Left main disease (LMD) has historically been treated by coronary artery bypass grafting (CABG) due to the large area of myocardium at risk and procedural challenges for percutaneous coronary intervention (PCI). However, with progressive advances in recent decades, PCI has proved to be a valid alternative in selected cases. In this context, first-generation drug-eluting stents (DES) were compared with CABG in four randomized trials (RCTs): SYNTAX1 (n=705), PRECOMBAT (n=600), LE MANS (n=105) and Boudriot et al. (n=201). SYNTAX is arguably the landmark study in this setting. The first all-comers trial, it introduced the concept of coronary disease complexity,2 and later, patient complexity,3 as potential predictors of outcomes, although the impact of the SYNTAX score (SS) on outcomes was not confirmed in later RCTs. In the pre-specified LMD subgroup analysis at five years,4 SYNTAX revealed no differences between PCI and CABG in major adverse cardiac and cerebrovascular events (MACCEs), mortality or myocardial infarction (MI), although it was not powered for isolated adverse events. It suggested that CABG had lower MACCE rates than PCI only in the highest SS tertile, ≥33. As the SYNTAX trial did not confirm the hypothesis of PCI non-inferiority in the overall population, its LMD SS subgroup findings were hypothesis-generating only.1
The development of second-generation DES with lower stent thrombosis rates, and the lack of statistical power in previous trials, prompted the next LMD RCTs: EXCEL5 (n=1905) and NOBLE6 (n=1201), both with the mission to finally determine whether PCI was non-inferior to CABG in patients with LMD and low or intermediate SS.
Five-year results of the EXCEL and NOBLE trialsAt five years, the EXCEL trial showed CABG to be non-superior to PCI, with 22.0% having the primary composite endpoint of death, stroke or MI in the PCI group vs. 19.2% for CABG (95% confidence interval [CI], 0.9%-6.5%; p=0.13).7 All-cause mortality was higher in the PCI group at five years (13.0% vs. 9.9%; odds ratio [OR], 1.38; 95% CI, 1.03-1.85). Ischemia-driven revascularization, which was not included in the composite primary outcome, was also higher in the PCI group (16.9% vs. 6.9%; OR, 1.84; 95% CI, 1.39-2.44).7
At five years, the NOBLE trial revealed a significantly higher incidence of the primary composite outcome of death, stroke, spontaneous MI and revascularization in the PCI group (29% vs. 19%; p=0.0002). All-cause mortality was similar between the two groups (36% vs. 33%) but the total repeat revascularization rate (17% vs. 10%; p=0.0009) and non-procedural MI (8% vs. 3%; p=0.0002) favored CABG.8
These divergent results may be explained by pivotal differences between the two trials, summarized in Table 1, and methodological issues as detailed below.
Main differences between the EXCEL and NOBLE trials.
| Variable | EXCEL | NOBLE |
|---|---|---|
| Primary composite endpoint | Death, any MI (including periprocedural) and stroke, but not repeat revascularization | Death, only spontaneous MI, stroke and repeat revascularization |
| MI definition | New definition based on CK-MB with equal thresholds for CABG and PCI | Third Universal Definition of MI |
| Patient population | More diabetic patients (29% vs. 15%)Excluded patients with SS>32 (although on core lab analysis 25% had SS>32) | Fewer diabetic patients (15% vs. 29%)Excluded patients with more than 3 lesions or a complex additional lesion (chronic total occlusion, bifurcation lesion requiring two-stent techniques or lesion with calcified or tortuous vessel morphology) |
| Devices used | Only everolimus-eluting stents (second-generation) | Biolimus-eluting stent (second generation) and first-generation DES in 11% of cases |
| Sponsors | Abbott Vascular | Aarhus University Hospital (main sponsor)Biosensors (institutional research grant) |
DES: drug-eluting stent; MI: myocardial infarction; SS: SYNTAX score.
The EXCEL controversy was sparked when the head of the surgical committee, Prof. D. Taggart of Oxford University, decided to remove his name from the list of authors because the main paper in the New England Journal of Medicine (NEJM) failed to report an analysis of MI according to the Universal Definition of Myocardial Infarction and, despite an all-cause mortality benefit of 3.1% with CABG, the authors concluded that CABG was not superior to PCI. Trial data leaked to the BBC showed a significantly higher rate of all MI in the PCI group, raising doubts concerning the non-inferiority conclusion, and led the European Association for Cardio-Thoracic Surgery (EACTS) to withdraw its support for the recommendations for treatment of LMD in the 2018 European Society of Cardiology/EACTS myocardial revascularization guidelines.9
So, what are the main sources for this bitter controversy?
All-cause mortality in EXCELAlthough all-cause mortality was a secondary endpoint, unadjusted for multiple comparisons, there was a significant gap of 3.1% (13.0% in PCI and 9.9% in CABG; OR, 1.38; 95% CI, 1.03-1.85) in all-cause mortality at five years in favor of CABG. This was considered by the EXCEL authors to be due to chance alone,10 based on the absence of a significant difference in cardiovascular mortality. However, it should be borne in mind that the adjudication process, i.e. determining the causes of death, in a non-blinded trial, can be subject to ascertainment and misclassification biases. The two most recent meta-analyses of all LMD PCI vs. CABG RCTs showed no statistically significant difference in mortality.11,12 However, if the results of EXCEL and NOBLE are pooled, there is a higher risk of death for PCI and therefore the question remains unresolved.13
Definition of myocardial infarction in EXCELThe EXCEL protocol defining postprocedural MI used the same CK-MB thresholds for CABG and PCI (>10× upper reference limit [URL] in isolation or >5× URL with new Q waves or other confirmation of ischemia, as published by the Society for Cardiovascular Angiography and Interventions [SCAI]).14 It is well known that CABG is associated with the release of myocardial biomarkers due to aortic clamping and cardiac manipulation. This definition differs from those used in previous trials comparing PCI with CABG and has been shown to overestimate MI after CABG compared to other definitions. Cho et al. showed a substantial difference in the rates of periprocedural MI after PCI and CABG, depending on the MI definition used: 18.7% vs. 2.9% using the Second Universal Definition; 3.2% vs. 1.9% by the Third Universal Definition; and 5.5% vs. 18.3% by the SCAI definition.15 The use of the SCAI definition may have affected the primary endpoint and may explain why five-year MI rates in the CABG arm of the EXCEL trial7 (9.1%) are two to five times higher than in other LMD trials: 4.8% in SYNTAX,4 1.7% in PRECOMBAT and 3% in NOBLE.8 In a post-hoc analysis, Gaudino et al.16 showed that if the unpublished, but prespecified, universal definition had been used for procedural MI in EXCEL, the five-year composite endpoint would have demonstrated clear superiority of CABG (OR, 1.40; 95% CI, 1.09-1.81; p=0.009).
In the original trial protocol,17 and in successive versions (all including the Universal Definition as one definition of MI), the EXCEL investigators left the trial's specific MI definition open. The protocol defining MI was only published in 2016,5 using the SCAI definition,14 two months before the three-year results were published in the NEJM,18 which is most unusual. Finally, in the five-year results the EXCEL investigators failed to include the data on MI according to the prespecified secondary endpoint using the Second Universal Definition.
In a recent letter to the Editor of the NEJM,19 the EXCEL leaders reported that the large discrepancy between the two definitions in the number of CABG-related procedural myocardial infarctions (57 by the protocol definition vs. 13 by the universal definition) was mostly due to a lack of confirmatory evidence of myocardial ischemia that is required in the universal definition. However, reanalysis of the primary outcome using the protocol-prespecified Second Universal Definition is still unpublished.
The NOBLE trial8 appears to be less controversial, although critics have pointed out some flaws. An interim change of protocol, including primary outcomes reported and follow-up, due to lower-than-expected rates of MACCE, put the trial's internal validation at risk. The use of 11% first-generation along with second-generation (89%) DES may have influenced the PCI results, as the rate of stent thrombosis was significantly higher in NOBLE than in EXCEL (3% vs. 0.7%). Additionally, the inclusion of repeat revascularization in the composite endpoint may be debatable, since it is considered to be less clinically important compared to death, MI or stroke, although both SYNTAX1 and PRECOMBAT also included it in the composite endpoint.
Meaningful versus statistical differences?The EXCEL investigators concluded that there was no statistically significant difference between PCI and CABG in the primary outcome at five years (difference, 2.8%; 95% CI, 0.9-6.5%). However, the 95% CI interval for the difference in MACCE rates between PCI and CABG is wide, ranging from 0.9% to 6.5%, mostly above 0%, favoring CABG. Importantly, there is an increasing gap over time between the two treatments after the second year in Kaplan-Meier curves of the primary endpoint, diverging in favor of CABG.
EXCEL was designed as a non-inferiority trial, and the three-year results were reported with an agreed margin of non-inferiority of 4.2%.5,18 If the protocol-defined, non-inferiority type of analysis, as reported at three years, had also been used for the five-year report, PCI was not non-inferior to CABG, as the 6.5% upper bound of the confidence interval would have exceeded the non-inferiority margin of 4.2%.
To whom do these results apply?In all trials, results are only valid for populations with the same anatomical and clinical characteristics, the same techniques and expertise used in the selected centers. Extrapolation of trial results to wider, real-world populations could miss the target in a large proportion of patients, with potentially unpredictable outcomes. NOBLE and EXCEL7,8 included relatively young patients (around 66 years), with low comorbidity and favorable anatomical and clinical characteristics for both procedures. To put this in perspective, of the 2905 patients with >50% left main stenosis initially screened in EXCEL, only 1905 were randomized. The other 1000 patients were included in registries. Non-eligibility criteria included coronary disease that was considered too extensive (269/995; 27%) or too complex for PCI (317/995; 32%) and in 18% (183/999), specific coronary lesion characteristics or patient characteristics prevented randomization to CABG. This means that more than 30% (1000/2905) of patients with LMD were not represented in EXCEL. Worryingly, this issue of the external validity of RCTs, the backbone of translational and evidence-based medicine, is still, unforgivably, lacking in the guidelines.
SummaryOverall, PCI for LMS is associated with fewer early complications, less pain, shorter hospital stays and faster return to normal activity than CABG. Interpreting trial data requires an understanding of methodological issues that is not readily available to the busy clinician. At five-year follow up, the absolute magnitude of the differences in mortality appears to be small, favoring CABG, depending on which trials are pooled. The composite of death/stroke/MI depends on the definition of MI and the duration of follow-up. However, PCI is associated with significantly higher MI and repeat revascularization rates.
As the guidelines are based on findings from RCTs, there is an urgent need for more transparency through confirmatory, independent, analysis of trial databases.
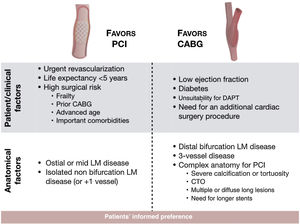
Decision-making hinges on trial results, but also on patient characteristics such as life expectancy, LM anatomy, disease extent, left ventricular function, and the presence of diabetes or other comorbidities, as well as operator proficiency (Figure 1). The best decision for an individual patient is achieved through inputs from patients, interventional cardiologists, surgeons, imaging specialists and clinical cardiologists.20 Although medical societies may support diverging opinions on clinical grounds, consensus is being built every day, in well-functioning heart teams, in patients’ best interests.
Conflicts of interestThe authors have no conflicts of interest to declare.