agents, and Diuretics) label in Table 1.41,42 Women with severe forms of heart failure will require intensive care management, with invasive monitoring including intra-arterial blood pressure, central venous pressure, and a pulmonary artery catheter. Women presenting with shock will require inotropic and vasopressor support. Patients refractory to medical management may require short-term assist devices in the form of extracorporeal membrane oxygenation or long-term devices such as a ventricular assist device (VAD).43
BOARD therapeutic scheme for peripartum cardiomyopathy in acute and chronic heart failure and their safety profile during pregnancy and lactation.20,40,41
| Treatment | Acute | Chronic | Safety profile | |
|---|---|---|---|---|
| Pregnancy | Lactation | |||
| Bromocriptine | 2.5 mg for 1 week, 5 mg for 2 weeks and 2.5 mg for 6 weeks | Prevents lactation | ||
| Oral heart failure drugs | ||||
| ACEIs | Continue for 12–24 months after recovery | Essential for all patients | Teratogenic | Enalapril/captopril |
| ARBs | Continue for 12–24 months after recovery | In patients who do not tolerate ACEIs | Teratogenic | Avoid |
| Beta-blockers | Continue for 12–24 months after recovery | Essential for all patients | Safe in pregnancy. Use with some caution. Near delivery observe infants for bradycardia/hypotension | Metoprolol/bisoprolol |
| Ivabradine | Discontinue if HR <50 bpm | Recommended if HR >70 bpm | Use with caution | Avoid |
| Cardiac glycoside | Use with caution | Digoxin | ||
| SGLT2i | May be added post lactation | Teratogenic | ||
| Anticoagulation | ||||
| Vitamin K antagonists | Teratogenic in first trimesterSecond and third trimester: use with extreme caution | Warfarin | ||
| Non-vitamin K antagonist oral anticoagulants | Avoid | Avoid | ||
| Unfractionated heparin | Use with caution | Use with caution | ||
| LMWH | Preferred anticoagulant | Dalteparin/enoxaparin | ||
| Fondaparinux | Use with caution | Avoid | ||
| Relaxants | ||||
| Vasodilators | Use with caution. Hydralazine can be used | Hydralazine | ||
| Nitrates | Use with caution | Use with caution | ||
| Diuretics | ||||
| Mineralocorticoid receptor antagonists | Stop after recovery | Eplerenone preferred | Avoid if possible. May cause feminization of fetus | Use with caution |
| Loop diuretics | Taper if no signs of fluid overload | Recommended in patients with fluid overload | Use with caution for reduced placental blood flow | Use with caution |
| Thiazide diuretics | Taper if no signs of fluid overload | Recommended in patients with fluid overload | Use with caution for reduced placental blood flow | Hydrochlorthiazide |
ACEIs: angiotensin-converting enzyme inhibitors; ARBs: angiotensin receptor blockers; bpm: beats per minute; HR: heart rate; LMWH: low molecular weight heparin; SGLT2i: sodium-glucose co-transporter 2 inhibitor.
Drugs such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, which are contraindicated in pregnancy because of their potential to cause birth defects, can be used postpartum.39,42 Similarly, diuretics can be used in the postpartum period without the risk of compromising uterine perfusion and are effective in reducing preload.
Anticoagulant therapyPregnancy is inherently a hypercoagulable state, and when coupled with a severe form of PPCM with associated atrial fibrillation or mural thrombi, there is a high risk of venous and arterial thrombosis due to ventricular dysfunction-induced blood stasis.44,45 Anticoagulation with heparin during pregnancy and with heparin or warfarin postpartum is recommended. The therapy may be continued until there is significant recovery in LV function.
Antiarrhythmic drugsPregnancy is associated with an increased incidence of arrhythmias, particularly premature ventricular complexes, even in women without pre-existing heart disease. PPCM is significantly associated with ventricular arrhythmia. Data from 9841 cases revealed arrhythmia in 18.7% of patients, with ventricular tachycardia (4.2%) being the most common. Atrial fibrillation was present in 1.3%, bundle branch block in 1.7%, ventricular fibrillation in 1% and cardiac arrest in 2.2%.37 Arrhythmia can cause serious risk to women with PPCM.
BromocriptineBromocriptine is a dopamine D2 receptor agonist and acts by inhibiting prolactin release. The antiangiogenic 16-kDa form of prolactin is known to exert detrimental effects on the cardiac microvasculature, leading to dysfunction.46,47 In small trials, PPCM patients who received bromocriptine showed better recovery at six months with improved LV function.47 Bromocriptine use is associated with thromboembolic events; therefore, prophylactic doses of anticoagulants should always accompany treatment with bromocriptine.
Hilfiker-Kleiner et al. conducted a multicenter randomized trial that revealed full functional LV recovery (LVEF >50%) at six months in 52% of patients who received 2.5 mg bromocriptine for one week postpartum, while 68% of patients who received 5 mg for two weeks followed by 2.5 mg for six weeks achieved complete recovery.46 Haghikia et al. demonstrated improved right ventricular function in 24 patients with right ventricular ejection fraction <45% at six-month follow-up after being prescribed bromocriptine.49 This finding suggests that bromocriptine is effective in patients with biventricular failure.
Cardiac transplantationIn the worst-case scenario, if all possible conservative therapeutic options fail, heart transplantation is the last treatment choice. Up to 10% of PPCM patients require heart transplantation. Jawad et al. reported five patients who received orthotopic heart transplantation.43 Four of these patients had previously received a VAD and median time to transplantation from PPCM onset was 140 days. In women with severe life-threatening PPCM heart transplantation appears to be a safe therapeutic option with or without intervening mechanical circulatory support.
DeliveryUnless PPCM threatens the life of mother or fetus, there is no indication for early delivery, but onset of hemodynamic instability requires urgent delivery irrespective of gestation period. A planned Caesarean section with appropriate inotropic/vasopressor and/or mechanical support is preferred in decompensated or very severe heart failure, while induction of labor may be possible in most asymptomatic women with less severe heart failure. Important considerations during labor and surgical delivery include prevention of fluid overload and pulmonary edema, invasive hemodynamic monitoring for management of cardiac output, supine hypotension, and the anesthetic technique.50,51
Epidural analgesia is recommended during labor as it will stabilize cardiac output, while combined spinal and epidural anesthesia is preferred for Caesarean sections.
BreastfeedingIn most women with stable PPCM, breastfeeding can be supported. However, in women with severe heart failure, the high metabolic demands of lactation and breastfeeding require consideration of prevention of lactation.52 Adopting this approach enables optimum use of all heart failure drugs without risk to fetus and newborn.
PrognosisWomen with PPCM appear to have a more favorable outcome than those with other forms of cardiomyopathy. Mortality at six months ranged from 2% in Germany to 12.6% in South Africa, while mortality at 12 months was 4–14% and 7% at a mean follow-up of 19 months. Much of this information is from small studies of selected geographical populations.16,53,54
Counseling and subsequent pregnanciesWomen are recommended to undergo six-monthly echocardiography until LVEF recovers to >50% and annual visits for 10 years for women who remain stable after tapering of drug therapy for heart failure.21 Echocardiographic findings of persistent LV dilatation or reduced myocardial strain may be present in some patients despite normal LV function. In such patients life-long heart failure therapy should be continued.
Few studies have reported subsequent pregnancies in women with PPCM. Heart failure symptoms are more frequent in women whose LVEF had not normalized before a subsequent pregnancy. Therefore, all patients with persistent LV dysfunction should be advised against future pregnancies. All patients with previously diagnosed PPCM and their partners should receive careful counseling (class I recommendation) concerning the longer-term prognosis and undergo a risk stratification if further pregnancies are considered.54 Based on a recent publication reporting on the outcome of women with PPCM and subsequent pregnancy in cohorts from Germany, Scotland and South Africa, women with impaired systolic function are at substantial risk of relapse and death and should therefore be strongly advised against pregnancy. As any subsequent pregnancy in a woman with PPCM entails a substantial risk, those women should be monitored by an experienced multidisciplinary team throughout pregnancy and for at least one year postpartum.
ConclusionPPCM remains an underdiagnosed peripartum disease due to its rarity. Women with symptoms consistent with heart failure should undergo clinical examination and cardiac biomarker testing, and echocardiography should be considered if these are abnormal. Tests of miR-146a and Fas/APO-1 may be useful bedside diagnostic modalities in the future. Heart failure should be managed according to current guidelines, respecting the safety limitations during pregnancy and breastfeeding. There is some evidence that bromocriptine might be helpful; a definitive trial is currently underway in the USA. Supportive therapy for heart failure should be initiated promptly and patient monitoring should be continued even after recovery of LV function. Women with PPCM or who experienced PPCM in a previous pregnancy should be managed by an experienced multidisciplinary pregnancy heart team. This should include careful pre-pregnancy reassessment and counseling.
Conflicts of interestRajni Bala and Dr. Sakshi Mehta are employees of Adduct Healthcare Pvt. Ltd., Mohali, India. Vikas C. Roy, Geetika Kaur and Antonio de Marvao have no conflicts of interest to declare.
The authors thank Adduct Healthcare Pvt. Ltd., Mohali, India (www.adducthealthcare.com) for medical writing assistance.