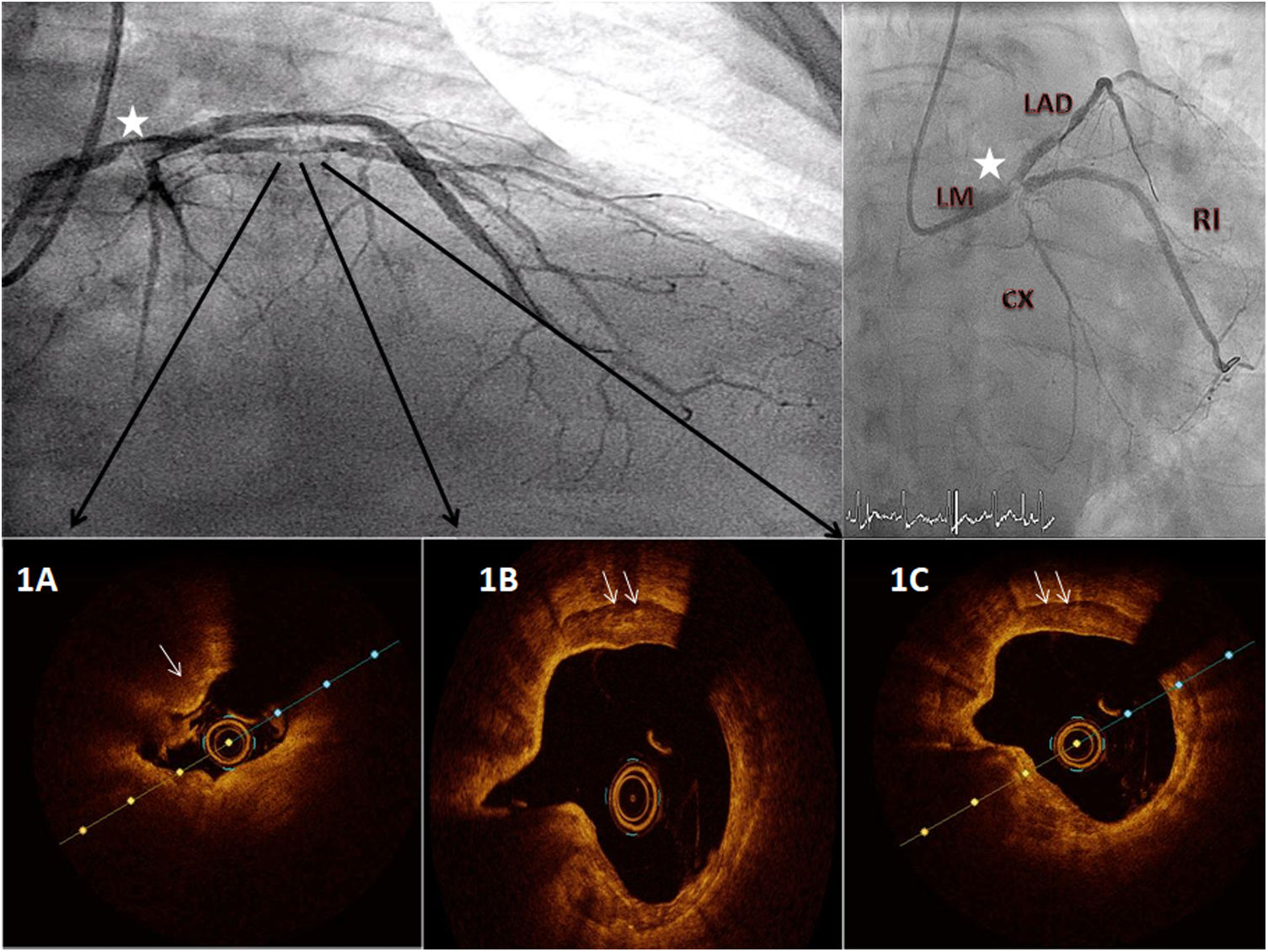
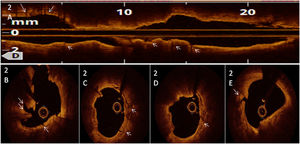
A 63-year old man was admitted with a diagnosis of non-ST elevation myocardial infarction. Electrocardiogram showed generalized ST depression but isolated ST elevation in aVR. Echocardiogram showed normal left ventricular ejection fraction with no wall motion abnormalities but severe pulmonary hypertension. Diagnostic angiography demonstrated a severe, heavily calcified lesion in the distal left main (LM) artery (Figure 1, star) with significant stenosis in proximal left anterior descending artery (LAD) and ramus intermedius (RI) (Medina 1-1-1). Baseline optical coherence tomography (OCT) revealed a >180° calcium arc (Figure 1B-C, arrows) coupled to calcified nodules (Figure 1A, arrow), leading to an almost occlusive reduction in lumen area in proximal LAD (Figure 1A). Percutaneous revascularization was chosen after discussion by the heart team and intracoronary lithotripsy was planned.
Baseline angiogram and optical coherence tomography (OCT) evaluation. A severe, calcified lesion is seen in distal left main artery (star) with severe stenosis over left anterior descending artery (LAD) and ramus intermedius. OCT images reveal a calcium arc >180° with calcium nodules over proximal LAD (f=Figure 1A).
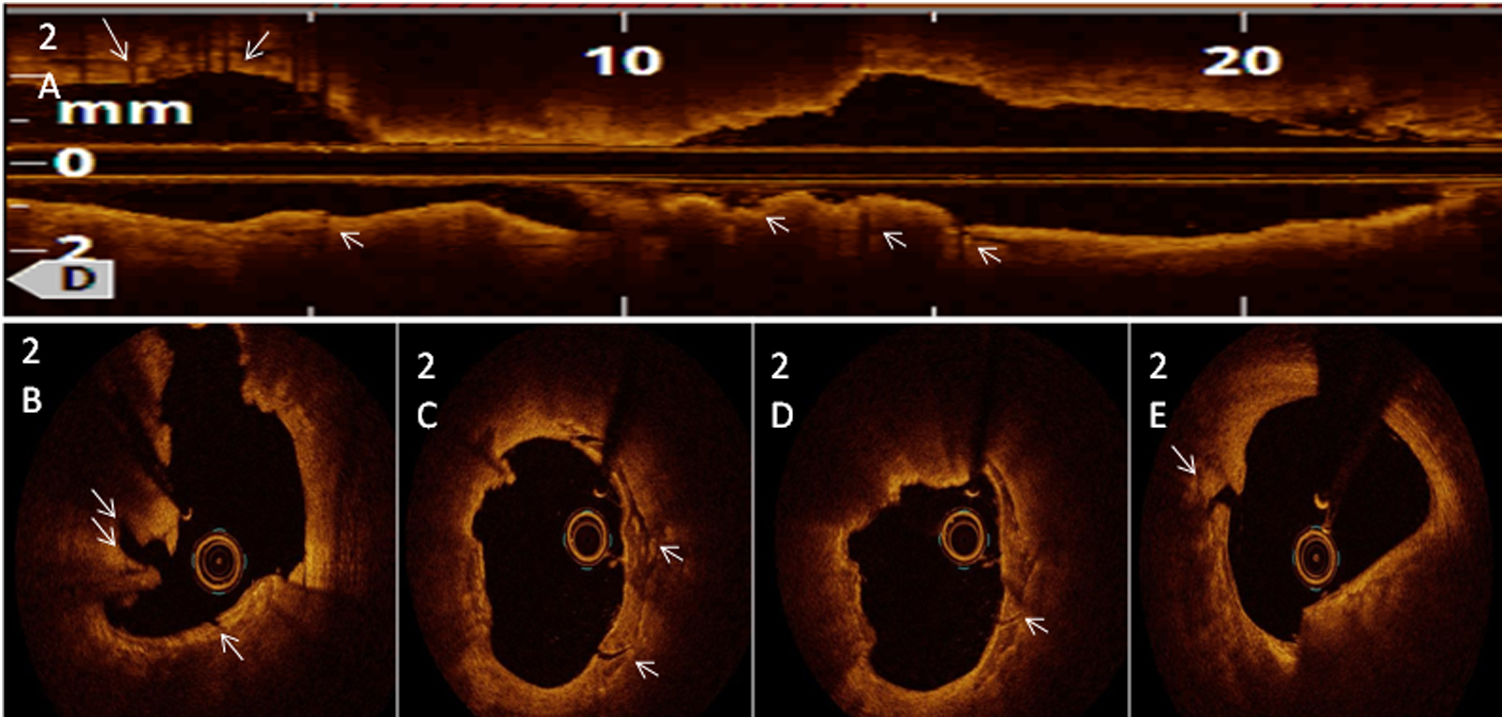
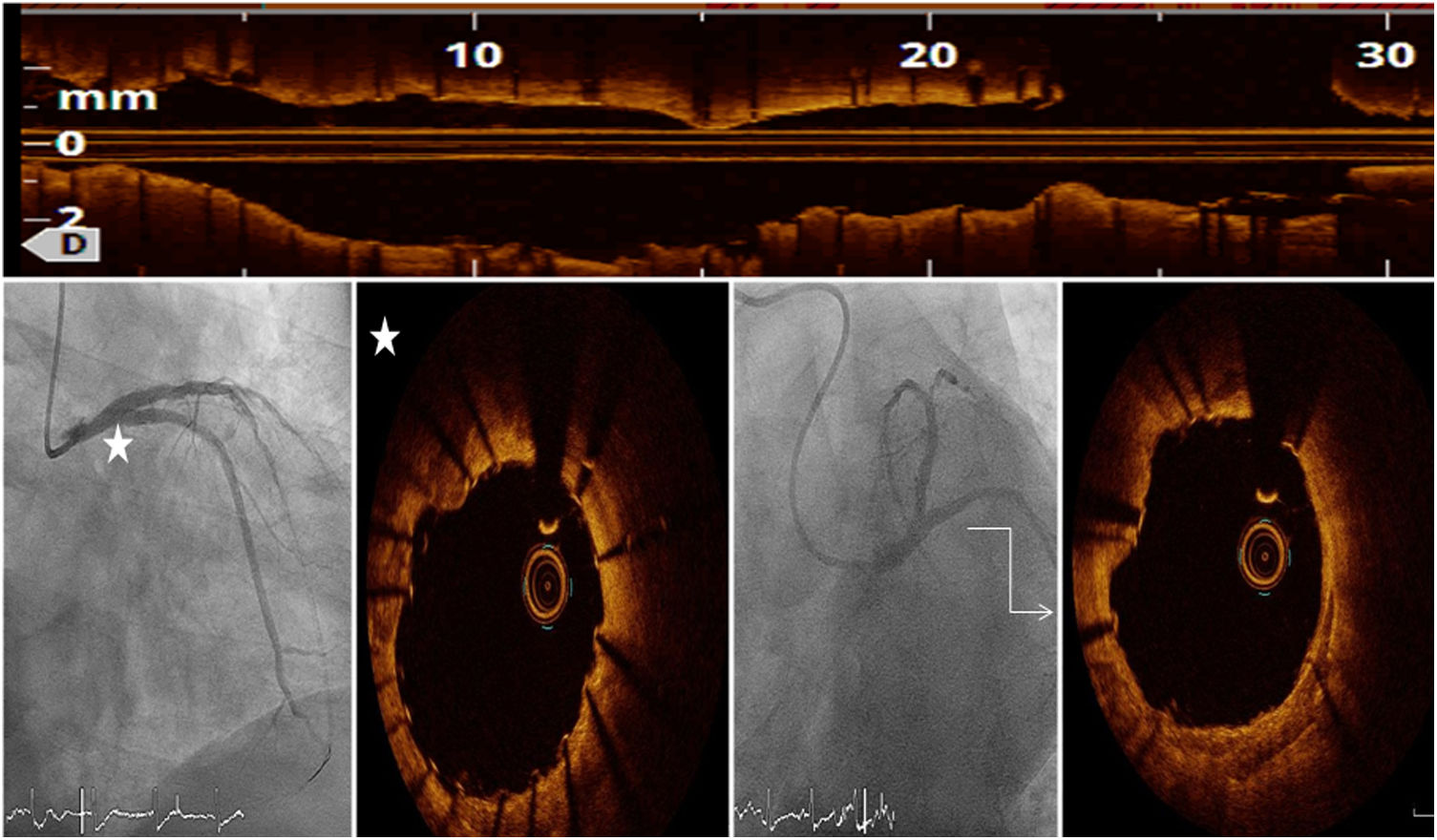
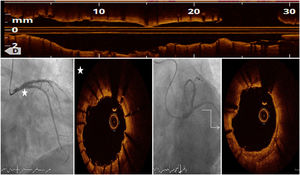
After predilatation with small semi-compliant balloon, we crossed a 3.5×12 mm Shockwave® lithotripsy balloon to proximal LAD and RI lesions. Ten sonic wave pulses were delivered at four atmospheres in both lesions, followed by another 50 pulses in LAD and 10 more pulses in RI. A second Shockwave® balloon of 4×12 mm was placed over distal LM and 80 pulses were applied. No hemodynamic impairment developed. Optical coherence tomography images showed aggressive plaque modification with transverse, deep fractures (Figure 2A, arrows) both over the calcium arc (Figure 2C-E) and nodules (Figure 2B). A culotte technique was chosen for LM percutaneous coronary intervention. Post-procedure OCT (Figure 3) and intravascular ultrasound demonstrated optimal stent expansion and apposition, with no residual dissections.
Although evidence is still scarce, with this case we support OCT-guided intravascular lithotripsy in LM percutaneous coronary intervention as a reliable debulking technique which improves the outcome.
Conflicts of interestThe authors have no conflicts of interest to declare.