We discuss the case of a 49-year-old patient with left ventricular systolic dysfunction and a large, mobile and protruding apical thrombus. In spite of anticoagulation treatment, extensive and clearly defined systemic embolization occurred.
We discuss the current evidence on the treatment of intracardiac thrombus with high risk of systemic embolization and propose a tailored approach to avoid potential catastrophic consequences.
Apresentamos o caso de um doente de 49 anos com disfunção sistólica ventricular esquerda e um trombo apical de grandes dimensões, móvel e com protrusão para a cavidade ventricular. Apesar do tratamento anticoagulante, ocorreram vários fenómenos de embolização sistémica, extensos e muito ilustrativos.
Discutimos a evidência atual sobre o tratamento de trombos intracardíacos com alto risco de embolização sistémica e propomos uma reflexão sobre uma abordagem personalizada para evitar potenciais consequências catastróficas.
We present the case of a 49-year-old male, a smoker, with type 2 diabetes mellitus, hypertension, dyslipidemia, stage 3 renal failure and atrial fibrillation (AF). He had been recently diagnosed with probable tachycardiomyopathy, because of fluctuating degrees of left ventricular systolic dysfunction in the context of poorly controlled AF, in the absence of coronary artery disease.
He was admitted with rapid AF and decompensated heart failure. In terms of AF treatment, he was taking bisoprolol, digoxin and warfarin, but his international normalized ratio was subtherapeutic.
He was started on parenteral anticoagulation, but shortly after admission he developed left hemiparesis, pain in the lower limbs and abdominal pain.
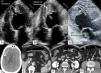
The echocardiogram showed moderate left ventricular (LV) systolic impairment and a massive mobile thrombus in the LV apex (Figure 1A and B) and another in the left atrium (Figure 1C).
(A) Transthoracic echocardiogram, apical 4-chamber view in diastole, showing apical LV thrombus; (B) transthoracic echocardiogram, apical 4-chamber view in systole, showing the thrombus protruding into the LV cavity; (C) transthoracic echocardiogram, apical 3-chamber view, showing the LV and LA thrombi; (D) cerebral computed tomography, displaying a large cerebral infarct; (E–G) abdominal computed tomography with contrast, showing splenic (E) and renal (F) infarcts and almost total occlusion of the infrarenal abdominal aorta (G). LA: left atrial; LV: left ventricular.
Computed tomography confirmed multiple cerebral (Figure 1D), splenic (Figure 1E) and renal (Figure 1F) infarcts, as well as an almost total occlusion of the infrarenal abdominal aorta (Figure 1G), distal to the origin of the inferior mesenteric artery.
He was referred for emergent thrombectomy for removal of the aortic thrombus and continued anticoagulation, with favorable recovery.
This is a catastrophic case of intracardiac thrombus with massive systemic emboli. It is a reminder of the dangerous association between atrial fibrillation and left ventricular systolic impairment, highlighting the importance of adequate anticoagulation in these patients.
It also prompts reflection on the lack of treatment options available for patients when a large mobile protruding thrombus is already present and there is a substantial risk for systemic embolic phenomena, even with anticoagulation treatment. Surgical thrombectomy1,2 may be considered, especially if there are recurrent emboli despite anticoagulation and if the thrombus remains large, but it also carries a very high risk.
Some weeks later, another patient was admitted to our center with a history of ischemic heart disease and decompensated heart failure. She had a very large, apparently pedunculated and protruding LV thrombus. Medical and surgical treatment options were discussed, but her surgical risk was felt to be very high and she was started on anticoagulation, maintaining clinical stability. After a week, when she was about to be discharged, a transthoracic echocardiogram was repeated, which no longer showed any intracardiac thrombus. A few hours later, she suddenly died of a massive stroke.
In conclusion, handling patients with a large intracardiac thrombus, particularly when located in the left cardiac chambers and clearly fresh, mobile and pedunculated, is often problematic. In these circumstances, to start anticoagulation and hope for the best feels quite insufficient.
In the few observational studies available to date, 10–15% of patients with an LV thrombus (most of them after myocardial infarction) suffered a significant embolic event, especially in the first 3–4 months,3 and anticoagulation was associated with a significant reduction in the occurrence of embolization.4,5 However, not all thrombi are the same. In particular, thrombus mobility and protrusion have been associated with a higher embolization risk, of approximately 60%.3,6
Since large, protruding, fresh thrombi are relatively rare, there are no studies that specifically address this problem. The few published case reports and observational studies of thrombus with these characteristics that were treated with a surgical approach showed successful results2,7,8 and perhaps this option should be considered more often.
Other options could also be explored, such as the development of a percutaneous device to temporarily contain the thrombus in the apex and facilitate aspiration, or some other option that increases the odds for a positive outcome.
We hope that further research will be performed in this area and that it will be possible to offer a better treatment strategy for high-risk intracardiac thrombus.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.