Congenital pericardial defects are extremely rare with a reported incidence of <1 in 10000 and a male:female ratio of 3:1. Most patients are asymptomatic and diagnosis is usually incidental. Symptomatic patients present a range of non-specific symptoms, meaning that imaging is crucial for diagnosis.
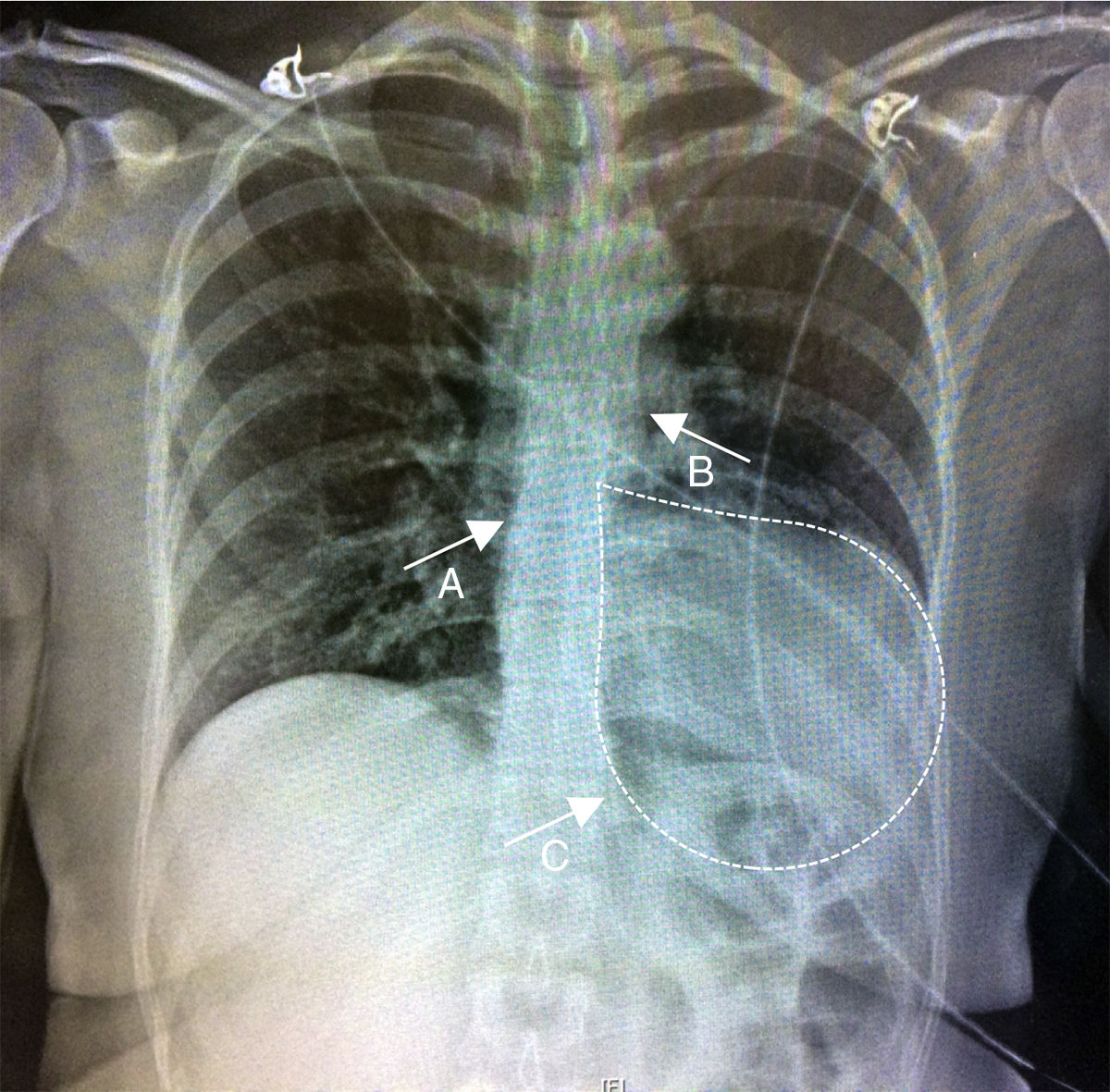
A 46-year-old woman was referred to our department with symptoms of palpitations and atypical chest pain. Clinical examination found a palpable apical impulse on the midaxillary line. Electrocardiogram revealed sinus rhythm with a heart rate of 90 bpm, left anterior fascicular block and incomplete right bundle branch block. Chest X-ray (Figure 1) revealed levoposition and a “teardrop” appearance of the heart, superimposition of the right cardiac border over the spine, a prominent main pulmonary artery and a translucent area between the heart and the diaphragm.
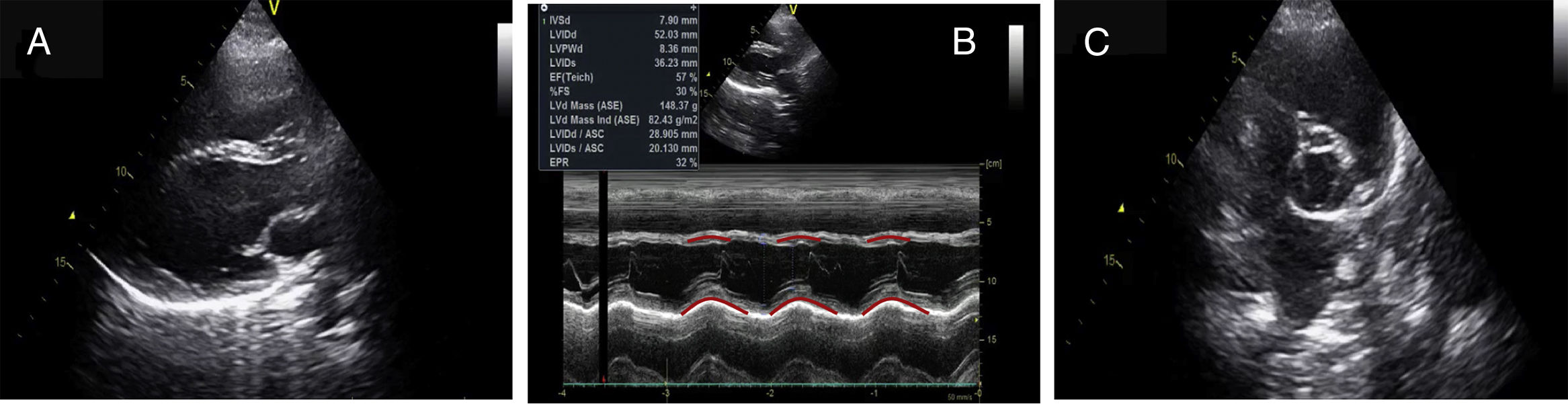
Unusual transthoracic echocardiographic windows were required, which showed paradoxical ventricular septal motion, cardiac hypermobility and apparent right ventricular dilation (Figure 2).
Systemic-to-pulmonary shunt, arrhythmogenic cardiomyopathy and congenital pericardial defect were considered as possible diagnoses.
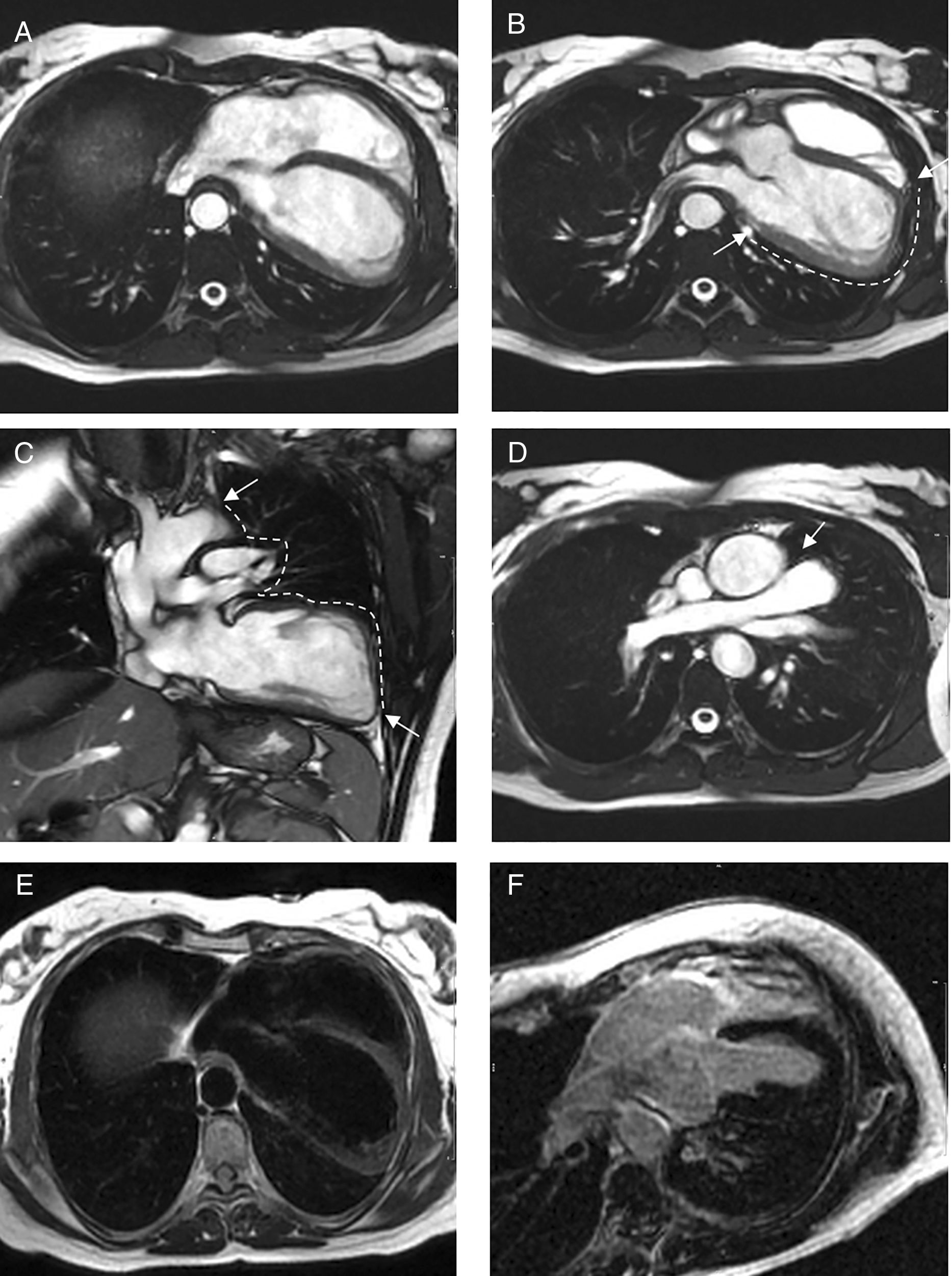
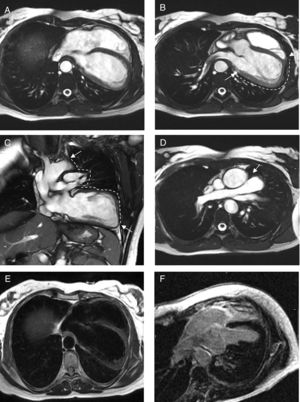
As the echocardiographic images were suboptimal, cardiac magnetic resonance imaging (MRI) was performed (Figure 3), confirming leftward displacement of the heart (Figure 3A) and hypermobility (Video 1). Absence of left ventricular pericardium and pericardial fat (Figure 3B and C) and interposition of lung tissue between the great vessels (Figure 3D) were also observed. This last finding is considered a specific diagnostic sign (for some authors even a pathognomonic sign) of congenital pericardial defect.
Cardiac MRI images. (A-D) Steady-state free precession images. (A) Axial image showing left and posterior heart displacement. (B) Axial image displaying non-visualization of the pericardium and pericardial fat around the left ventricle (between the white arrows). (C) Coronal image showing absence of the pericardium and pericardial fat around the left ventricle and great vessels (between the white arrows), with lung tissue interposition in the several recesses where the pericardium is usually found. (D) Axial image showing lung tissue in the aorto-pulmonary window (white arrow), which is considered a pathognomonic sign of this condition. (E) T1-weighted axial image with no abnormalities, particularly, fat tissue deposition. (F) Delayed gadolinium-enhanced axial image with no macroscopic areas of myocardial fibrosis/necrosis.
Therefore, our patient was diagnosed with complete defect of the left pericardium, which is the most common type described in the literature. As it is a form with good prognosis, no treatment was given and the patient was kept under regular follow-up.
Conflicts of interestThe authors have no conflicts of interest to declare.