We present the case of a 73-year-old woman with a history of pulmonary embolism referred to our department due to suspected pulmonary hypertension.
She was in WHO II functional class and the transthoracic echocardiogram showed pulmonary artery systolic pressure of 58 mmHg, with no right ventricular dilatation or dysfunction. Ventilation/perfusion scan after 3 months of oral anticoagulation confirmed the perfusion defects and right heart catheterization confirmed precapillary pulmonary hypertension (mean pulmonary artery pressure 36 mmHg, pulmonary vascular resistance 5.19 Wood units), so a diagnosis of chronic thromboembolic pulmonary hypertension was established.
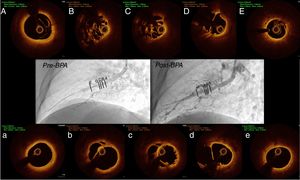
The patient refused pulmonary thromboendarterectomy and vasodilator therapy was started. In December 2017 the patient was still symptomatic, so she underwent five sessions of balloon pulmonary angioplasty (BPA), leading to hemodynamic normalization and clinical improvement. In the third session, the A8 segment of the right lower lobe was treated. Slow arterial flow was found, with no venous return, although no lesion was seen on angiography (Figure 1 Pre-BPA and Video 1). Optical coherence tomography (OCT) (contrast infusion protocol of 10 ml/s in 4 seconds at 400 psi) documented a web lesion at the level of the bifurcation (Figure 1A-E). Dilation with semi-compliant balloons (diameter 2.0-3.0 mm) was performed. OCT after dilation documented lumen expansion and recanalization of the web lesion (Figure 1a-e). Angiographically, there was improvement in arterial flow and venous return (Figure 1 Post-BPA and Video 2).
(A-E) Optical coherence tomography of A8 segment of the right lower lobe documenting a web lesion (type B); Pre-BPA: angiogram before balloon pulmonary angioplasty; Post-BPA: angiogram after balloon pulmonary angioplasty; (a-e) optical coherence tomography of A8 segment after dilation with semicompliant balloons (2.0 and 3.0 mm diameter at 58.8 Psi) documenting recanalization of the web lesion.
OCT is still an experimental tool in BPA that needs further validation. Nevertheless, it is useful in the identification of the type of lesion and for balloon sizing, and can also help to elucidate the pathological mechanisms of the disease.
Conflicts of interestThe authors have no conflicts of interest to declare.