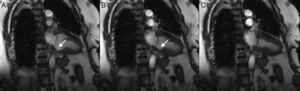
We present the case of an 84‐year‐old woman admitted for Takotsubo cardiomyopathy complicated by congestive heart failure. Cardiovascular magnetic resonance (CMR) imaging was performed on day five and confirmed severely depressed left ventricular systolic function with typical apical ballooning. In steady‐state free precession long‐axis cine imaging, a basal inferior myocardial cleft was also observed, with no signs of myocardial noncompaction or regional wall motion abnormalities involving this segment. The pre‐discharge CMR study confirmed the presence of a basal inferior myocardial cleft and significant improvement in left ventricular systolic function.
Myocardial clefts are congenital abnormalities that have been described in healthy individuals as well as in the setting of hypertrophic cardiomyopathy, but it is not clear whether it is a benign structural variant or a distinct cardiomyopathy phenotype. To our knowledge this is the first reported case of this abnormality in a patient with Takotsubo cardiomyopathy.
Apresentamos o caso de uma mulher de 84 anos de idade admitida por cardiomiopatia de Takotsubo, complicada com insuficiência cardíaca. Realizou ressonância magnética cardíaca (RMC) ao quinto dia de internamento que confirmou a presença de disfunção sistólica grave do ventrículo esquerdo e imagem típica de balonamento apical. Foi também visualizada uma fenda miocárdica no ventrículo esquerdo com localização ínfero‐basal, sem sinais de não‐compactação miocárdica associada ou alterações da motilidade envolvendo este segmento. A RMC pré‐alta confirmou a presença da referida fenda miocárdica e uma melhoria significativa da função sistólica ventricular esquerda.
As fendas miocárdicas são anomalias congénitas que têm sido descritas em indivíduos saudáveis, assim como, no contexto da cardiomiopatia hipertrófica, não estando ainda esclarecido se será uma variante do normal ou um fenótipo associado a cardiomiopatia. Segundo o nosso conhecimento este é o primeiro caso descrito de uma fenda miocárdica num doente com cardiomiopatia de Takotsubo.
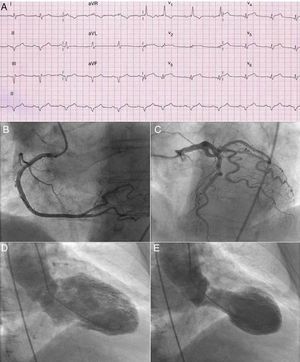
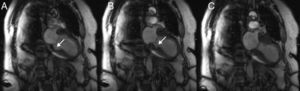
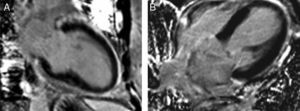
An 84‐year‐old overweight Caucasian woman, with arterial hypertension, presented to the emergency room with chest pain radiating to both arms and back. The patient denied any recent emotionally or physically stressful event. The admission ECG showed sinus rhythm, right bundle branch block, ST‐segment elevation in the anterior leads (1 mm) and Q waves in the inferior leads (Figure 1A). Due to suspicion of an acute anterior myocardial infarction, emergent coronary angiography was performed, which revealed no significant obstructive lesions (Figure 1B and C); ventriculography disclosed moderately to severely depressed left ventricular (LV) systolic function and marked apical ballooning with basal hyperkinesia (Figure 1D and E). A diagnosis of Takotsubo cardiomyopathy was presumed. The patient was admitted to the intensive cardiac care unit with congestive heart failure and was managed with diuretics, a beta‐blocker, an angiotensin‐converting enzyme inhibitor and anticoagulation with low molecular weight heparin. Laboratory data showed an increase in troponin I (peak 6.3 ng/ml) and brain natriuretic peptide (peak 2305 pg/ml). Cardiovascular magnetic resonance (CMR) imaging was performed on day five and confirmed severely depressed LV systolic function with mid‐apical akinesia of the LV chamber. Unexpectedly, in steady‐state free precession long‐axis cine imaging, a basal inferior myocardial cleft was also observed (Figure 2). There were no signs of myocardial noncompaction or regional wall motion abnormalities involving this segment. After administration of gadolinium no myocardial delayed enhancement was observed (Figure 3), which further substantiated the diagnosis of Takotsubo cardiomyopathy. The patient recovered and was discharged home on day 15, maintaining the same medical treatment. The pre‐discharge CMR study confirmed the presence of a basal inferior myocardial cleft and recovery of LV systolic function (Figure 4).
Left ventricular vertical long‐axis steady‐state free precession cardiac magnetic resonance cine images at end‐diastole (A), mid‐systole (B) and end‐systole (C) demonstrates akinesia of the mid‐apical segments of the left ventricle. A myocardial cleft (arrows) in the basal inferior segment was also observed, which was completely obliterated during end‐systole.
Alterations in myocardial structure frequently overlooked in the past can nowadays become apparent with the increasing use of multislice computed tomography and CMR for evaluation of the coronary arteries and cardiac structures. LV clefts are recently reported structural abnormalities of the left ventricle discovered incidentally during cross‐sectional diagnostic imaging procedures. They have been the focus of attention due to the possibility that they are associated with hypertrophic cardiomyopathy (HCM), having been initially described in post‐mortem hearts of patients with HCM1; later, in a study by Germans et al.2 among HCM mutation carriers, 81% had evidence of clefts, prompting the speculation that LV clefts might precede manifest hypertrophy. However, Johansson et al.3 reported that myocardial clefts in the LV basal inferior wall and the interventricular septum in CMR studies are not confined to HCM patients, but are also found in healthy individuals and are associated with other clinical entities including hypertension and congenital heart disease (although genetic analysis for HCM carrier mutations was not performed). They defined clefts as discrete V‐shaped extensions of blood signal penetrating >50% of the thickness of adjoining compact myocardium in long‐axis views, that tend to narrow or occlude in systole, without local hypokinesia or dyskinesia.
This congenital structural variant of the myocardium is thought to be a result of myocardial fiber disarray in typical regions of LV (commonly seen in the interventricular septum and LV inferior wall) and possibly due to focal fissuring between circularly oriented myocardial muscle fascicles.4
Although the majority of authors consider it probable that LV clefts have no prognostic significance,5 a prospective study to clarify the clinical importance of these structures would be helpful. To our knowledge this is the first reported case of this abnormality in a patient with Takotsubo cardiomyopathy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.