Myocardial infarction is very rare in children. It can have different etiologies such as thromboembolism caused by nephrotic syndrome (NS).
We report the case of a 15 year old boy with NS, diagnosed at the age of 7 year, admitted for prolonged chest pain. The final diagnosis was ST-elevation myocardial infarction with thromboembolism in the left anterior descending artery due to hypercoagulability of NS.
This association is very uncommon and the management of both conditions presents a challenge.
O enfarte do miocárdio (EM) é raro nas crianças. Pode ter etiologias diferentes, tais como o tromboembolismo causado por síndrome nefrótico (SN).
Apresentamos o caso de um rapaz de 15 anos com SN, diagnosticado desde os sete anos e admitido por dor torácica prolongada. O diagnóstico final foi de enfarte do miocárdio com elevação do segmento ST com tromboembolismo na descendente anterior esquerda (DAE) devido a hipercoagulabilidade do SN.
Essa associação é muito incomum e o tratamento de ambas as situações representa um desafio.
Myocardial infarction (MI) is very rare in children and can have different etiologies. Unlike older patients, in whom atherosclerotic disease is the main underlying disease, the pathogenesis in younger patients can be varied. One such etiology is thromboembolism caused by nephrotic syndrome (NS). We present a case of MI in a young male with history of NS.
Case reportA previously healthy young 15 old male developed NS at the age of seven. He was brought to the pediatric department of our center where the diagnosis of minimal change disease was made based on the kidney biopsy. He was treated with steroids to which he responded. Later, he developed steroid-dependent nephrotic syndrome, frequently relapsing, for which he was put on short courses of steroids followed by maintenance and subsequently combined with calcineurin inhibitors plus enalapril.
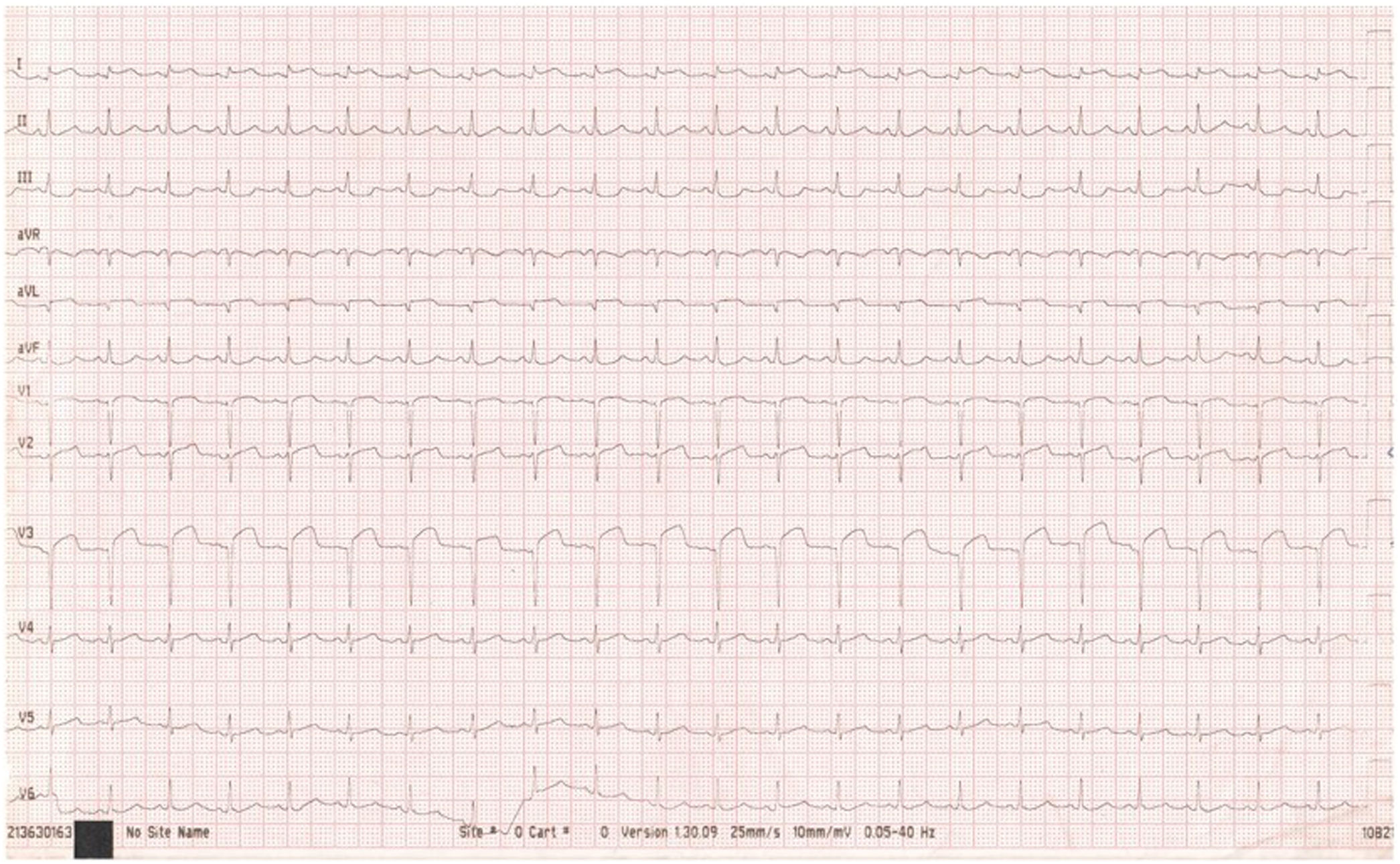
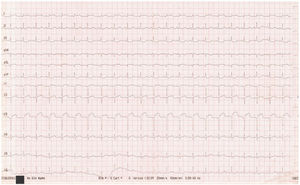
He presented to the emergency department in April 2017 with a sudden onset of severe and prolonged retrosternal chest pain radiating to the left arm. He did not have any smoking, alcohol or drug use habits. There was no history of diabetes, hypertension, hepatitis B, malignant tumor or connective tissue disease. Moreover, there was no family history of thrombophilia or premature coronary artery disease. At the time of presentation, the patient was in a stable hemodynamic condition. His blood pressure was 120/70 mmHg, his pulse was 105 beats per minute, and his body temperature was 36.7°C. He had facial and peripheral oedema. Heart, lung, and abdominal examinations were normal. The electrocardiogram (ECG) showed typical ST-segment elevation and pathological Q waves in the anterior and lateral leads (Figure 1). The patient was treated for ST-segment elevation MI (STEMI). He received antithrombotic treatment with clopidogrel, aspirin and enoxaparin. The echocardiography revealed a reduced left ventricular ejection fraction (LVEF) to 40%. There was severe left ventricular anterior and antero-septal wall hypokinesia. The blood tests revealed elevated cardiac troponin I (71ng/mL). Further biochemical analyses showed the following: platelets 619×109/L, serum creatinine 26 μmol/L, blood urea nitrogen 3.4 mmol/L, albumin 18 g/dL, total cholesterol (CT) 11.04 mmol/L, low-density lipoprotein cholesterol (LDL-C) 8.2 mmol/L, high-density lipoprotein cholesterol (HDL-C) 0.98 mmol/L, and triglyceride 4.8 mmol/L. Fibrogen plasma concentration was elevated (7 g/L). Anti-thrombin III levels, protein C and protein S activity were normal. Twenty-four hours of urine analysis showed that albuminuria was 4 g/24 h. Antistreptolysin O, antinuclear antibodies/anti-double stranded DNA, antiphospholipid antibodies and anti-beta-2 glycoprotein were negative.
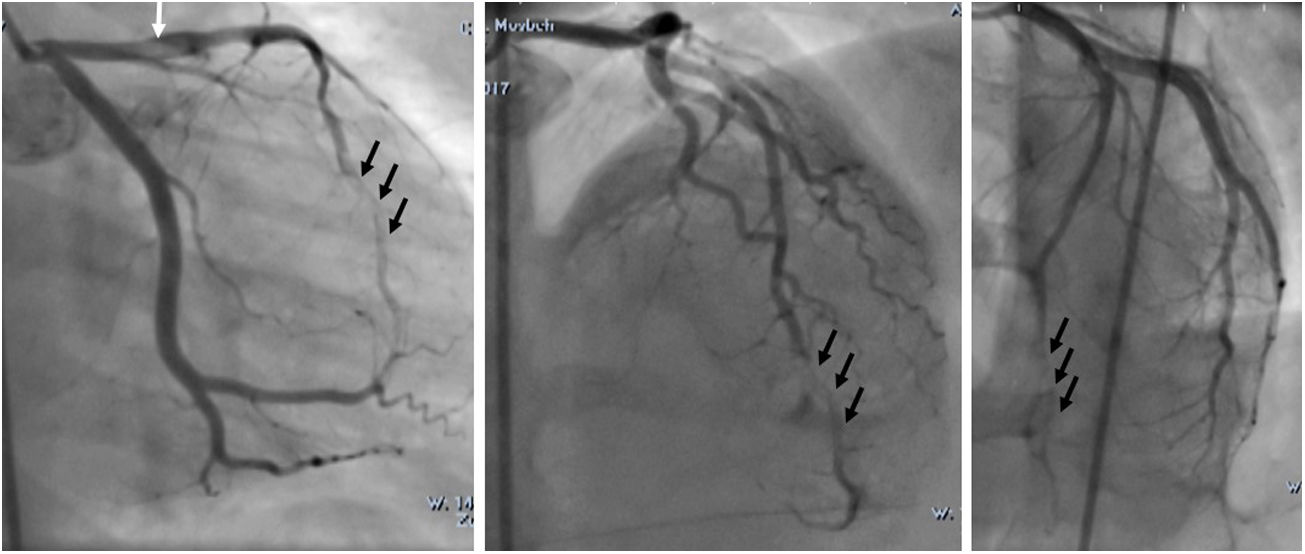
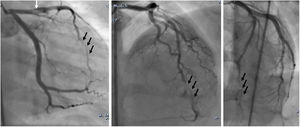
An emergency coronary angiography (CAG) was performed at admission, eight hours after chest pain onset and showed a massive thrombosis of the left anterior descending artery (LAD) with thrombolysis in myocardial infarction II flow (Figure 2). Tirofiban was injected into the LAD for thrombolysis during the CAG procedure.
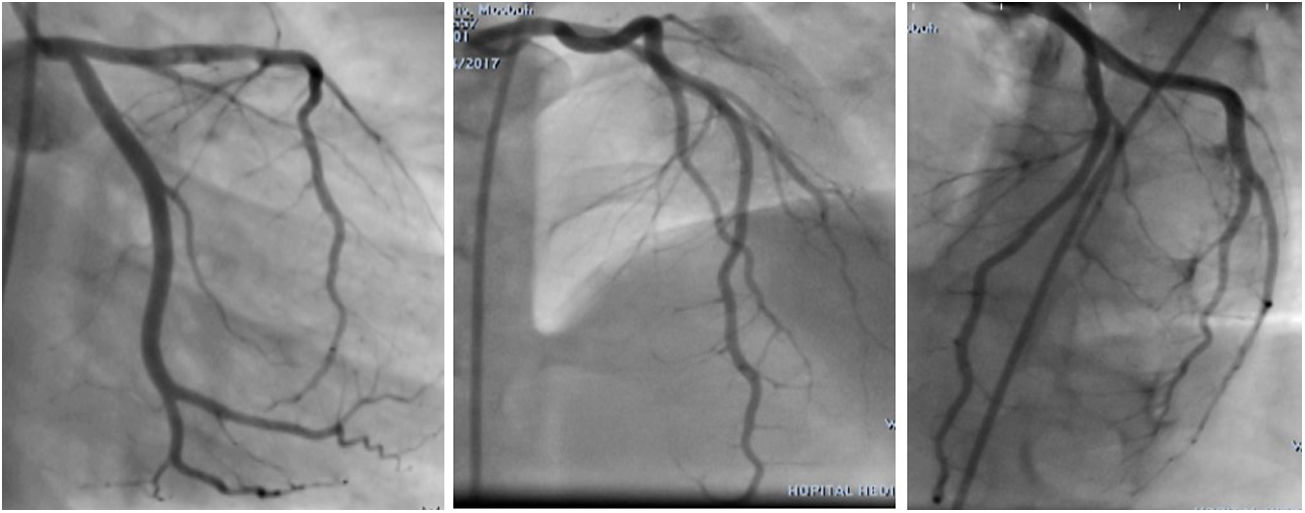
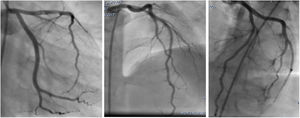
The final diagnosis was STEMI with thromboembolism in the LAD. The patient continued to receive antithrombotic medication (aspirin, clopidogrel, tirofiban and heparin), nitrates, statins, diuretics, beta blockers, and a high dose of prednisolone to treat his decompensated NS. A CAG, performed after 7 days, revealed normal coronary artery flow and no more thrombosis (Figure 3). The patient was discharged after eight days in a stable hemodynamic condition. He was followed up by the pediatrician for immunosuppressive therapy. He continued to be stable and asymptomatic at 12-month follow-up. Echocardiogram revealed LVEF was 53%, which was better than before.
DiscussionThe thromboembolic complications associated with NS are seen in 35% of patients.1 However, arterial thromboses are much less common, being observed in only 1.8-5%,2 making the disease's prognosis more serious, especially when they affect vital organs. The risk of MI is multiplied by eight in patients with NS.3 MI can be classified into two different categories: It may be due to coronary artery thrombosis, embolism, spasm or a combination of these; Another condition is abnormal coronary arteries, including significant accelerated atherosclerosis due to chronic dyslipidemia and the high level of inflammatory factors in patients with NS.4
In our case, NS is considered the cause of thrombotic occlusion of the coronary arteries, leading to STEMI. Coronary thrombosis was confirmed by CAG at admission, eight hours after chest pain onset and treated with Intracoronary thrombolysis plus tirofiban. The time between nephrotic syndrome findings and onset of MI was eight years in this case. The causes of acute MI in this patient may be due to a hypercoagulative state including, increases in factors V, VIII, and X, increased fibrinogen and platelet levels, increased adhesion and aggregation of platelets, decreases in factors IX and XI and decreased activity of anti-thrombin-III and anti-plasmin, leading to thromboembolic events even in intact arteries.5 Furthermore, long-term steroid therapy can promote and aggravate thrombosis. The angiographic control performed seven days after onset of MI showed a complete thrombus dissolving after antithrombotic therapy. This suggests the role of antiplatelets and anticoagulant treatment in acelerating physiologic thrombolysis in a hypercoagulative state such as NS. In most reported cases of thromboembolic events in NS, treatment with high dose heparin with or without thrombolytic agents has been found to be effective in dissolving thrombus.6 The optimal therapeutic interventions depend on the patient's hemodynamic status, the region of lesion, and the number of vessels involved. Various treatment modalities have been attempted, including interventional procedures, such as percutaneous coronary intervention and coronary artery bypass graft, which have been proven successful for critical or multivessel dissection cases.4 Furthermore, conservative medical treatment with antiplatelets, thrombolytics and nitroglycerin could also be efficient.
For these patients, long-term anticoagulant therapy is therefore particularly important. This also suggests the role of long term prophylactic anticoagulation in children with steroid-resistant NS. Although there are no prospective studies improving this role, some authors recommend prophylactic use of warfarin or aspirin in high-risk patients with plasma albumin
In conclusion, children with severe hypoalbuminemia are at increased risk of thrombosis, so they should be treated and carefully observed to reduce its occurrence. Furthermore, for all children with acute chest pain and ST segment elevation on the ECG, clinicians should pay greater attention. In fact, young patients can have acute coronary events in the absence of atherosclerotic disease and the possibility of underlying NS should be always considered.
Conflicts of interestThe authors have no conflicts of interest to declare.