Arrhythmias are often recorded in strength training athletes without cardiovascular abnormalities but may also be a sign of an underlying cardiovascular disease which carries a risk of sudden cardiac death (SCD). Nowadays, bodybuilding is a popular sport among adolescents and young adults. There have been few studies of arrhythmias comparing bodybuilders with healthy controls and excluding anabolic steroid use. We aimed to assess the structural, functional and electrical characteristics of bodybuilders’ hearts compared with control subjects.
MethodsIn this study, we assessed 35 male competitive bodybuilders and 35 healthy control subjects matched for age, gender, and body mass index. A detailed cardiovascular and systemic examination was performed at the beginning of the study to collect demographic data and anthropometric measures. Biochemical and hematologic, echocardiographic, 24-h Holter, and ECG measurements were obtained from all participants.
ResultsVentricular arrhythmias were encountered significantly more frequently in bodybuilders than in the control group. QT and QTc were not significantly different between groups. Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio were significantly greater in bodybuilders than in the control group (p<0.001 for all). There was a positive correlation between Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio and right ventricular (RV) diameter and arrhythmias.
ConclusionProlonged repolarization is common in athletes, although its predictive value is unclear. In this study, alterations in ventricular repolarization were positively correlated with RV dimensions. Therefore, we postulate that arrhythmias in strength athletes may be predicted by assessing the right ventricle echocardiographically and dispersions of repolarization on the ECG, and that SCD could be avoided in strength athletes by careful application of this information.
As arritmias são registadas muitas vezes nos atletas de alta competição sem alterações cardiovasculares, podendo no entanto ser um sinal de doença cardiovascular subjacente, o que constitui um prognóstico de risco de morte súbita cardíaca (MSC). Hoje em dia o fisiculturismo é um desporto popular praticado por muitos adolescentes e adultos jovens. Não são muitos os estudos comparativos entre os fisiculturistas e grupos de controlo saudáveis. Foi nosso objetivo avaliar as características estruturais, funcionais e elétricas do coração dos fisiculturistas comparadas com as do grupo controlo.
MétodoNeste estudo avaliámos 35 fisiculturistas de competição do sexo masculino e 35 indivíduos saudáveis do grupo controlo, emparelhados por idade, género e índice de massa corporal. Foram realizados exames cardiovasculares e sistémicos no início do estudo, com registo de dados demográficos e medidas antropométricas. Foram obtidos registos bioquímicos e hematológicos, ecocardiográficos e do registo de Holter de 24 horas, bem como medições eletrocardiográficas de todos os participantes.
ResultadosAs arritmias ventriculares encontradas foram significativamente mais frequentes nos fisiculturistas do que no grupo controlo. Os valores do QT e do QTc não foram significativamente diferentes entre os grupos. O intervalo Tp-e, a relação TP-e/QT e a relação Tp-e/QTc foram significativamente superiores no grupo dos fisiculturistas quando comparado com o grupo controlo (p<0,001). Verificou-se uma correlação positiva entre o intervalo Tp-e, a relação Tp-e/QT e a relação Tp-e/QT com o diâmetro do ventrículo direito (VD) e a arritmia.
ConclusãoA repolarização prolongada é comum nos atletas, mesmo quando o seu valor preditivo é pouco claro. Neste estudo, as alterações na repolarização ventricular foram positivamente correlacionadas com as dimensões do VD. Assim, admitimos que as arritmias nos atletas de alta competição possam ser previsíveis através de ecocardiografia do VD e por dispersões da repolarização no ECG. Por último, a MSC pode ser evitável nos atletas de alta competição com recurso a este tipo de interpretação, considerada razoável e passível de aplicação.
It is well established that moderate-intensity exercise reduces the risk of cardiovascular mortality and morbidity.1 However, vigorous exercise can transiently increase the risk of sudden cardiac death (SCD).2 Thus, moderate exercise is better than no exercise, but vigorous exercise may be harmful to some individuals. Nowadays, bodybuilding is a popular sport among adolescents and young adults. Bodybuilders perform principally high static and low dynamic work aiming to increase muscle mass. Dynamic exercise mainly induces volume load in the cardiac cavities, whereas static exercise causes mainly pressure load.3 The types of exercises performed by bodybuilders increase stroke volume and cardiac output to a greater degree than in other athletes.4
Increased cardiac preload and afterload is associated with symmetrical enlargement of all cardiac chambers.5 Athlete's heart, which is characterized by hypertrophy and/or dilatation of the cardiac chambers with normal or enhanced function, may be induced by chronic physical training. However, slight differences in echocardiographic patterns are observed consistent with the type of training.1
Cardiac hypertrophy is associated with alterations in the electrophysiological properties of the heart, which may thus become more susceptible to malignant tachyarrhythmias. Several mechanisms have been proposed to explain the vulnerability of the hypertrophied ventricle to life-threatening arrhythmias. Furthermore, in some individuals long-term exercise training may cause adverse structural and electrical cardiac remodeling, including fibrosis and stiffening of the atria, right ventricle, and large arteries.6 Also, the combination of interstitial fibrosis and stiffening leads to abnormalities in ventricular repolarization.7,8
Myocardial repolarization can be assessed by various methods on the electrocardiogram (ECG) including QT interval dispersion, corrected QT dispersion (QTc), the interval between the peak and the end of the T wave (Tp-e) and novel indices, the Tp-e/QT ratio and Tp-e/QTc ratio.9,10 An increased Tp-e interval may also be a useful index to predict ventricular arrhythmias (VAs) and cardiovascular mortality.11,12 Frequent premature ventricular complexes (PVCs) are often recorded in trained athletes without cardiovascular abnormalities but may also be a sign of underlying cardiovascular disease and predict risk of SCD.13–17
Although ventricular repolarization and VAs have been widely assessed in bodybuilders using anabolic steroids, there have been few studies of arrhythmias comparing bodybuilders with healthy controls and excluding anabolic steroid use.18 We aimed to assess the structural, functional and electrical characteristics of bodybuilders’ hearts compared with control subjects.
MethodsStudy populationIn this study, we assessed 35 male competitive bodybuilders and 35 healthy control subjects matched for age, gender, and body mass index (BMI). All bodybuilders had been training intensively for at least five years. Prior to data collection, the study was approved by the appropriate institutional ethics committee and written informed consent was obtained from each participant. Androgenic anabolic steroid users were excluded from the study. All the participants were in sinus rhythm and none were using medications such as antiarrhythmics, tricyclic antidepressants, antihistamines, or antipsychotics.
In all subjects, a detailed cardiovascular and systemic examination was performed at the beginning of the study to collect demographic data and anthropometric measures including weight, height, BMI, and body surface area (BSA). Biochemical and hematologic measurements were also obtained from all participants.
Echocardiographic assessmentEchocardiography was performed in left lateral decubitus position with a General Electric Vingmed Vivid 5 system (GE Vingmed Ultrasound AS, Horten, Norway) and a 3.5 MHz 3S-RS probe. A single-lead ECG was recorded continuously during the echocardiographic examination. Two-dimensional and M-mode images were acquired in parasternal long- and short-axis and apical 4-chamber views. All measurements were averaged over three cardiac cycles. Two-dimensional echocardiographic measurements were performed according to the standards outlined by the American Society of Echocardiography.19 Left atrial (LA) and left ventricular (LV) dimensions and wall thicknesses were obtained in parasternal long-axis view with the M-mode cursor positioned just beyond the mitral leaflet tips, perpendicular to the long axis of the ventricle. LV end-diastolic (LVEDD) and end-systolic (LVESD) diameter and interventricular septal (IVST) and LV posterior wall (PWT) thicknesses were measured. LV ejection fraction (LVEF) was calculated by Simpson's method.19,20
LV mass (LVM) and LVM indexed to BSA (LVM index) were estimated by LV cavity dimension and wall thickness at end-diastole. The Devereux formula21 was used to determine LVM: LVM (g)=0.8{1.04[([LVEDD+IVST+PWT]3-LVEDD3)]}+0.6. LVM index was calculated as LVM divided by BSA. Relative wall thickness (RWT) allows further classification of LV mass increase as either concentric (RWT >0.42) or eccentric hypertrophy (RWT ≤0.42) and was calculated as RWT=(2×PW)/LVEDD.
Right ventricular (RV) and right atrial (RA) dimensions and mitral and tricuspid valvular velocities were obtained in apical 4-chamber views. Mitral inflow velocities were measured by pulsed-wave Doppler echocardiography with the sample volume placed at the tip of the mitral leaflets in apical 4-chamber view. Peak early (E) and late (A) diastolic transmitral flow velocities were measured and the E/A ratio was calculated. Tricuspid regurgitation (TR) jets were measured by continuous wave Doppler across the tricuspid valve. RV systolic pressure is a useful measure of pulmonary hypertension, and can be estimated from even small TR jets. Pulmonary artery systolic pressure (PASP) was measured indirectly from the modified Bernoulli equation (4V2+RAP), where V is peak velocity of the TR jet, and RAP is estimated or assumed right atrial pressure.20
Interpretation of electrocardiographic and Holter recordingsStandard 12-lead ECGs were obtained at rest in the supine position with a paper speed of 25 mm/s and voltage of 10 mm/mV. Resting heart rate was measured from the ECG taken during patient assessment. QT interval was defined as the time from the onset of the Q wave to the end of the T wave. QTc was calculated by using Bazett's formula.22 The Tp-e interval was measured from the peak of the T wave to the end of the T wave.7 The end of the T wave was defined as the intersection of the tangent to the downslope of the T wave and the isoelectric line. From these measurements the Tp-e/QT and Tp-e/QTc ratios were calculated. The ECGs were assessed by two cardiologists. The interobserver and intraobserver coefficients of variation were 2.1% and 1.8%, respectively.
Three-channel digital 24-h Holter recordings were obtained to assess arrhythmias on the participants’ resting day using a BI9800TL+3 system (Biomedical Instruments). PVCs, ventricular tachycardia (VT), atrial premature complexes (APCs), supraventricular tachycardias and atrial fibrillation were identified from analysis of the 24-h Holter recordings.
Statistical analysisThe statistical analysis was performed using IBM SPSS version 20.0 (IBM SPSS Inc, Chicago, IL, USA). Variables were expressed as mean ± standard deviation and were tested for normality of distribution by the Shapiro-Wilk test. An independent sample t test was used to analyze normally distributed variables and the Mann-Whitney U-test to analyze non-normally distributed variables. Correlation was analyzed using Spearman's correlation coefficient (r). Categorical data were presented as frequencies and percentages and were analyzed by Pearson's chi-square, continuity correction chi-square and Fisher's exact tests. p-values less than 0.05 were considered statistically significant.
ResultsWe analyzed 35 male competitive bodybuilders and 35 healthy control subjects matched for age, gender, and BMI. The four bodybuilders who were using anabolic steroids were excluded from the analysis. The bodybuilders had been training intensively for 7.0±0.64 years. No significant differences were observed between the groups in age, height, weight, BSA, BMI, blood pressure, or laboratory findings (except BUN and creatinine: p=0.030 and p=0.001, respectively). However, the controls had higher HR than the bodybuilders (71.80±1.78 and 66.23±1.91 bpm, respectively; p=0.037) (Table 1).
Demographic data, anthropometric measures, and biochemical and hematologic laboratory results in the study population.
| Controls (n=35) | Bodybuilders (n=35) | p | |
|---|---|---|---|
| Age, years | 28.06±0.73 | 26.29±1.14 | 0.060 |
| Height, cm | 173.8±1.01 | 175.5±1.31 | 0.225 |
| Weight, kg | 73.54±1.67 | 76.60±2.21 | 0.269 |
| BMI, kg/m2 | 24.34±0.51 | 24.76±0.52 | 0.576 |
| BSA, m2 | 1.88±0.024 | 1.93±0.033 | 0.248 |
| Years of sport participation | - | 7.0±0.64 | - |
| SBP, mmHg | 116.71±1.34 | 120.29±1.81 | 0.105 |
| DBP, mmHg | 70.86±0.86 | 73.43±1.16 | 0.131 |
| HR, bpm | 71.80±1.78 | 66.23±1.91 | 0.037 |
| TC, mg/dl | 165.51±5.99 | 167.03±7.1 | 0.911 |
| LDL-C, mg/dl | 109.34±5.24 | 108.71±6.2 | 0.986 |
| HDL-C, mg/dl | 43.57±1.31 | 47.11±1.89 | 0.127 |
| TG, mg/dl | 128.49±14.81 | 122.43±8.65 | 0.424 |
| Hb, g/dl | 15.30±0.15 | 15.61±0.13 | 0.117 |
| HCT, % | 44.75±0.43 | 45.72±0.36 | 0.085 |
| WBC, 103/μl | 6.91±2.53 | 7.46±2.73 | 0.141 |
| Platelets, 103/μl | 223.03±6.36 | 219.74±6.86 | 0.127 |
| BUN, mg/dl | 13.35±0.57 | 15.33±0.69 | 0.030 |
| Cr, mg/dl | 0.88±0.02 | 0.98±0.02 | 0.001 |
| ALT | 22.11±1.73 | 24.91±2.56 | 0.800 |
| Na, mmol/l | 142.8±1.34 | 14.46±0.39 | 0.180 |
| K, mmol/l | 4.40±0.04 | 4.48±0.46 | 0.192 |
| Blood glucose, mg/dl | 90.65±2.31 | 87.14±2.1 | 0.353 |
ALT: alanine transaminase; BMI: body mass index; BSA: body surface area; BUN: blood urea nitrogen; Cr: creatinine; DBP: diastolic blood pressure; Hb: hemoglobin; HCT: hematocrit; HDL-C: high-density lipoprotein cholesterol; HR: heart rate; K: potassium; LDL-C: low-density lipoprotein cholesterol; Na: sodium; SBP: systolic blood pressure; TC: total cholesterol; TG: triglycerides; WBC: white blood cell count.
The details of the echocardiographic analyses are shown in Table 2. IVST, LV PWT, LVM, LVM index and RWT were significantly higher in bodybuilders than in controls (p=0.019, p=0.025, p=0.006, p=0.01 and p=0.022, respectively). Also, RV, RA and PASP were greater in bodybuilders. No significant differences were found in aortic root diameter, LA end-diastolic, LVEDD, LVESD, or LVEF among the groups. Transmitral Doppler echocardiography showed lower E/A ratios in bodybuilders than in control subjects.
Echocardiographic findings in the study population.
| Controls (n=35) | Bodybuilders (n=35) | p | |
|---|---|---|---|
| ARD, mm | 25.51±0.47 | 24.98±0.41 | 0.399 |
| LAD, mm | 32.4±0.64 | 33.79±0.49 | 0.697 |
| IVST, mm | 8.99±0.15 | 9.73±0.21 | 0.019 |
| LVPW, mm | 8.84±0.14 | 9.49±0.19 | 0.025 |
| LVM, g | 134.06±4.16 | 154.94±6.02 | 0.006 |
| LVM index, g/m2 | 71.20±1.94 | 80.09±2.76 | 0.010 |
| RWT | 0.393±0.01 | 0.425±0.01 | 0.022 |
| LVEDD, mm | 45.39±0.63 | 45.89±0.74 | 0.609 |
| LVESD, mm | 33.74±5.67 | 29.56±0.76 | 0.197 |
| RAD, mm | 35.1±0.60 | 36.86±0.64 | 0.049 |
| RVEDD, mm | 33.39±0.73 | 35.89±0.76 | 0.021 |
| PSAP, mmHg | 19.09±1.19 | 21.94±0.85 | 0.045 |
| LVEF, % | 66.4±0.61 | 67.14±0.61 | 0.637 |
| E/A ratio | 2.09±0.18 | 2.84±0.25 | 0.023 |
ARD: aortic root diameter; IVST: intraventricular septal thickness; LAD: left atrial diameter; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; LVESD: left ventricular end-systolic diameter; LVM: left ventricular mass; LVPW: left ventricular posterior wall; PASP: pulmonary artery systolic pressure; RAD: right atrial diameter; RVEDD: right ventricular end-diastolic diameter; RWT: relative wall thickness.
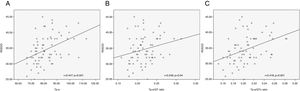
The results of 24-h Holter recordings and electrocardiographic parameters are shown in Table 3. PVCs and APCs were encountered significantly more frequently in bodybuilders than in the control group. QT and QTc were not significantly different between the groups. Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio were significantly greater in bodybuilders than in controls (p<0.001 for all) (Figure 1). QRS duration was not statistically different between the groups. PVCs and APCs were significantly more frequent in bodybuilders compared with controls (p=0.024 and p<0.001, respectively). No atrial fibrillation was detected in 24-h Holter recordings of any of the participants but non-sustained VT was demonstrated in two bodybuilders (p=0.493).
Myocardial repolarization parameters and arrhythmias in the study population.
| Controls (n=35) | Bodybuilders (n=35) | p | |
|---|---|---|---|
| Tp-e, ms | 76.58±1.07 | 87.47±1.76 | <0.001 |
| Tp-e/QT ratio | 0.202±0.004 | 0.235±0.005 | <0.001 |
| Tp-e/QTc ratio | 0.190±0.003 | 0.223±0.005 | <0.001 |
| QT, ms | 380.54±4.10 | 373.13±4.60 | 0.233 |
| QTc, ms | 405.20±3.86 | 393.83±4.34 | 0.054 |
| PVCs, n | 3.43±0.74 | 132.17±108.90 | 0.031 |
| APCs, n | 39.66±24.01 | 231.46±140.58 | <0.001 |
APCs: atrial premature complexes; PVCs: premature ventricular complexes; QTc: corrected QT dispersion; Tp-e: interval between the peak and the end of the T wave.
Spearman's correlation analysis revealed positive correlations between RV end-diastolic diameter and Tp-e interval (r=0.447; p<0.001), Tp-e/QT ratio (r=0.246; p=0.04), and Tp-e/QTc ratio (r=0.418; p<0.001) (Figure 2). Positive correlations were also demonstrated between PVCs and Tp-e interval (r=0.312; p=0.009), Tp-e/QT ratio (r=0.345; p=0.003), Tp-e/QTc ratio (r=0.259; p=0.03), and between APCs and Tp-e interval (r=0.261; p=0.029), Tp-e/QT ratio (r=0.239; p=0.047), and Tp-e/QTc ratio (r=0.264; p=0.027). However, there was no correlation between LA diameter, IVST, PWT, LV mass, LVM index, RWT, LVEDV, LVESV or LVEF and Tp-e, Tp-e/QT ratio, or Tp-e/QTc ratio (Figure 1).
DiscussionIn the present study, we showed that PVCs and APCs identified by Holter recordings were more frequent in bodybuilders, and that indices of repolarization dispersion on the ECG (Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio) were higher. This suggests that there may be a link between strength training and VAs and SCD. The positive correlation found between the presence of VAs and changes in these new parameters of repolarization variability is significant because these new indices have greater potential for prediction of arrhythmic risk in this population than the simple measurement of QT or QTc.
PVCs occur in 1-4% of healthy non-athletic subjects undergoing 24-h ambulatory ECG monitoring.15 In healthy athletes, PVCs seem to occur with the same frequency as in the general population,23 although some authors report a higher prevalence in athletes than in controls.14 It is known that exercise has both risks and benefits for ventricular ectopy and can induce or prevent arrhythmias, depending on dose and intensity.24 There is evidence that intense exercise may promote PVCs or non-sustained VT, and can lead to SCD in athletes.25 Strenuous exercise may be associated with adverse electrical and structural remodeling in otherwise normal hearts.26,27
Biffi et al.28 studied 355 athletes with VAs ranging from frequent PVCs to non-sustained VT on 24-h ambulatory ECG monitoring; none of the athletes with a structurally normal heart suffered any adverse cardiac events over an eight-year follow-up. Heidbuchel et al.26 observed a high incidence of major arrhythmic events (39%) including sudden cardiac death (20%) among 46 young athletes who presented with frequent PVCs or non-sustained VT during a five-year follow-up.29 PVCs may be an early manifestation of a concealed evolving heart disease at risk of SCD.30 The prognosis of truly idiopathic VAs is benign. However, a small percentage of individuals with frequent VAs may develop left ventricular dysfunction over time31 and rare reports have documented cardiac arrest and polymorphic VT.32,33
Moreover, in athletes, some arrhythmias may be secondary to a shift in autonomic modulation from parasympathetic to sympathetic during exercise, which could stimulate adrenergic receptors, mediating increases in cellular concentrations of cyclic adenosine monophosphate.30,34,35 Autonomic regulation could be an important factor in VAs in for athletes, as seen in catecholaminergic polymorphic VT, an inherited malignant arrhythmia syndrome provoked by increased sympathetic activity and presenting with exercise- or stress-related polymorphic VAs in young patients with structurally normal hearts.36
On the other hand, LA fibrosis may play a key role in the generation of supraventricular arrhythmias.37 Vigorous exercise may lead to myocardial fibrosis that manifests as cardiac dysfunction and arrhythmias. Also, both decreases in refractory period and slowed conduction due to vagally-mediated shortening of the excitation wave length facilitate reentry.38 A meta-analysis of six studies involving 655 athletes engaging in diverse sporting disciplines reported a five-fold increase in risk of AF compared to controls.39
Our results revealed that PVCs and APCs were significantly more frequent in bodybuilders. Non-sustained VT occurred in two athletes, without statistical significance. Also, no AF was encountered in our study. Management of PVCs in the athletic population is complex because they may be a sign of an underlying heart disease. According to the current recommendations, an annual reassessment should be considered in athletes with suspect findings.26,40
While the ECG is an essential tool for the initial investigation of athletes with PVCs, echocardiography is an important diagnostic exam for detecting myocardial abnormalities, since the information it gives on the structures of the heart may provide insight into the origin of arrhythmias.
The increased cardiac preload and afterload resulting from chronic intensive exercise is associated with symmetrical enlargement of all cardiac chambers.5 A study of 1300 Italian athletes competing in endurance sports demonstrated markedly enlarged LV and LA diameters but little increase in LV wall thickness.41 Bodybuilding principally involves high static (isometric) and low dynamic (isotonic) exercise that mainly induces pressure load.3 Echocardiographic studies show that strength-trained athletes (including weightlifters, power lifters and bodybuilders) have increased LV wall thickness similar to the concentric hypertrophy observed in chronic pressure overload.42,43 The results of a meta-analysis by Pluim et al.44 show that strength-trained athletes, who were thought to develop purely concentric LV hypertrophy, in fact demonstrated an increase in both absolute and relative wall thickness and calculated cardiac mass. Moreover, no significant difference in LV diameter has been reported between strength-trained athletes and heavy controls.45–47 Both IVST and PWT are 15-20% greater in trained athletes than in age- and gender-matched untrained controls.46,48,49 However, these thicknesses in athletes are most often within the normal range. Prospective studies of exercise training demonstrate that endurance training increases LV internal dimensions with little change in LV wall thickness.50 By contrast, strength exercise training increases LV wall thickness with little effect on LV cavity dimensions.44 Our results were in agreement with previous findings that IVST, LV PWT, LVM, LVM index and RWT are significantly higher in bodybuilders than in controls, but within normal ranges. No significant differences were found in LA end-diastolic, LVEDD, LVESD, or LVEF between our study groups. A few studies have suggested that exercise training increases aortic diameter,51,52 but no such difference between groups was demonstrated in our results.
However, our analysis also showed that RV and RA dimensions and PASP were greater in bodybuilders. Modest increases in RV dimensions have been reported in strength-trained athletes.53 High-intensity static exercise may contribute to increased PASP and reduction in RV systolic function.54 Very few studies have examined RA size in endurance-trained athletes, but those that are available also demonstrate larger RA dimensions than in age- and gender-matched strength athletes and controls.55 Athletes show a 10-15% increase in right ventricular cavity size compared with non-athlete individuals of similar age and size.56
The mechanisms underlying the reported arrhythmias in athletes are unknown, but there is a suggestion that strenuous exercise may cause fibrosis (scarring), which acts as a substrate for generating arrhythmias.57 Evidence from animal models tends to support this theory. Benito et al. studied cardiac changes in rats exercising on a treadmill.58 At 16 weeks, which in human terms is equivalent to 10 years, exercising rats developed eccentric LV hypertrophy, diastolic dysfunction, and diffuse fibrosis in the atria and right ventricle. More importantly, VT during electrophysiological studies was inducible in 42% of these rats compared with only 6% in sedentary rats.56 Similarly, Venlet et al.59 recently described a novel clinical entity of an isolated subepicardial right ventricular outflow tract scar serving as a substrate for fast VT in endurance athletes that can be successfully treated by ablation.
Nonetheless, Verdile et al.17 and Delise et al.,60 investigating populations of competitive athletes without detectable cardiovascular abnormalities, found that PVCs had a right ventricular outflow tract morphology on the ECG. In a study of 40 athletes, it was shown that chronic exercise promotes right ventricular remodeling and 80% of VAs were of RV origin.61 In a recent study, Zaidi et al.62 found that over 40% of male athletes exhibit RV dimensions exceeding the upper limits of normal for the general population, raising the suspicion of arrhythmogenic right ventricular cardiomyopathy (ARVC). Similarly, La Gerche et al.63 studied 40 healthy athletes at baseline and after an endurance race and observed transient RV enlargement associated with impaired RV function on echocardiography. The authors postulated that consistent prolonged and intensive endurance exercise may lead to irreversible RV remodeling with a propensity to fatal arrhythmias, which has led to the concept of exercise-induced ARVC. Both studies require confirmation, but are consistent with the concept that exercise training increases RV dimensions and that this enlargement stresses myocardial junctions, producing cellular damage and structural changes in the right ventricle which mimic ARVC.
Acute increases in PASP with exercise are greater than increases in systemic arterial pressure.64 Likewise, we can postulate on the basis of our results that strength training produces relatively greater increases in RV than in LV wall stress, particularly in bodybuilders. Hence, it may be a substrate for VAs in bodybuilders.
Myocardial repolarization has been assessed by various parameters including QT interval, QTc, and transmural dispersion of repolarization. Several studies indicate that prolonged QT and QTc are associated with VAs and SCD without any structural cardiac changes.65 Previous studies also demonstrated that QT and QTc were normal in training-induced LV hypertrophy in both young and older athletes.66,67 Similarly, we found no difference in QT or QTc between bodybuilders and controls.
Studies have indicated that Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio can be used as indices of total (transmural, apicobasal, and global) dispersion of repolarization9,10 and hence as an electrocardiographic marker of risk for VAs and SCD.11,12,68 It has been shown that Tp-e interval and Tp-e/QT ratio are associated with increased risk for malignant VAs in a variety of conditions12,69,70 and are increased in LV hypertrophy.18,70 A recent study revealed that Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio were significantly prolonged with steroid use in bodybuilders.18 However, in a study by Braschi et al.,71 athlete's heart was not associated with any alteration in ventricular repolarization, and physiologic adaptive LV hypertrophy did not affect the duration of Tp-e interval or the Tp-e/QT ratio. In our study population, Tp-e, Tp-e/QT ratio, and Tp-e/QTc ratio were prolonged in bodybuilders.
In conclusion, it is challenging to predict the outcome in athletes with PVCs based on noninvasive investigations, and in this population, it may be difficult to categorize remodeling as adaptive or pathological by echocardiographic measurements.72–74 Prolonged repolarizations are common in athletes, although their predictive value is unclear. In our study, alterations in ventricular repolarization were positively correlated with RV dimensions, thus we postulate that arrhythmias in strength athletes may be predicted by assessing the right ventricle echocardiographically and dispersions of repolarization on the ECG, and that malign VAs and SCD could be avoided in strength athletes by careful application of this information. The prognostic utility of these indices requires confirmation in future studies for more consistent results.
Study limitationsOur sample size was limited, and the study's cross-sectional design meant we could not examine the clinical implications of the parameters assessed in strength training athletes. Further well-designed studies with a longer follow-up are needed in a larger number of subjects to study malignant arrhythmias. Only younger male individuals were studied. Thus, female and older athletes, including retired individuals, should be assessed to confirm the results of this noninvasive analysis.
Conflicts of interestThe authors have no conflicts of interest to declare.